Abstract
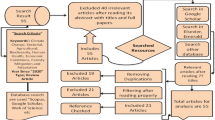
An increase in the annual daily temperature is documented and predicted to occur in the coming decades. Climate change has a direct effect and adverse impact on human health, as well as on multiple ecosystems and their species. The purpose of this paper is to review the effect of climate change on neglected tropical diseases including leishmaniasis, schistosomiasis, and lymphatic filariasis in the Eastern Mediterranean Region (EMR). A list of engine web searches was done; 280 full-text records were assessed for eligibility. Only 48 original records were included within the final selection for the review study. Most research results show an alteration of neglected diseases related to climate change influencing specifically the Eastern Mediterranean Region, in addition to the expectation of more effects at the level of vectors and reservoir whether its vector transmission route or its egg hatching and replication or even the survival of adult worms in the coming years. At the same time, not all articles related to the region interpret the direct or indirect effect of climate variations on these specific diseases. Although few studies were found describing some of climate change effects on neglected tropical diseases in the region, still, the region lacks research funding, technical, and mathematical model expertise regarding the direct effect of climate change on the ecosystems of these neglected tropical diseases.



Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Intergovernmental Panel on Climate Change. (2015). Summary for policymakers. In Climate Change 2014: Mitigation of Climate Change: Working Group III Contribution to the IPCC Fifth Assessment Report (pp. 1–30). introduction, Cambridge: Cambridge University Press.
Field CB, Barros V, Stocker TF, Qin D, Dokken DJ, Ebi KL, et al. (Ed.). IPCC 2012. Managing the risks of extreme events and disasters to advance climate change adaptation. A special report of the intergovernmental panel on climate change. Cambridge, UK, and New York, NY, USA: Cambridge University Press; 2012.
World Health Organization (WHO) febrauary, 2018. Climate change and human health. Available at: https://www.who.int/news-room/fact-sheets/detail/climate-change-and-health
Field, C.B., V.R. Barros, D.J. Dokken, et al. 2014. Climate change 2014: impacts, adaptation, and vulnerability. Part A: global and sectoral aspects. Working Group II Contribution to the Fifth Assessment Report of the Intergovernmental Panel on Climate Change. Cambridge, UK and New York, NY: Cambridge University Press.
McIntyre KM, Setzkorn C, Hepworth PJ, et al. Systematic assessment of the climate sensitivity of important human and domestic animals pathogens in Europe. Sci Rep. 2017;7:7134.
McMichael AJ. Globalization, climate change, and human health. N Engl J Med. 2013;368:1335–43.
Costello A, et al. Managing the health effects of climate change. Lancet. 2009;373:1693–733.
Watts N, et al. Health and climate change: policy responses to protect public health. Lancet. 2015;386:1861–914.
Bryson JM, Bishop-Williams KE, Berrang-Ford L, Nunez EC, Lwasa S, Namanya DB, Harper SL. Indigenous Health Adaptation To Climate Change Research Team. Neglected tropical diseases in the context of climate change in East Africa: a systematic scoping review. The American journal of tropical medicine and hygiene. 2020;102(6):1443–54.
World Health Organization (WHO), 2006. The World Health Report 2006. Geneva, Switzerland: WHO. Nairobi Climate Change Conference - November 2006. Available at: https://unfccc.int/files/press/backgrounders/application/pdf/factsheet_africa.pdf
World Health Organization (WHO), 2003. Climate change and human health - risks and responses. Summary. Available at: https://www.who.int/globalchange/summary/en/
Al-Delaimy, W., Ramanathan, V., & Sánchez Sorondo, M. (2020). Health of people, health of planet and our responsibility: climate change, air pollution and health. This reference is a full text book of 33 chapters begins with ecosystem protection of living organism and ending with the moral trust of scientists towards their society in leading the effect of climate change on human health.
B Yeh K, M Fair J, Smith W, Martinez Torres T, Lucas J, Monagin C, Winegar R, Fletcher J. Assessing climate change impact on ecosystems and infectious disease: important roles for genomic sequencing and a one health perspective. Tropic Med Infect Dis. 2020;5 (2):90.
Abuzaid AA, Abdoon AM, Aldahan MA, Alzahrani AG, Alhakeem RF, Asiri AM, Alzahrani MH, Memish ZA. Cutaneous leishmaniasis in Saudi Arabia: a comprehensive overview. Vector-Borne and Zoonotic Diseases. 2017;17(10):673–84.
Hotez PJ, Savioli L, Fenwick A. Neglected tropical diseases of the Middle East and North Africa: review of their prevalence, distribution, and opportunities for control. PLoS Negl Trop Dis. 2012;6(2):e1475.
Larsen M, Roepstorff A. Seasonal variation in development and survival of Ascaris suum and Trichuris suis eggs on pastures. Parasitology. 1999;119(2):209–22. https://doi.org/10.1017/S0031182099004503.
Gungoren B, Latipov R, Regallet G, Musabaev E. Effect of hygiene promotion on the risk of reinfection rate of intestinal parasites in children in rural Uzbekistan. Trans R Soc Trop Med Hyg. 2007;101(6):564–9. https://doi.org/10.1016/j.trrstmh.2007.02.011.
Pan C-T, Ritchie L, Hunter G. Reinfection and seasonal fluctuations of Ascaris lumbricoides among a group of children in an area where night soil is used. J Parasitol. 1954;40(5):603–8. https://doi.org/10.2307/3274027.
Seo B, Cho S, Choi J. Seasonal fluctuation of Ascaris reinfection incidences in a rural Korean population. Korean J Parsitol. 1979;17(1):11–8. https://doi.org/10.3347/kjp.1979.17.1.11.
Gunawardena G, Karunaweera N, Ismail M. Wet days: are they better indicators of Ascaris infection levels? J Helminthol. 2004;78:305–10. https://doi.org/10.1079/JOH2004252.
McCarthy JJ, Canziani OF, Leary NA, Dokken DJ, White KS. Climate change 2001: impacts, adaptation and vulnerability. Contribution of working group II to the third assessment report of the intergovernmental panel of climate change (IPCC). Cambridge (UK): Cambridge University Press; 2001.
Arene F. Ascaris suum: influence of embryonation temperature on the viabil- ity of the infective larva. J Therm Biol. 1986;11(1):9–15. https://doi.org/10.1016/0306-4565(86)90011-2.
Kim M, Pyo K, Hwang Y, Park K, Hwang I, Chai J, Shin E. Effect of tem- perature on embryonation of Ascaris suum eggs in an environmental chamber. Korean J Parasitol. 2012;50(3):239–42. https://doi.org/10.3347/kjp.2012.50.3.239.
Shoukry NM, Morsy TA. Arthropod borne diseases at Toshka. Upper Egypt World J Zool. 2011;6(2):126–33.
Hotez PJ, Savioli L, Fenwick A. Neglected tropical diseases of the Middle East and North Africa: review of their prevalence, distribution, and opportunities for control. PLoS Negl Trop Dis. 2012;6(2):e1475.
World Health Organization (WHO), the Regional Office for the Eastern Mediterranean, May 2020. Key facts about leishmaniasis .Available at: https://www.who.int/news-room/fact-sheets/detail/leishmaniasis.
World Health Organization (WHO), the Regional Office for the Eastern Mediterranean, May 2021. Key facts about Schistosomiasis .Available at: http://www.emro.who.int/health-topics/schistosomiasis/. This report and key facts about schistosomiasis is up to date information about schistosomiasis infection.
Al-Warid HS, Al-Saqur IM, Al-Tuwaijari SB, Zadawi KA. The distribution of cutaneous leishmaniasis in Iraq: demographic and climate aspects. Asian Biomedicine. 2017;11(3):255–60.
Pringle G. The sandflies (Phlebotominae) of Iraq. Bull Entomol Res. 1953;43(4):707–34.
Al-Obaidi MJ, Abd Al-Hussein MY, Al-Saqur IM. Survey study on the prevalence of cutaneous leishmaniasis in Iraq. Iraqi Journal of Science. 2016;57(3C):2181–7.
Zivdari M, Hejazi SH, Mirhendi SH, Jafari R, Rastegar HA, Abtahi SM. Molecular identification of leishmania parasites in sand flies (Diptera, Psychodidae) of an endemic foci in Poldokhtar, Iran. Advanced biomedical research. 2018;7.
Shirzadi MR, Mollalo A, Yaghoobi-Ershadi MR. Dynamic relations between incidence of zoonotic cutaneous leishmaniasis and climatic factors in Golestan Province. Iran Journal of arthropod-borne diseases. 2015;9(2):148.
Charrahy Z, Yaghoobi‐Ershadi MR, Shirzadi MR, Akhavan AA, Rassi Y, Hosseini SZ, Webb NJ, Haque U, Bozorg Omid F, Hanafi‐Bojd AA. Climate change and its effect on the vulnerability to zoonotic cutaneous leishmaniasis in Iran. Transboundary and emerging diseases. 2021. This reference is up to date and is using MaxEnt model to study effect of climate change on cutaneous leishmaniasis ecological niches.
el-Hassan AM, Zijlstra EE, Ismael A, Ghalib HW. Recent observations on the epidemiology of Kala-azar in the eastern and central states of the Sudan. Tropical and geographical medicine. 1995;47(4):151–6.
Osman OF, Kager PA, Oskam L. Leishmaniasis in the Sudan: a literature review with emphasis on clinical aspects. Tropical Med Int Health. 2000;5(8):553–62.
Pratlong F, Dereure J, Bucheton B, El-Saf S, Dessein A, Lanotte G, et al. Sudan: the possible original focus of visceral leishmaniasis. Parasitology. 2001;122:599–605.
Zijlstra EE, el-Hassan AM. Leishmaniasis in Sudan Visceral leishmaniasis. Trans R Soc Trop Med Hyg. 2001;95(Suppl 1):S27-58.
Sunyoto T, Potet J, Boelaert M. Visceral leishmaniasis in Somalia: a review of epidemiology and access to care. PLoS neglected tropical diseases. 2017;11(3):e0005231.
Marlet MVL, Wuillaume F, Jacquet D, Quispe KW, Dujardin JC, Boelaert M. A neglected disease of humans: a new focus of visceral leishmaniasis in Bakool, Somalia. Trans R Soc Trop Med Hyg. 2003;97:667–71. https://doi.org/10.1016/S0035-9203(03)80099-8.
Qayad MG. Health care services in transitional Somalia: challenges and recommendations. Bild An Int J Somali Stud. 2007;7:190–210.
Fuje MM, Ruiz Postigo JA EM& B-IR. Scaling up the control of visceral leishmaniasis in Somalia. 2011. p. Poster presented at 7th European Congress of Tropi.
Elnaiem DEA. Ecology and control of the sand fly vectors of Leishmania donovani in East Africa, with special emphasis on Phlebotomus orientalis. J Vector Ecol. 2011;36:23–31.
Beyrer C, Villar JC, Suwanvanichkij V, Singh S, Baral SD, Mills EJ. Neglected diseases, civil conflicts, and the right to health. Lancet. 2007;370:619–27. https://doi.org/10.1016/S0140-6736(07)61301-4.
Gryseels B, Polman K, Clerinx J, Kestens L. Human schistosomiasis. The Lancet. 2006;368(9541):1106–18.
Lotfy WM. Climate change and epidemiology of human parasitosis in Egypt: a review. J Adv Res. 2014;5(6):607–13.
Patz JA, Graczyk TK, Geller N, Vittor AY. Effects of environmental change on emerging parasitic diseases. Int J Parasitol. 2000;30(12–13):1395–405.
Sady H, Al-Mekhlafi HM, Mahdy MA, Lim YA, Mahmud R, Surin J. Prevalence and associated factors of schistosomiasis among children in Yemen: implications for an effective control programme. PLoS Negl Trop Dis. 2013 22;7(8):e2377.
Sallam JA, Wright SG. Schistosomiasis mansoni in Yemen: a review. Ann Saudi Med. 1992;12(3):294–6.
Simonsen PE, Derua YA, Magesa SM, Pedersen EM, Stensgaard AS, Malecela MN, Kisinza WN: Lymphatic filariasis control in Tanga Region, Tanzania: status after eight rounds of mass drug administration.
Halliday A, Guimaraes AF, Tyrer HE, Metuge H, Patrick C, Arnaud KO, Kwenti T, Forsbrook G, Steven A, Cook D, Enyong P, Wanji S, Taylor MJ, Turner JD. A murine macrofilaricide pre-clinical screening model for onchocerciasis and lymphatic filariasis. Parasit Vectors. 2014;7(1):472.
World Health Organization (WHO), 2021: key facts about lymphatic filariasis: progress report. Geneva. .Available at : https://www.who.int/news-room/factsheets/detail/lymphatic-filariasis
Ramzy RM, Goldman AS, Kamal HA. Defining the cost of the Egyptian lymphatic filariasis elimination programme. Filaria J. 2005;4:7.
Ramzy RM, Kamal HA, Hassan MA, Haggag AA. Elimination of lymphatic filariasis as a public health problem from the Arab Republic of Egypt. Acta tropica. 2019;199:105121 (This paper describes the steps of elimination LF in Egypt and the application of MDA rounds for population).
World Health Organization, March 2018. Neglected tropical diseases. Egypt: first country in Eastern Mediterranean region to eliminate lymphatic filariasis. Availavle at: https://www.who.int/neglected_diseases/news/Egypt_first_EMRO_country_eliminate_LF/en/
Ramzy RM, Al Kubati AS. Progress towards elimination of lymphatic filariasis in the Eastern Mediterranean Region. International Health. 2021;13(Supplement_1):S28-32.
Coates SJ, Norton SA. The effects of climate change on infectious diseases with cutaneous manifestations. Int J Women's Dermatol. 2020
Pedersen UB, Stendel M, Midzi N, Mduluza T, Soko W, Stensgaard AS, Vennervald BJ, Mukaratirwa S, Kristensen TK. Modelling climate change impact on the spatial distribution of fresh water snails hosting trematodes in Zimbabwe. Parasit Vectors. 2014;7(1):1–2.
Stensgaard AS, Utzinger J, Vounatsou P, Hürlimann E, Schur N, Saarnak CF, Simoonga C, Mubita P, Kabatereine NB, Tchuenté LA, Rahbek C. Large-scale determinants of intestinal schistosomiasis and intermediate host snail distribution across Africa: does climate matter? Acta Trop. 2013;128(2):378–90.
Pullan RL, Brooker SJ. The global limits and population at risk of soil-transmitted helminth infections in 2010. Parasit Vectors. 2012;5(1):1–4.
Brooker S, Clements AC, Bundy DA. Global epidemiology, ecology and control of soil-transmitted helminth infections. Adv Parasitol. 2006;62:221–61.
Okulewicz A. The impact of global climate change on the spread of parasitic nematodes. Annals of Parasitology. 2017;63(1):15–20.
Hernandez AD, Poole A, Cattadori IM. Climate changes influence free-living stages of soil-transmitted parasites of European rabbits. Glob Change Biol. 2013;19(4):1028–42.
Weaver HJ, Hawdon JM, Hoberg EP. Soil-transmitted helminthiases: implications of climate change and human behavior. Trends Parasitol. 2010;26(12):574–81.
Mokhtari M, Miri M, Nikoonahad A, Jalilian A, Naserifar R, Ghaffari HR, Kazembeigi F. Cutaneous leishmaniasis prevalence and morbidity based on environmental factors in Ilam, Iran: spatial analysis and land use regression models. Acta Trop. 2016;163:90–7.
Blum AJ, Hotez PJ. Global “worming”: climate change and its projected general impact on human helminth infections.
Dhimal M, Ahrens B, Kuch U. Climate change and spatiotemporal distributions of vector-borne diseases in Nepal–a systematic synthesis of literature. PloS one. 2015;10(6):e0129869.
Slater H, Michael E. Predicting the current and future potential distributions of lymphatic filariasis in Africa using maximum entropy ecological niche modelling. PloS one. 2012;7(2):e32202.
Akinwale OP, Ajayi MB, Akande DO, Gyang PV, Adeleke MA, Adeneye AK, Adebayo MO, Dike AA. Urinary schistosomiasis around Oyan Reservoir, Nigeria: twenty years after the first outbreak. Iran J Public Health. 2010;39(1):92.
De Clercq D, Vercruysse J, Sène M, Seck I, Sall CS, Ly A, Southgate VR. The effects of irrigated agriculture on the transmission of urinary schistosomiasis in the middle and upper valleys of the Senegal River basin. Ann Trop Med Parasitol. 2000;94(6):581–90.
Fazal O, Hotez PJ. NTDs in the age of urbanization, climate change, and conflict: Karachi, Pakistan as a case study. PLOS Neglected Tropical Diseases. 2020;14(11):e0008791.
Schorscher J, Goris M. Incrimination of Phlebotomus (Larroussius) orientalis as a vector of visceral leishmaniasis in western Upper Nile Province, southern Sudan. Trans R Soc Trop Med Hyg. 1992;86:622–3.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Conflict of Interest
The author declares no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Climate Change and Health
This article is part of the Topical Collection on Global Environmental Health and Sustainability
Rights and permissions
About this article
Cite this article
Al-Delaimy, A.K. The Prospective Effects of Climate Change on Neglected Tropical Diseases in the Eastern Mediterranean Region: a Review. Curr Envir Health Rpt 9, 315–323 (2022). https://doi.org/10.1007/s40572-022-00339-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40572-022-00339-7