Abstract
Purpose
To evaluate clinical efficacy/safety of augmented peripheral osteoplasty in oncologic patients with long-term follow-up.
Materials and Methods
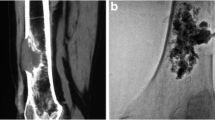
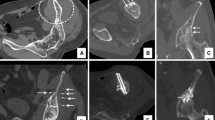
Percutaneous augmented peripheral osteoplasty was performed in 12 patients suffering from symptomatic lesions of long bones. Under extensive local sterility measures, anesthesiology care, and fluoroscopic guidance, direct access to lesion was obtained and coaxially a metallic mesh consisting of 25–50 medical grade stainless steel micro-needles (22 G, 2–6 cm length) was inserted. PMMA for vertebroplasty was finally injected under fluoroscopic control. CT assessed implant position 24-h post-treatment.
Results
Clinical evaluation included immediate and delayed follow-up studies of patient’s general condition, NVS pain score, and neurological status. Imaging assessed implant’s long-term stability. Mean follow-up was 16.17 ± 10.93 months (range 2–36 months). Comparing patients’ scores prior (8.33 ± 1.67 NVS units) and post (1.42 ± 1.62 NVS units) augmented peripheral osteoplasty, there was a mean decrease of 6.92 ± 1.51 NVS units. Overall mobility improved in 12/12 patients. No complication was observed.
Conclusion
Percutaneous augmented peripheral osteoplasty (rebar concept) for symptomatic malignant lesions in long bones seems to be a possible new technique for bone stabilization. This combination seems to provide necessary stability against shearing forces applied in long bones during weight bearing.




Similar content being viewed by others
References
Gasbarrini A, Beisse R, Fisher C, Rhines L. Spine metastasis. Int J Surg Oncol. 2011;2011:375097. doi:10.1155/2011/375097.
Kelekis AD, Somon T, Yilmaz H, Bize P, Brountzos EN, Lovblad K, Ruefenacht D, Martin JB. Interventional spine procedures. Eur J Radiol. 2005;55(3):362–83.
Anselmetti GC, Manca A, Tutton S, Chiara G, Kelekis A, Facchini FR, Russo F, Regge D, Montemurro F. Percutaneous vertebral augmentation assisted by PEEK implant in painful osteolytic vertebral metastasis involving the vertebral wall: experience on 40 patients. Pain Physician. 2013;16(4):E397–404.
Baerlocher MO, Saad WE, Dariushnia S, Barr JD, McGraw JK, Nikolic B. Society of Interventional Radiology Standards of Practice Committee. Quality improvement guidelines for percutaneous vertebroplasty. J Vasc Interv Radiol. 2014;25(2):165–70.
Barr JD, Jensen ME, Hirsch JA, McGraw JK, Barr RM, Brook AL, Meyers PM, Munk PL, Murphy KJ, O’Toole JE, Rasmussen PA, Ryken TC, Sanelli PC, Schwartzberg MS, Seidenwurm D, Tutton SM, Zoarski GH, Kuo MD, Rose SC, Cardella JF. Position statement on percutaneous vertebral augmentation: a consensus statement developed by the Society of Interventional Radiology (SIR), American Association of Neurological Surgeons (AANS) and the Congress of Neurological Surgeons (CNS), American College of Radiology (ACR), American Society of Neuroradiology (ASNR), American Society of Spine Radiology (ASSR), Canadian Interventional Radiology Association (CIRA), and the Society of NeuroInterventional Surgery (SNIS). J Vasc Interv Radiol. 2014;25(2):171–81.
Gangi A, Sabharwal T, Irani FG, Buy X, Morales GP, Adam A. Quality assurance guidelines for percutaneous vertebroplasty. CVIR. 2006;29(2):173–8.
Habermann ET, Lopez RA. Metastatic disease of bone and treatment of pathological fractures. Orthop Clin North Am. 1989;20:469–86.
Ward WG, Holsenbeck S, Dorey FJ, Spang J, Howe D. Metastatic disease of the femur: surgical treatment. Clin Orthop Relat Res. 2003;415S:230–44.
Lutz S, Chowb E. A review of recently published radiotherapy treatment guidelines for bone metastases: contrasts or convergence? J Bone Oncol. 2012;1:18–23.
Anselmetti GC, Manca A, Ortega C, Grignani G, Debernardi F, Regge D. Treatment of extraspinal painful bone metastases with percutaneous cementoplasty: a prospective study of 50 patients. Cardiovasc Interv Radiol. 2008;6:1165–73.
Anselmetti GC. Osteoplasty: percutaneous bone cement injection beyond the spine. Semin Interv Radiol. 2010;2:199–208.
Chang SW, Murphy KP. Percutaneous CT-guided cementoplasty for stabilization of a femoral neck lesion. J Vasc Interv Radiol. 2005;6:889–90.
Basile A, Giuliano G, Scuderi V, Motta S, Crisafi R, Coppolino F, Mundo E, Banna G, Di Raimondo F, Patti MT. Cementoplasty in the management of painful extraspinal bone metastases: our experience. Radiol Med. 2008;7:1018–28.
Deschamps F, Farouil G, Hakime A, Barah A, Guiu B, Teriitehau C, Auperin A, deBaere T. Cementoplasty of metastases of the proximal femur: is it a safe palliative option? J Vasc Interv Radiol. 2012;23(10):1311–6.
Mirels H. Metastatic disease in long bones. A proposed scoring system for diagnosing impending pathologic fractures. Clin Orthop Relat Res. 1989;249:256–64.
Ristevski B, Jenkinson RJ, Stephen DJ, Finkelstein J, Schemitsch EH, McKee MD, Kreder HJ. Mortality and complications following stabilization of femoral metastatic lesions: a population-based study of regional variation and outcome. Can J Surg. 2009;52(4):302–8.
van der Linden YM, Kroon HM, Dijkstra SP, Lok JJ, Noordijk EM, Leer JW, Marijnen CA, Dutch Bone Metastasis Study Group. Simple radiographic parameter predicts fracturing in metastatic femoral bone lesions: results from a randomised trial. Radiother Oncol. 2003;69(1):21–31.
Anselmetti GC, Manca A, Chiara G, Tutton S, Iussich G, Gino G, Grignani G, Ortega C, Moselli N, Regge D. Painful pathologic fracture of the humerus: percutaneous osteoplasty with bone marrow nails under hybrid computed tomography and fluoroscopic guidance. J Vasc Interv Radiol. 2011;22(7):1031–4.
Deschamps F, Farouil G, Hakime A, Teriitehau C, Barah A, de Baere T. Percutaneous stabilization of impending pathological fracture of the proximal femur. Cardiovasc Interv Radiol. 2012;35(6):1428–32.
Nakata K, Kawai N, Sato M, Cao G, Sahara S, Sonomura T, Takasaka I, Minamiguchi H, Nakai M. Bone marrow nails created by percutaneous osteoplasty for long bone fracture: comparisons among acrylic cement alone, acrylic-cement-filled bare metallic stent, and acrylic-cement-filled covered metallic stent. Cardiovasc Interv Radiol. 2011;34(3):609–14.
Nakata K, Kawai N, Sato M, Cao G, Sahara S, Tanihata H, Takasaka I, Minamiguchi H, Nakai T. Percutaneous osteoplasty with a bone marrow nail for fractures of long bones: experimental study. J Vasc Interv Radiol. 2010;21(9):1436–41.
Kawai N, Sato M, Iwamoto T, Tanihata H, Minamiguti H, Nakata K. Percutaneous osteoplasty with use of a cement-filled catheter for a pathologic fracture of the humerus. J Vasc Interv Radiol. 2007;18(6):805–9.
He C, Tian Q, Wu CG, Gu Y, Wang T, Li M. Feasibility of percutaneous cementoplasty combined with interventional internal fixation for impending pathologic fracture of the proximal femur. J Vasc Interv Radiol. 2014;25(7):1112–7.
Dayer R, Peter R. Percutaneous cementoplasty complicating the treatment of a pathologic subtrochanteric fracture: a case report. Injury. 2008;7:801–4.
Piccioli A, Rossi B, Scaramuzzo L, Spinelli MS, Yang Z, Maccauro G. Intramedullary nailing for treatment of pathologic femoral fractures due to metastases. Injury. 2014;45(2):412–7.
Conflict of interest
Authors have no conflict of interest to declare. No industry support was received for this study.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kelekis, A., Filippiadis, D., Anselmetti, G. et al. Percutaneous Augmented Peripheral Osteoplasty in Long Bones of Oncologic Patients for Pain Reduction and Prevention of Impeding Pathologic Fracture: The Rebar Concept. Cardiovasc Intervent Radiol 39, 90–96 (2016). https://doi.org/10.1007/s00270-015-1138-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00270-015-1138-8