Abstract
Purpose
In the total hip arthroplasty (THA), the optimal administration route of tranexamic acid (TXA) remains controversial. This study was designed to investigate the impact of topical injection of TXA on blood loss during primary unilateral THA as well as short-term safety and adverse side effects compared with intravenous administration of TXA.
Material and methods
In this study, 75 patients who underwent unilateral THA were randomly divided into 3 groups receiving intra-articular TXA (IA group), intravenous TXA (IV group) or no TXA (control group C). Blood loss, postoperative drainage, covert blood loss, total blood volume, the number of blood transfusions after surgery and transfusion rate, incidence of deep venous thrombosis and pulmonary embolism were recorded and evaluated in the three groups after 1 week and 1 month.
Results
There were significant differences in the quantity of postoperative drainage, covert blood loss, total blood volume, the number of blood transfusions after surgery and transfusion rates between the three groups (P < 0.05), but blood loss during surgery showed no significant differences among the three groups (P > 0.05). In the IV group, 1 patient suffered from deep venous thrombosis of the lower limbs and in the C group, 2 patients suffered from superficial venous thrombosis of the lower limbs 2 and 4 days after surgery, respectively. In the IA group no complications occurred during the follow-up period.
Conclusion
Preoperative intravenous TXA and postoperative topical TXA significantly reduced postoperative blood loss and transfusion rates among the patients who underwent primary unilateral THA and the short-term safety was good. The data suggest that topical injection of TXA is safer and more effective, without postoperative complications.
Zusammenfassung
Zielsetzung
Der optimale Weg der Tranexamsäure(TXA)-Applikation im Rahmen der Hüfttotalendoprothese ist weiterhin umstritten. In der vorliegenden Studie sollten der Effekt einer topischen TXA-Injektion auf den Blutverlust während einer einseitigen Hüfttotalendoprothese, die kurzfristige Sicherheit und unerwünschte Wirkungen untersucht werden, jeweils im Vergleich zur intravenösen TXA-Applikation.
Material und Methoden
In dieser Studie wurden 75 Patienten, die eine einseitige Hüfttotalendoprothese erhielten, in 3 Gruppen randomisiert. Sie erhielten intraartikulär TXA (i.a.-Gruppe), intravenös TXA (i.v.-Gruppe) oder keine TXA (Kontrollgruppe). Dokumentiert und ausgewertet wurden Blutverluste, die postoperative Drainage, versteckte Blutverluste, das Gesamtblutvolumen, die Zahl der Bluttransfusionen nach chirurgischem Eingriff, die Transfusionsrate sowie die Inzidenz von tiefen Venenthrombosen und Lungenembolien, jeweils nach einer Woche und einem Monat in den drei Gruppen.
Ergebnisse
Es fanden sich signifikante quantitative Unterschiede zwischen den drei Gruppen in postoperativer Drainage, versteckten Blutverlusten, dem Gesamtblutvolumen, der Zahl der Bluttransfusionen nach chirurgischem Eingriff und in der Transfusionsrate (p < 0,05). Keine signifikanten Unterschiede zeigten sich dagegen im Blutverlust während des chirurgischen Eingriffs (p > 0,05). In der i.v.-Gruppe kam es bei einem Patienten zu einer tiefen Venenthrombose der unteren Extremitäten. In der Kontrollgruppe erlitten 2 Patienten eine oberflächliche Venenthrombose der unteren Extremitäten (2 bzw. 4 Tage nach dem Eingriff). Bei den Patienten der i.a.-Gruppe ereigneten sich in der Follow-up-Phase keine Komplikationen.
Schlussfolgerung
Die präoperative i.v.-Applikation und postoperative topische Applikation von TXA reduzierten signifikant den postoperativen Blutverlust und die Transfusionsrate bei Patienten, die einer primären einseitigen Hüfttotalendoprothese unterzogen wurden. Die kurzfristige Sicherheit war gut. Die Ergebnisse deuten darauf hin, dass die topische Injektion von TXA sicherer und wirksamer ist, ohne dass es dabei zu postoperativen Komplikationen kommt.



Similar content being viewed by others
References
Mednick RE, Alvi HM, Krishnan V et al (2014) Factors affecting readmission rates following primary total hip Arthroplasty. J Bone Joint Surg Am 96(14):1201–1209
Gibon E, Courpied JP, Hamadouche M (2013) Total joint replacement and blood loss: what is the best equation. Int Orthop 37:735–739
Bierbaum BE, Callaghan JJ, Galante JO et al (1999) An analysis of blood management in patients having a total hip or knee arthroplasty. J Bone Joint Surg Am 81:2–10
Massicotte L, Denault AY, Beaulieu D et al (2011) Aprotinin versus tranexamic acid during liver transplantation: impact on blood product requirements and survival. Transplantation 91:1273
Dhir A (2014) Antifibrinolytics in cardiac surgery. Ann Card Anaesth 16:117–125
Roy SP, Tanki UF, Dutta A et al (2012) Efficacy of intra-articular tranexamic acid in blood loss reduction following primary unilateral total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 20:2494–2501
Alshryda S, Mason J, Vaqhela M et al (2013) Topical(intra-articular) tranexamic acid reduces blood loss and transfusion rates following total knee replacement: a randomized controlled trial. J Bone Joint Surg Am 95:1961–1968
Maniar RN, Kumar G, Singhi T et al (2014) Most effective regimen of tranexamic acid in knee arthroplasty: a prospective randomized controlled study in 240 patient. Clin Orthop 470:2605–2612
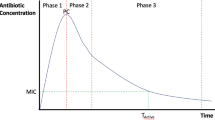
Blanie A, Bellamy L, Rhayem Y et al (2013) Duration of postoperative fibrinolysis after total hip or knee replacement: a laboratory follow-up study. Thromb Res 131(1):6–11
Alshryda S, Sukeik M, Sarda P, Blenkinsopp J, Haddad FS, Mason JM (2014) A systematic review and meta-analysis of the topical administration of tranexamic acid in total hip and knee replacement. Bone Joint J 96-B:1005–1015
Nadler SB, Hidalgo JU, Bloch T (1962) Prediction of blood volume in normal human adults. Surgery 51(2):224
Sehat KR, Evans RL, Newman JH (2004) Hidden blood loss following hip and knee arthroplasty correct management of blood loss should take hidden loss into account. J Bone Joint Surg Br 86(4):561
Tai TW, Chang CW, Lai KA et al (2012) Effects of Tourniquet Use on Blood Loss and Soft-Tissue Damage in Total Knee Arthroplasty:A Randomized Controlled Trial. J Bone Joint Surg 94(24):2209–2215
Liu X, Zhang X, Chen Y et al (2011) Hidden blood loss after total hip arthroplasty. J Arthroplasty 26(7):1100–1105
Li B, Wen Y, Liu D et al (2012) The effect of knee position on blood loss and range of motion following total knee arthroplasty. Knee Surg Sports Traumatol Arthrosc 20(3):594–599
Markar SR, Jones GG, Karthikesalingam A (2012) Transfusion drains versus suction drains in total knee replacement: meta-analysis. Knee Surg Sports Traumatol Arthrosc 20(9):1766–1772
Syrovets T, Lunov O, Simmet T (2012) Plasmin as a proinflammatory cell activator. J Leukoc Biol 92((3):509–519
Imai N, Dohmae Y, Suda K et al (2012) Tranexamic acid for reduction of blood loss during total hip arthroplasty. J Arthroplasty 27(1843):1838
McCormack PL (2012) Tranexamic acid a review of its use in the treatment of hyper fibrinolysis. Drugs 72:585–617
Irisson E, Hemon Y, Pauly V et al (2012) Tranexamic acid reduces blood loss and financial cost in primary total hip and knee replacement surgery. Orthop Traumatol Surg Res 98:477–483
Clave A, Fazilleau F, Dumser D et al (2012) Efficacy of tranexamic acid on blood loss after primary cementless total hip replacement with rivaroxaban thrombopro- phylaxis: a case-control study in 70 patients. Orthop Traumatol Surg Res 98(5):484–490
Alshryda S, Mason J, Sarda P et al (2013) Topical(intra-articular) tranexamic acid reduces blood loss and transfusion rates following total hip replacement: a randomized controlled trial (TRANX-H). J Bone Joint Surg Am 95:1969–1974
Gilbody J, Dhotar HS, Perruccio AV et al (2014) Topical tranexamic acid reduces transfusion rates in total hip and knee arthroplasty. J Arthroplasty 29:681–684
Konig G, Hamlin BR, Waters JH (2013) Topical tranexamic acid reduces blood loss and transfusion rates in total hip and total knee arthroplasty. J Arthroplast 28:1473–1476
Huotari K, Agthe N, Lyytikainen O (2007) Validation of surgical siteinfection surveillance in orthopedic procedures. Am J Infect Control 35:216–221
Yue C, Kang PD, Yang PQ, Xie JW, Pei FX (2014) Topical application of Tranexamic acid in primary total hip Arthroplasty: A randomized double-blind controlled trial. J Arthroplast 29(12):2452–2456
Wei W, Wei BE (2014) Comparison of topical and intravenous Tranexamic acid on blood loss and transfusion rates in total hip Arthroplasty. J Arthroplast 29(11):2113–2116
Acknowledgements
We thank Xianghao Ma, Yudong Jia, Huichao Wang for assistance in recruitment and data collection during the trial, Yingjie Zhu and Youwen Liu for clinical trials and regulatory expertise in the trial steering committee and data monitoring committee for this trial. The sponsors and funding bodies had no role in the inception or design of the study, data collection and analysis or preparation of this report.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
Y. Zhang, L. Zhang, X. Ma, Y. Jia, H. Wang, Y. Zhu and Y. Liu state that there are no conflicts of interest.
All studies on humans described in the present manuscript were carried outwith the approval of the responsible ethics committee and in accordance with national lawand the Helsinki Declaration of 1975 (in its current, revised form). Informed consent was obtained from all patients included in studies.
Additional information
Ying Zhang and Leilei Zhang contributed equally to this work.
Rights and permissions
About this article
Cite this article
Zhang, Y., Zhang, L., Ma, X. et al. What is the optimal approach for tranexamic acid application in patients with unilateral total hip arthroplasty?. Orthopäde 45, 616–621 (2016). https://doi.org/10.1007/s00132-016-3252-y
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00132-016-3252-y