Abstract
Background
Cardiovascular diseases are currently the commonest cause of death worldwide. Different strategies for their primary prevention have been planned, taking into account the main known risk factors, which include an atherogenic lipid profile and visceral fat excess.
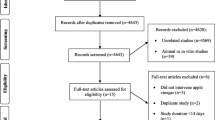
Methods
The study was designed as a randomized, parallel, single-center study with a nutritional intervention duration of 12 weeks. Whole soy foods corresponding to 30 g/day soy protein were given in substitution of animal foods containing the same protein amount.
Results
Soy nutritional intervention resulted in a reduction in the number of MetS features in 13/26 subjects. Moreover, in the soy group we observed a significant improvement of median percentage changes for body weight (−1.5 %) and BMI (−1.5 %), as well as for atherogenic lipid markers, namely TC (−4.85 %), LDL-C (−5.25 %), non-HDL-C (−7.14 %) and apoB (−14.8 %). Since the majority of the studied variables were strongly correlated, three factors were identified which explained the majority (52 %) of the total variance in the whole data set. Among them, factor 1, which loaded lipid and adipose variables, explained the 22 % of total variance, showing a statistically significant difference between treatment arms (p = 0.002).
Conclusions
The inclusion of whole soy foods (corresponding to 30 g/day protein) in a lipid-lowering diet significantly improved a relevant set of biomarkers associated with cardiovascular risk.




Similar content being viewed by others
Abbreviations
- apoB:
-
Apolipoprotein B
- apoA-I:
-
Apolipoprotein A-I
- BMI:
-
Body mass index
- BIA:
-
Bioelectrical impedance analysis
- CRP:
-
High-sensitivity C-reactive protein
- CVD:
-
Cardiovascular diseases
- DBP:
-
Diastolic blood pressure
- FPG:
-
Fasting plasma glucose
- HC:
-
Hip circumference
- HDL-C:
-
High-density lipoprotein cholesterol
- HOMA:
-
Homeostatic model assessment
- HR:
-
Heart rate
- LDL-C:
-
Low-density lipoprotein cholesterol
- Lp(a):
-
Lipoprotein (a)
- N:
-
Number
- PCSK9:
-
Proprotein convertase subtilisin/kexin 9
- SBP:
-
Systolic blood pressure
- sICAM-1:
-
Soluble intercellular adhesion molecular 1
- TC:
-
Total cholesterol
- TG:
-
Triglycerides
- VFR:
-
Visceral fat rating
- WC:
-
Waist circumference
References
Organization WH (2015) Obesity and overweight. http://www.who.int/mediacentre/factsheets/fs311/en/
Oliveros E, Somers VK, Sochor O, Goel K, Lopez-Jimenez F (2014) The concept of normal weight obesity. Prog Cardiovasc Dis 56(4):426–433. doi:10.1016/j.pcad.2013.10.003
Ebbert JO, Jensen MD (2013) Fat depots, free fatty acids, and dyslipidemia. Nutrients 5(2):498–508. doi:10.3390/nu5020498
Scaglione R, Di Chiara T, Cariello T, Licata G (2010) Visceral obesity and metabolic syndrome: two faces of the same medal? Intern Emerg Med 5(2):111–119. doi:10.1007/s11739-009-0332-6
Mangge H, Almer G, Truschnig-Wilders M, Schmidt A, Gasser R, Fuchs D (2010) Inflammation, adiponectin, obesity and cardiovascular risk. Curr Med Chem 17(36):4511–4520
Nicklas BJ, Ambrosius W, Messier SP, Miller GD, Penninx BW, Loeser RF, Palla S, Bleecker E, Pahor M (2004) Diet-induced weight loss, exercise, and chronic inflammation in older, obese adults: a randomized controlled clinical trial. Am J Clin Nutr 79(4):544–551
Ferri N, Ruscica M (2016) Proprotein convertase subtilisin/kexin type 9 (PCSK9) and metabolic syndrome: insights on insulin resistance, inflammation, and atherogenic dyslipidemia. Endocrine. doi:10.1007/s12020-016-0939-0
Lagos KG, Filippatos TD, Tsimihodimos V, Gazi IF, Rizos C, Tselepis AD, Mikhailidis DP, Elisaf MS (2009) Alterations in the high density lipoprotein phenotype and HDL-associated enzymes in subjects with metabolic syndrome. Lipids 44(1):9–16. doi:10.1007/s11745-008-3251-9
Brown L, Poudyal H, Panchal SK (2015) Functional foods as potential therapeutic options for metabolic syndrome. Obes Rev 16(11):914–941. doi:10.1111/obr.12313
Ruscica M, Gomaraschi M, Mombelli G, Macchi C, Bosisio R, Pazzucconi F, Pavanello C, Calabresi L, Arnoldi A, Sirtori CR, Magni P (2014) Nutraceutical approach to moderate cardiometabolic risk: results of a randomized, double-blind and crossover study with Armolipid Plus. J Clin Lipidol 8(1):61–68. doi:10.1016/j.jacl.2013.11.003
van Nielen M, Feskens EJ, Rietman A, Siebelink E, Mensink M (2014) Partly replacing meat protein with soy protein alters insulin resistance and blood lipids in postmenopausal women with abdominal obesity. J Nutr 144(9):1423–1429. doi:10.3945/jn.114.193706
Rebello CJ, Greenway FL, Finley JW (2014) A review of the nutritional value of legumes and their effects on obesity and its related co-morbidities. Obes Rev 15(5):392–407. doi:10.1111/obr.12144
Harland JI, Haffner TA (2008) Systematic review, meta-analysis and regression of randomised controlled trials reporting an association between an intake of circa 25 g soya protein per day and blood cholesterol. Atherosclerosis 200(1):13–27. doi:10.1016/j.atherosclerosis.2008.04.006
Anderson JW, Bush HM (2011) Soy protein effects on serum lipoproteins: a quality assessment and meta-analysis of randomized, controlled studies. J Am Coll Nutr 30(2):79–91
Sirtori CR, Agradi E, Conti F, Mantero O, Gatti E (1977) Soybean-protein diet in the treatment of type-II hyperlipoproteinaemia. Lancet 1(8006):275–277
Sirtori CR, Eberini I, Arnoldi A (2007) Hypocholesterolaemic effects of soya proteins: results of recent studies are predictable from the Anderson meta-analysis data. Br J Nutr 97(5):816–822. doi:10.1017/S0007114507670810
Jenkins DJ, Mirrahimi A, Srichaikul K, Berryman CE, Wang L, Carleton A, Abdulnour S, Sievenpiper JL, Kendall CW, Kris-Etherton PM (2010) Soy protein reduces serum cholesterol by both intrinsic and food displacement mechanisms. J Nutr 140(12):2302S–2311S. doi:10.3945/jn.110.124958
Allison DB, Gadbury G, Schwartz LG, Murugesan R, Kraker JL, Heshka S, Fontaine KR, Heymsfield SB (2003) A novel soy-based meal replacement formula for weight loss among obese individuals: a randomized controlled clinical trial. Eur J Clin Nutr 57(4):514–522. doi:10.1038/sj.ejcn.1601587
Velasquez MT, Bhathena SJ (2007) Role of dietary soy protein in obesity. Int J Med Sci 4(2):72–82
Takahira M, Noda K, Fukushima M, Zhang B, Mitsutake R, Uehara Y, Ogawa M, Kakuma T, Saku K (2011) Randomized, double-blind, controlled, comparative trial of formula food containing soy protein vs. milk protein in visceral fat obesity-FLAVO study. Circ J 75(9):2235–2243
Rebholz CM, Reynolds K, Wofford MR, Chen J, Kelly TN, Mei H, Whelton PK, He J (2013) Effect of soybean protein on novel cardiovascular disease risk factors: a randomized controlled trial. Eur J Clin Nutr 67(1):58–63. doi:10.1038/ejcn.2012.186
Mozaffarian D (2016) Dietary and policy priorities for cardiovascular disease, diabetes, and obesity: a comprehensive review. Circulation 133(2):187–225. doi:10.1161/CIRCULATIONAHA.115.018585
Reinwald S, Weaver CM (2010) Soy components vs. whole soy: are we betting our bones on a long shot? J Nutr 140(12):2312S–2317S. doi:10.3945/jn.110.124008
Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, Fruchart JC, James WP, Loria CM, Smith SC Jr (2009) International Diabetes Federation Task Force on E, Prevention, Hational Heart L, Blood I, American Heart A, World Heart F, International Atherosclerosis S, International Association for the Study of O. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation 120(16):1640–1645. doi:10.1161/CIRCULATIONAHA.109.192644
Schutz Y, Sarafian D, Miles JL, Montani JP, Dulloo AG (2012) Non-contact assessment of waist circumference: will tape measurements become progressively obsolete? Eur J Clin Nutr 66(2):269–272. doi:10.1038/ejcn.2011.183
Thomas EL, Collins AL, McCarthy J, Fitzpatrick J, Durighel G, Goldstone AP, Bell JD (2010) Estimation of abdominal fat compartments by bioelectrical impedance: the validity of the ViScan measurement system in comparison with MRI. Eur J Clin Nutr 64(5):525–533. doi:10.1038/ejcn.2010.18
Manios Y, Kanellakis S, Moschonis G, Pipidis I, Skoufas E, Zafiropulos V (2013) Estimation of abdominal fat mass: validity of abdominal bioelectrical impedance analysis and a new model based on anthropometry compared with dual-energy x-ray absorptiometry. Menopause 20(12):1280–1283. doi:10.1097/GME.0b013e31828f5cd8
Estruch R, Ros E, Martinez-Gonzalez MA (2013) Mediterranean diet for primary prevention of cardiovascular disease. N Engl J Med 369(7):676–677. doi:10.1056/NEJMc1306659
Sniderman A, Williams K, de Graaf J (2010) Non-HDL C equals apolipoprotein B: except when it does not! Curr Opin Lipidol 21(6):518–524. doi:10.1097/MOL.0b013e32833ee80c
Ruscica M, Macchi C, Gandini S, Morlotti B, Erzegovesi S, Bellodi L, Magni P (2016) Free and bound plasma leptin in anorexia nervosa patients during a refeeding program. Endocrine 51(2):380–383. doi:10.1007/s12020-015-0598-6
Ruscica M, Ferri N, Macchi C, Meroni M, Lanti C, Ricci C, Maggioni M, Fracanzani AL, Badiali S, Fargion S, Magni P, Valenti L, Dongiovanni P (2016) Liver fat accumulation is associated with circulating PCSK9. Ann Med 48(5):384–391. doi:10.1080/07853890.2016.1188328
Franceschini G, Calabresi L, Colombo C, Favari E, Bernini F, Sirtori CR (2007) Effects of fenofibrate and simvastatin on HDL-related biomarkers in low-HDL patients. Atherosclerosis 195(2):385–391. doi:10.1016/j.atherosclerosis.2006.10.017
Favari E, Gomaraschi M, Zanotti I, Bernini F, Lee-Rueckert M, Kovanen PT, Sirtori CR, Franceschini G, Calabresi L (2007) A unique protease-sensitive high density lipoprotein particle containing the apolipoprotein A-I(Milano) dimer effectively promotes ATP-binding cassette A1-mediated cell cholesterol efflux. J Biol Chem 282(8):5125–5132. doi:10.1074/jbc.M609336200
Locati D, Morandi S, Cupisti A, Ghiadoni L, Arnoldi A (2005) Characterization and quantification of soy isoflavone metabolites in serum of renal transplanted patients by high-performance liquid chromatography/electrospray ionization mass spectrometry. Rapid Commun Mass Spectrom 19(23):3473–3481. doi:10.1002/rcm.2222
Nakamura Y, Okuda N, Okamura T, Kadota A, Miyagawa N, Hayakawa T, Kita Y, Fujiyoshi A, Nagai M, Takashima N, Ohkubo T, Miura K, Okayama A, Ueshima H, Group NDR (2014) Low-carbohydrate diets and cardiovascular and total mortality in Japanese: a 29-year follow-up of NIPPON DATA80. Br J Nutr 112(6):916–924. doi:10.1017/S0007114514001627
Assmann G, Buono P, Daniele A, Della Valle E, Farinaro E, Ferns G, Krogh V, Kromhout D, Masana L, Merino J, Misciagna G, Panico S, Riccardi G, Rivellese AA, Rozza F, Salvatore F, Salvatore V, Stranges S, Trevisan M, Trimarco B, Vetrani C (2014) Functional foods and cardiometabolic diseases* international task force for prevention of cardiometabolic diseases. Nutr Metab Cardiovasc Dis 24(12):1272–1300. doi:10.1016/j.numecd.2014.10.010
Sirtori CR, Galli C, Anderson JW, Arnoldi A (2009) Nutritional and nutraceutical approaches to dyslipidemia and atherosclerosis prevention: focus on dietary proteins. Atherosclerosis 203(1):8–17. doi:10.1016/j.atherosclerosis.2008.06.019
Stein K (2000) FDA approves health claim labeling for foods containing soy protein. J Am Diet Assoc 100(3):292. doi:10.1016/S0002-8223(00)00088-2
Ioannidis JP (2016) We need more randomized trials in nutrition-preferably large, long-term, and with negative results. Am J Clin Nutr 103(6):1385–1386. doi:10.3945/ajcn.116.136085
Lerman RH, Minich DM, Darland G, Lamb JJ, Chang JL, Hsi A, Bland JS, Tripp ML (2010) Subjects with elevated LDL cholesterol and metabolic syndrome benefit from supplementation with soy protein, phytosterols, hops rho iso-alpha acids, and Acacia nilotica proanthocyanidins. J Clin Lipidol 4(1):59–68. doi:10.1016/j.jacl.2009.11.002
Pischon T, Boeing H, Hoffmann K, Bergmann M, Schulze MB, Overvad K, van der Schouw YT, Spencer E, Moons KG, Tjonneland A, Halkjaer J, Jensen MK, Stegger J, Clavel-Chapelon F, Boutron-Ruault MC, Chajes V, Linseisen J, Kaaks R, Trichopoulou A, Trichopoulos D, Bamia C, Sieri S, Palli D, Tumino R, Vineis P, Panico S, Peeters PH, May AM, Bueno-de-Mesquita HB, van Duijnhoven FJ, Hallmans G, Weinehall L, Manjer J, Hedblad B, Lund E, Agudo A, Arriola L, Barricarte A, Navarro C, Martinez C, Quiros JR, Key T, Bingham S, Khaw KT, Boffetta P, Jenab M, Ferrari P, Riboli E (2008) General and abdominal adiposity and risk of death in Europe. N Engl J Med 359(20):2105–2120. doi:10.1056/NEJMoa0801891
Twig G, Yaniv G, Levine H, Leiba A, Goldberger N, Derazne E, Ben-Ami Shor D, Tzur D, Afek A, Shamiss A, Haklai Z, Kark JD (2016) Body-mass index in 2.3 Million adolescents and cardiovascular death in adulthood. N Engl J Med 374(25):2430–2440. doi:10.1056/NEJMoa1503840
Meigs JB (2000) Invited commentary: insulin resistance syndrome? Syndrome X? Multiple metabolic syndrome? A syndrome at all? Factor analysis reveals patterns in the fabric of correlated metabolic risk factors. Am J Epidemiol 152(10):908–911 (discussion 912)
Anderson JW, Hoie LH (2005) Weight loss and lipid changes with low-energy diets: comparator study of milk-based versus soy-based liquid meal replacement interventions. J Am Coll Nutr 24(3):210–216
Hodge AM, Boyko EJ, de Courten M, Zimmet PZ, Chitson P, Tuomilehto J, Alberti KG (2001) Leptin and other components of the metabolic syndrome in mauritius—a factor analysis. Int J Obes Relat Metab Disord 25(1):126–131
Moreno LA, Pineda I, Rodriguez G, Fleta J, Giner A, Juste MG, Sarria A, Bueno M (2002) Leptin and metabolic syndrome in obese and non-obese children. Horm Metab Res 34(7):394–399. doi:10.1055/s-2002-33472
Park HS, Lee MS, Park JY (2004) Leptin and the metabolic syndrome in Korean adolescents: factor analysis. Pediatr Int 46(6):697–703. doi:10.1111/j.1442-200x.2004.01984.x
Zhang XM, Zhang YB, Chi MH (2016) Soy protein supplementation reduces clinical indices in type 2 diabetes and metabolic syndrome. Yonsei Med J 57(3):681–689. doi:10.3349/ymj.2016.57.3.681
Morandi S, Locati D, Ferrario F, Chiesa G, Arnoldi A (2005) A simple method for the characterization and quantification of soy isoflavone metabolites in the serum of MMTV-Neu mice using high-performance liquid chromatography/electrospray ionization mass spectrometry with multiple reaction monitoring. Rapid Commun Mass Spectrom 19(2):153–161. doi:10.1002/rcm.1760
Richelle M, Pridmore-Merten S, Bodenstab S, Enslen M, Offord EA (2002) Hydrolysis of isoflavone glycosides to aglycones by beta-glycosidase does not alter plasma and urine isoflavone pharmacokinetics in postmenopausal women. J Nutr 132(9):2587–2592
Zheng Y, Hu J, Murphy PA, Alekel DL, Franke WD, Hendrich S (2003) Rapid gut transit time and slow fecal isoflavone disappearance phenotype are associated with greater genistein bioavailability in women. J Nutr 133(10):3110–3116
Acknowledgments
This study has been supported by an unrestricted grant to Centro Dislipidemie (A.S.S.T. Grande Ospedale Metropolitano Niguarda, Milano, Italy) from the Alpro Foundation (Gent, Belgium). The founding sponsors had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; and in the decision to publish the results.
Author contributions
MR wrote the paper and performed ELISA experiments; PM wrote the paper and coordinated the study; AA, LC and CS conceived the study and critically revised the manuscript; CP selected the patients and acted as clinical monitor; SG performed all the statistical analyses; BM and CM performed biochemical analysis; MG and CV performed analysis on HDL; GA performed isoflavones analysis; and RB was the dietician. All authors reviewed the results and approved the final version of the manuscript.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Conflict of interest
The authors declare no conflict of interest.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Ruscica, M., Pavanello, C., Gandini, S. et al. Effect of soy on metabolic syndrome and cardiovascular risk factors: a randomized controlled trial. Eur J Nutr 57, 499–511 (2018). https://doi.org/10.1007/s00394-016-1333-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00394-016-1333-7