Abstract
Background
We previously showed that using the radial artery access site as opposed to the femoral artery site decreases the radiation exposure of patients during coronary artery interventions. The objective of this study was to compare radiation exposure levels of the operating physician during coronary interventions when incorporating both radial and femoral artery approaches.
Methods
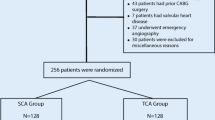
The study assessed all coronary angioplasties performed in a major metropolitan general hospital. The study design was prospective and observational, in which we measured the radiation exposure of the patient and the operator. Measurements of radiation levels were made using an electronic personal dosimeter (Diamentor® E2-DAP) at the radial and at the femoral artery access sites. An interventional cardiologist operator performed all the percutaneous coronary interventions (PCI) using a single-plane angiography unit via both femoral and radial artery approaches.
Results
Data from 252 PCIs were recorded. The mean physician radiation exposure levels from the femoral access site and the right radial access site were 40.5 ± 20.2 µSv and 47.5 ± 26.5 µSv, respectively (p < 0.02). There was a strong correlation between physician and patient radiation exposure levels. However, there was no correlation between patient body mass index and radiation exposure levels.
Conclusion
We found significantly higher physician radiation exposure levels with the radial artery than with the femoral artery access site.
Zusammenfassung
Hintergrund
Die Autoren haben bereits früher nachgewiesen, dass durch Nutzung der A. radialis als Zugangslokalisation im Gegensatz zur A. femoralis die Strahlenbelastung der Patienten bei Koronarinterventionen sinkt. Ziel der vorliegenden Arbeit war es, die Strahlenexpositionsdosen des Operateurs während der Koronarintervention sowohl bei Verwendung eines Radial- als auch bei Nutzung eines Femoralarterienzugangs zu untersuchen.
Methoden
Es wurden alle Koronarinterventionen untersucht, die in einem bedeutenden großstädtischen Allgemeinkrankenhaus erfolgten. Im Design handelte es sich um eine prospektive Beobachtungsstudie, in der die Strahlenbelastung von Patient und Operateur gemessen wurde. Die Messung der Strahlendosen erfolgte unter Verwendung eines elektronischen Personendosimeters (Diamentor® E2-DAP) am Ort des Zugangs zur Radial- bzw. zur Femoralarterie. Ein interventionell tätiger Kardiologe führte alle perkutanen Koronarinterventionen (PCI) unter Einsatz eines monoplanen Angiographiesystems via Femoral- oder Radialarterienzugang durch.
Ergebnisse
Die Daten von 252 PCI wurden dokumentiert. Die durchschnittliche Strahlenexpositionsdosis des Arztes betrug bei Zugang über die Femoralarterie 40,5 ± 20,2 µSv bzw. bei Zugang über die rechte Radialarterie 47,5 ± 26,5 µSv, (p < 0,02). Es bestand eine starke Korrelation der Strahlenexpositionsdosen von Arzt und Patient. Jedoch fand sich keine Korrelation zwischen dem Body-Mass-Index des Patienten und den Strahlenexpositionsdosen.
Schlussfolgerung
Bei einem Zugang über die Radialarterie stellten die Autoren signifikant höhere Strahlenbelastungsdosen des Arztes fest als bei einem Zugang über die A. femoralis.



Similar content being viewed by others
References
Adamo M, Byrne RA, Baumbach A et al (2016) Assessing the cardiology community position on transradial intervention and the use of bivalirudin in patients with acute coronary syndrome undergoing invasive management: results of an EAPCI survey. EuroIntervention 12(9):1154–1163. https://doi.org/10.4244/EIJY15M12_01
Burzotta F, Trani C, Mazzari MA et al (2012) Vascular complications and access crossover in 10,676 transradial percutaneous coronary procedures. Am Heart J 163(2):230–238. https://doi.org/10.1016/j.ahj.2011.10.019
Mehta SR, Jolly SS, Cairns J et al (2012) Effects of radial versus femoral artery access in patients with acute coronary syndromes with or without ST-segment elevation. J Am Coll Cardiol 60(24):2490–2499. https://doi.org/10.1016/j.jacc.2012.07.050
Romagnoli E, Biondi-Zoccai G, Sciahbasi A et al (2012) Radial versus femoral randomized investigation in ST-segment elevation acute coronary syndrome: the RIFLE-STEACS (Radial Versus Femoral Randomized Investigation in ST-Elevation Acute Coronary Syndrome) study. J Am Coll Cardiol 60(24):2481–2489. https://doi.org/10.1016/j.jacc.2012.06.017
Ibanez B, James S, Agewall S et al (2017) 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC). Eur Heart J. https://doi.org/10.1093/eurheartj/ehx393
Brasselet C, Blanpain T, Tassan-Mangina S et al (2008) Comparison of operator radiation exposure with optimized radiation protection devices during coronary angiograms and ad hoc percutaneous coronary interventions by radial and femoral routes. Eur Heart J 29(1):63–70. https://doi.org/10.1093/eurheartj/ehm508
Lange HW, von Boetticher H (2006) Randomized comparison of operator radiation exposure during coronary angiography and intervention by radial or femoral approach. Catheter Cardiovasc Interv 67(1):12–16. https://doi.org/10.1002/ccd.20451
Mann JT 3rd, Cubeddu G, Arrowood M (1996) Operator radiation exposure in PTCA: comparison of radial and femoral approaches. J Invasive Cardiol 8(Suppl D):22D–25D
Liu H, Jin Z, Jing L (2014) Comparison of radiation dose to operator between transradial and transfemoral coronary angiography with optimised radiation protection: a phantom study. Radiat Prot Dosimetry 158(4):412–420. https://doi.org/10.1093/rpd/nct261
Lo TS, Ratib K, Chong AY et al (2012) Impact of access site selection and operator expertise on radiation exposure; a controlled prospective study. Am Heart J 164(4):455–461. https://doi.org/10.1016/j.ahj.2012.06.011
Michael TT, Alomar M, Papayannis A et al (2013) A randomized comparison of the transradial and transfemoral approaches for coronary artery bypass graft angiography and intervention: the RADIAL-CABG Trial (RADIAL Versus Femoral Access for Coronary Artery Bypass Graft Angiography and Intervention). JACC Cardiovasc Interv 6(11):1138–1144. https://doi.org/10.1016/j.jcin.2013.08.004
Haga Y, Chida K, Kaga Y et al (2017) Occupational eye dose in interventional cardiology procedures. Sci Rep 7(1):569. https://doi.org/10.1038/s41598-017-00556-3
Suzuki S, Furui S, Kohtake H et al (2006) Radiation exposure to patient’s skin during percutaneous coronary intervention for various lesions, including chronic total occlusion. Circ J 70(1):44–48
Tarighatnia A, Pourafkari L, Farajollahi A et al (2017) Operator radiation exposure during transradial coronary angiography: effect of single vs. double catheters. Herz. https://doi.org/10.1007/s00059-017-4595-9
Chambers CE, Fetterly KA, Holzer R et al (2011) Radiation safety program for the cardiac catheterization laboratory. Catheter Cardiovasc Interv 77(4):546–556. https://doi.org/10.1002/ccd.22867
Politi L, Biondi-Zoccai G, Nocetti L et al (2012) Reduction of scatter radiation during transradial percutaneous coronary angiography: a randomized trial using a lead-free radiation shield. Catheter Cardiovasc Interv 79(1):97–102. https://doi.org/10.1002/ccd.22947
Mesbahi A, Mehnati P, Keshtkar A, Aslanabadi N (2008) Comparison of radiation dose to patient and staff for two interventional cardiology units: a phantom study. Radiat Prot Dosimetry 131(3):399–403. https://doi.org/10.1093/rpd/ncn188
Ikari Y, Nagaoka M, Kim JY et al (2005) The physics of guiding catheters for the left coronary artery in transfemoral and transradial interventions. J Invasive Cardiol 17(12):636–641
Tarighatnia A, Alian MAH, Ghojazadeh M, Farajollahi AR (2016) Comparison of the patient radiation exposure during coronary angiography and angioplasty procedures using trans-radial and trans-femoral access. J Cardiovasc Thorac Res 8(2):77–82. https://doi.org/10.15171/jcvtr.2016.15
Chida K, Morishima Y, Inaba Y et al (2012) Physician-received scatter radiation with angiography systems used for interventional radiology: comparison among many X‑ray systems. Radiat Prot Dosimetry 149(4):410–416. https://doi.org/10.1093/rpd/ncr312
Ball WT, Sharieff W, Jolly SS et al (2011) Characterization of operator learning curve for transradial coronary interventions. Circ Cardiovasc Interv 4(4):336–341. https://doi.org/10.1161/CIRCINTERVENTIONS.110.960864
Abdelaal E, Plourde G, MacHaalany J et al (2014) Effectiveness of low rate fluoroscopy at reducing operator and patient radiation dose during transradial coronary angiography and interventions. JACC Cardiovasc Interv 7(5):567–574. https://doi.org/10.1016/j.jcin.2014.02.005
Wassef AW, Hiebert B, Ravandi A et al (2014) Radiation dose reduction in the cardiac catheterization laboratory utilizing a novel protocol. JACC Cardiovasc Interv 7(5):550–557. https://doi.org/10.1016/j.jcin.2013.11.022
Neill J, Douglas H, Richardson G et al (2010) Comparison of radiation dose and the effect of operator experience in femoral and radial arterial access for coronary procedures. Am J Cardiol 106(7):936–940. https://doi.org/10.1016/j.amjcard.2010.06.002
Mercuri M, Mehta S, Xie C et al (2011) Radial artery access as a predictor of increased radiation exposure during a diagnostic cardiac catheterization procedure. JACC Cardiovasc Interv 4(3):347–352. https://doi.org/10.1016/j.jcin.2010.11.011
Vano E, Ubeda C, Leyton F et al (2009) Staff radiation doses in interventional cardiology: correlation with patient exposure. Pediatr Cardiol 30(4):409–413. https://doi.org/10.1007/s00246-008-9375-0
Park EY, Shroff AR, Crisco LV, Vidovich MI (2013) A review of radiation exposures associated with radial cardiac catheterisation. EuroIntervention 9(6):745–753. https://doi.org/10.4244/EIJV9I6A119
Agarwal S, Parashar A, Ellis SG et al (2014) Measures to reduce radiation in a modern cardiac catheterization laboratory. Circ Cardiovasc Interv 7(4):447–455. https://doi.org/10.1161/CIRCINTERVENTIONS.114.001499
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
A. Tarighatnia, A.R. Farajollahi, A.H. Mohammadalian, M. Ghojazadeh, M. Azadeh, E. Koleini, and N.D. Nader declare that they have no competing interests.
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all individual participants included in the study.
Rights and permissions
About this article
Cite this article
Tarighatnia, A., Farajollahi, A.R., Mohammadalian, A.H. et al. Radiation exposure levels according to vascular access sites during PCI. Herz 44, 330–335 (2019). https://doi.org/10.1007/s00059-017-4639-1
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00059-017-4639-1