Abstract
Objectives
To evaluate the cost effectiveness of onabotulinumtoxinA (BOTOX®, 200 units [200 U]) for the management of urinary incontinence (UI) in adults with neurogenic detrusor overactivity (NDO) due to subcervical spinal cord injury or multiple sclerosis that is not adequately managed with anticholinergic drugs (ACHDs).
Perspective
UK National Health Service (NHS) perspective.
Methods
A Markov state-transition model was developed, which compared onabotulinumtoxinA + best supportive care (BSC) with BSC alone (comprising behavioural therapy and pads, alone or in combination with clean intermittent catheterization and possibly with ACHDs). Non-responders were eligible for invasive procedures. Health states were defined according to the reduction in UI episodes. Efficacy data and estimates of resource utilization were pooled from 468 patients on onabotulinumtoxinA in two phase III clinical trials. Drug costs (2013) and administration costs (NHS Reference Costs 2011–2012) were obtained from published sources. The time horizon of the model was 5 years, and costs and benefits were discounted at 3.5 %. Scenario, one-way and probabilistic sensitivity analyses (PSAs) were conducted to explore uncertainties around the assumptions.
Results
In the base case, treatment with onabotulinumtoxinA + BSC over 5 years was associated with an increase in costs of £1,689 and an increase in quality-adjusted life-years (QALYs) of 0.4, compared with BSC alone, resulting in an incremental cost-effectiveness ratio of £3,850 per QALY gained. Sensitivity analyses showed that utility values had the greatest influence on model results. PSA suggests that onabotulinumtoxinA + BSC had a 100 % probability of being cost effective at a willingness to pay of <£20,000.
Conclusion
For adult patients with NDO who are not adequately managed with ACHDs, onabotulinumtoxinA + BSC appears to be a cost-effective use of resources in the UK NHS.
Similar content being viewed by others
OnabotulinumtoxinA (BOTOX®, 200 U) + best supportive care (BSC) has been shown to significantly reduce the number of urinary incontinence (UI) episodes in adult patients with neurogenic detrusor overactivity (NDO) due to spinal cord injury or multiple sclerosis that is not adequately managed with anticholinergic drugs. |
OnabotulinumtoxinA + BSC is associated with a utility benefit that reflects the reduction in the number of UI episodes experienced by patients. |
The addition of onabotulinumtoxinA to BSC for the treatment of adult patients with NDO appears to be a cost-effective intervention in the UK setting, according to the options analysed in the base-case model (base-case incremental cost-effectiveness ratio [ICER] £3,850 per quality-adjusted life-year [QALY] gained). |
The results remained robust, with the ICER remaining below £20,000 per QALY, across all probabilistic sensitivity analyses and sensitivity analyses. |
1 Introduction
Any abnormality in bladder control as a consequence of a neurological disease is generally classified as neuropathic bladder dysfunction. This disorder mainly affects urine storage, particularly in patients who exhibit a loss of upper motor neurone control—for example, in spinal cord injury (SCI) and multiple sclerosis (MS) [1]. Symptoms of impaired urine storage include increased frequency of urination, urinary incontinence (UI) and urgency [1]. Urodynamic assessment is used to confirm the presence of detrusor overactivity, which is termed ‘neurogenic detrusor overactivity’ (NDO) in a population with an underlying neurological condition [2]. NDO has a significant impact on health-related quality of life (HRQoL); patients commonly report detriments in physical function, emotional wellbeing and social relationships [1, 3]. The economic burden of UI due to NDO is substantial [3].
Current best practice is based on National Institute for Health and Care Excellence (NICE) guidelines for the management of UI in neurological disease [1, 4], which recommend behavioural therapy, use of incontinence pads, clean intermittent self-catheterization (CIC) and treatment of adverse events (AEs) [1, 4]. Together, these are classified as best supportive care (BSC). In addition, the use of anticholinergic drugs (ACHDs), onabotulinumtoxinA (BOTOX®, 200 units [200 U]) and augmentation cystoplasty are also recommended as potential treatment options [1, 4]. Many patients fail to improve with ACHDs, either because of lack of efficacy or because they develop AEs (for example, dry mouth, constipation or blurred vision) [5]. High discontinuation rates and interruptions in ACHDs suggest that patients with NDO are not being offered adequate options to manage their UI [6, 7]. Patients whose NDO is not adequately managed with ACHDs, or in whom ACHDs are poorly tolerated, either continue with BSC alone or receive a combination of onabotulinumtoxinA + BSC [1, 4]. Augmentation cystoplasty can be undertaken for refractory patients. This procedure is effective, with good long-term results [8, 9], but is expensive and can have long-term complications [8]. Thus, onabotulinumtoxinA + BSC can become a treatment option for those patients who are refractory to ACHDs [1, 4].
The primary evidence supporting the use of onabotulinumtoxinA + BSC in adults with NDO comes from the pooled intention-to-treat (ITT) population of two pivotal phase III studies (NCT00461292 and NCT00311376; http://www.clinicaltrials.gov) [10, 11]. The pooled population included 468 adults with ≥14 UI episodes/week due to MS (n = 261) or SCI (n = 207), receiving onabotulinumtoxinA 200 U (n = 227) or placebo (n = 241). All patients received BSC. Most baseline characteristics were comparable between the aetiology groups; however, differences included gender (the majority [71 %] of SCI patients were male; the majority [82 %] of MS patients were female), baseline CIC use (SCI: 84.8 %; MS: 29.4 %) and baseline ACHD use (SCI: 60.0 %; MS: 50.7 %) [12]. The results of the clinical trials demonstrated that onabotulinumtoxinA significantly reduced the number of UI episodes and improved urodynamic parameters and quality of life (QoL) relative to placebo. The reduction in the number of UI episodes in patients receiving onabotulinumtoxinA was more than double that observed in placebo-injected patients (mean change from baseline to week 6: −21.3 versus −10.5 episodes [p < 0.001]; from baseline to week 12: −20.6 versus −9.9 episodes [p < 0.001]). QoL, as measured using the Incontinence Quality of Life (I-QOL) questionnaire total score at weeks 6 and 12, was improved threefold in onabotulinumtoxinA-treated patients, compared with those receiving placebo (p < 0.001) [12].
The aim of this economic evaluation was to assess the cost effectiveness, from the perspective of the UK National Health Service (NHS), of onabotulinumtoxinA + BSC compared with BSC alone for the management of UI in adult patients with NDO who are not adequately managed with ACHDs.
2 Methods
An existing Markov model was adapted for the UK [13]. The analysis employed a Markov state-transition model (written in Microsoft Excel© [Redmond, WA, USA]) to estimate the costs per quality-adjusted life-year (QALY) of onabotulinumtoxinA 200 U + BSC for the treatment of UI in patients with NDO (due to MS or SCI), who are not adequately managed on ACHDs, over a 5-year time horizon.
2.1 Data Sources
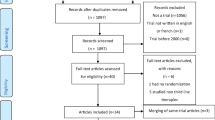
A review of the published literature, using systematic methodology, was conducted.Footnote 1 The following databases were searched (January 2000–February 2011): BIOSIS Preview®, EMBASE®, EMBASE Alert, SciSearch® and MEDLINE®. Relevant terms for the condition (specifically, ‘urinary incontinence due to NDO’) were crossed with outcome concepts, study type concepts and intervention concepts, as appropriate. If evidence from published sources was not available, expert opinion was sought via advisory panel and survey.
2.2 Treatments Modelled
Treatment effect was measured using patient-reported diary data on UI episodes over a 7-day period prior to each study visit. Efficacy and safety estimates of onabotulinumtoxinA and BSC were based on data within the first 12 weeks after treatment initiation from the pooled ITT population from two phase III, randomized, controlled trials (RCTs) [10–12]. Patient-level data files from each of the trials were combined in order to pool the data. Week 12 was the furthest time point after treatment initiation at which randomization integrity was maintained; after this point, the high degree of crossover became problematic for obtaining unbiased estimates (crossover was driven by patient requests for re-treatment) [12].
Patients in the onabotulinumtoxinA arm who responded (≥50 % reduction in weekly UI episodes from baseline) to treatment by week 12 were assumed to be re-treated every 9 months, on the basis of data from the phase III trials [12]. Subsequent treatments with onabotulinumtoxinA were assumed to produce the same duration of effect and efficacy.
Data from the placebo arms of the pooled ITT population from two phase III RCTs were used to approximate BSC treatment in clinical practice. The placebo arms in the phase III trials were deemed appropriate to inform the BSC arm of the model, since all patients who were receiving ACHDs when they started the trial were required to remain on the ACHD at the baseline dose for the remainder of the trial [12]. In addition, they could initiate CIC at the discretion of the physician, and they used incontinence pads as needed [12]. In clinical practice, patients receiving BSC (alone or in combination) may stop, restart, switch or use multiple concomitant ACHDs, and/or titrate to higher doses. Although this was not permitted in the trial, the participants had experienced NDO for some time, and therapy with ACHD was likely to be optimized already [12]. As the placebo in the trial was administered via injection, the efficacy of this placebo injection was likely to have been greater than the efficacy of BSC in actual clinical practice, and this was, thus, considered to be a conservative approach [12].
2.3 Model Structure
2.3.1 Model Design
The modelled treatment pathway incorporated a comparison of onabotulinumtoxinA + BSC with BSC alone. Non-responders would continue to receive BSC and, after 36 weeks, a proportion (5 %) of these were assumed to undergo bladder surgery (augmentation cystoplasty) [14].
The commonly used Markov state-transition approach [15] was selected in favour of individual cycle-level transitions among the health states after week 12, because of difficulties with the high level of crossover in the BSC group in the pivotal studies [12]. A 5-year time horizon, with a model cycle length of 6 weeks, was used in the base case. This time horizon was selected on the basis of data from the two phase III trials and longer-term data suggesting that patients continue to gain benefit from onabotulinumtoxinA with repeated injections [10–12, 16, 17]. Lifetime (60-year) treatment outcomes were assessed in a sensitivity analysis. Outcome measures were QALYs, lifetime costs and incremental cost-effectiveness ratios (ICERs).
The model included six health states based on a reduction in weekly UI episodes, which is commonly used to determine treatment effects in UI: (1) <50 % reduction (non-responders); (2) ≥50–99 % reduction (non-dry responders); (3) 100 % reduction (dry); (4) post-surgery dry (100 % reduction); (5) post-surgery non-dry responders (≥50–99 % reduction); and (6) death. Patients entered the model on day 1 and then cycled among the health states every 6 weeks. It was assumed that all patients could be in only one state at any time. The definition of health states is in line with published literature, whereby a ≥50 % reduction in UI episodes would represent treatment success [10, 11, 16]. Figure 1 shows disease progression in this Markov state-transition model.
Patient-level data were then used to develop transition probabilities for the transitions between baseline, week 6 and week 12 health states for the onabotulinumtoxinA + BSC and BSC arms. The transition was assumed to occur directly after initiation of treatment. Transition probabilities for patients post-surgery were based on publicly available literature [8, 18]. Transitions to the death state were calculated from general population mortality rates in the UK life tables.
A flexible rate of discontinuation was applied in the model, starting from the first onabotulinumtoxinA treatment. In the absence of other available evidence, assumptions regarding annual discontinuation rates were based on the discontinuation rate among responder patients in the pivotal studies (that is, among patients who were treated with onabotulinumtoxinA and responded to treatment [≥50 % reduction in UI episodes] at week 12) and included discontinuations due to lack of efficacy, AEs, pregnancy, and personal or other reasons that may occur in clinical practice (drop-out rates: 5.73 % in the onabotulinumtoxinA group and 11.43 % in the BSC group). This was operationalized in the model in a conservative manner by moving patients from the dry to the non-dry responder health state and by moving patients from the dry and non-dry responder health states to the non-responder health state. Assumptions used around treatment discontinuation were tested in sensitivity analysis.
The analysis was conducted from the perspective of the UK NHS and Personal Social Services, and incorporates utilities and costs associated with receiving treatment for clinical symptoms. All indirect and non-medical costs were excluded from this analysis. All costs included in the cost-effectiveness model were in British pounds sterling (£), and costs and benefits beyond the first year were discounted annually at a rate of 3.5 %, in accordance with methods guidance from NICE [19].
2.3.2 Model Validation
Internal validity was evaluated by subjecting the model to thorough debugging, using null and extreme input values, and a detailed review of all mathematical formulas and coding by both internal and external reviewers. External validation of model inputs and assumptions was gained via an advisory board panel, comprising seven members (clinicians, pharmacists and policy makers). The panel reviewed the clinical and economic data and related assumptions for relevance and their validity in clinical practice.
2.4 Model Parameters
All key parameters are summarized in Table 1.
2.4.1 Adverse Events
Urinary tract infections (UTIs; symptomatic and asymptomatic) were modelled as AEs. The UTI rate was estimated from the phase III trials [12] as an event rate per patient-year at week 12 (placebo-controlled data), taking into account the total number of UTIs from baseline to week 12. Standard error (SE) was calculated using the bootstrap method with a sample of 1,000. The mean number of UTIs per model cycle was determined by dividing the mean yearly rate by 8.
2.4.2 Utilities
The EuroQol Five Dimensions (EQ-5D) and Short Form 36 (SF-36) questionnaires were administered in the pivotal studies at baseline and on study exit only; therefore, these utility values could not be used in the model. Consequently, utility values for the model were derived from the I-QOL questionnaire [20], which was administered in the pivotal studies [12]. A two-stage process was used to develop the condition-specific Incontinence Utility Index from the I-QOL questionnaire and its neurogenic model [21].
The utility values correspond with treatment and response status (Table 1). Because of the lack of available literature reporting utilities associated with the health states post-surgery, post-surgery dry and non-dry responders were assumed to have the same utilities as dry and non-dry responders, respectively.
Time-dependent weighting of the utility scores for responding patients in both groups allowed the data from the entire course of the trial to be modelled and allowed the relevant impact on QALYs to be captured. This weighting was related to the possible loss of efficacy over time that was experienced by patients in the onabotulinumtoxinA 200 U group and that would precede the request for re-treatment, and the loss of placebo effect in the comparator arm. The distribution of patients within each health state at weeks 6 and 12 was taken from the pivotal studies to inform the utilities at these time points. In order to inform the rate of subsequent degradation, the weighted average of the health state distributions at weeks 18, 24, 30 and 36 was used to calculate the average utility for each cohort up to the mean time to request re-treatment. Given the mean time to re-treatment of nine months (8.94) in patients who respond to onabotulinumtoxinA at week 12, week 36 was selected to accommodate a model cycle duration of 6 weeks.
Disutilities due to AEs from drug treatment were not modelled, because of the limited evidence in the NDO population. AEs were, therefore, accounted for in the model only in terms of costs.
2.4.3 Resource Use and Costs
Resource use data were derived from the studies as far as possible and supplemented with values from a literature review. However, as published data were not available for both the proportion of non-responding patients receiving augmentation cystoplasty and the number of additional physician visits for treating UI, these estimates were validated via an advisory board panel.
The cost of treatment in the onabotulinumtoxinA arm of the model included the per-unit cost of onabotulinumtoxinA (200 U vial: £276.40) and consultant time to administer the injection (see Table 2) [22, 23]. On the basis of the mean time to request re-treatment from the phase III trials (8.94 months), responders were assumed to receive re-treatment, on average, every 9 months. BSC treatment was not associated with any intervention costs.
Resource use and costs associated with UI and management of AEs were applied to both the onabotulinumtoxinA and BSC arms. Resource use (use of ACHDs, use of incontinence pads, drug administration, use of CIC and treatment of UTIs with antibiotics) was estimated from the two phase III trials. Other resource use was estimated using results from a qualitative survey of UK specialist physicians (details are provided in Online Resource 1 in the Electronic Supplementary Material).
Resource use and costs associated with surgical intervention included the cost of surgery. Given the limited evidence on AEs associated with augmentation cystoplasty in patients with NDO, these were not taken into account in the base-case analysis.
2.5 Sensitivity Analyses
One-way sensitivity analyses and probabilistic sensitivity analyses (PSAs) were performed by varying effectiveness, utility and cost parameters.
Parameter uncertainty was assessed in a PSA [24]. Beta distributions were fitted for patient distributions and health-related utility data; gamma distributions were fitted for all cost parameters; and normal distributions were fitted to sample mean frequency estimates (for example, mean number of UI episodes, physician visits). Each point estimate was associated with a respective SE. Where the SE was not available, a variation of ±10 % was assumed. Values used in the PSA were derived by random sampling from respective distributions. PSA results were generated from 1,000 iterations. Distribution parameters, as well as probabilistic values from one random sampling, are provided in Online Resource 2 in the Electronic Supplementary Material.
A range of scenario analyses were conducted to account for the uncertainty of cost effectiveness associated with assumptions relating to clinical practice, costs and estimates of the value of health outcomes.
3 Results
The onabotulinumtoxinA + BSC group incurs lower healthcare resource utilization than the BSC group. A smaller number of UI episodes in the onabotulinumtoxinA + BSC group means reduced use of incontinence pads and fewer physician visits, compared with the BSC group. Corresponding with the reduced resource utilization, healthcare costs are reduced with the onabotulinumtoxinA + BSC group over the 5-year time horizon. Resource utilization and disaggregated costs for the base-case analyses are provided in Table 3, and estimates of total costs per health state (per patient) at year 5 are provided in Table 4. Over the 5-year time horizon, it is estimated that a mean of 516 UI episodes (per person-year) would be avoided at a cost of £3 per episode.
Over a 5-year time horizon, treatment with onabotulinumtoxinA + BSC was associated with an increase in costs of £1,689 (£8,735 versus £7,046) and an increase of 0.4388 in discounted QALYs gained (1.7236 versus 1.2848) compared with BSC alone. These results generated an ICER of £3,850 per QALY gained (Table 5).
3.1 Scenario Analyses
Scenario analyses are presented in Table 6. Results from the scenario analyses indicate that the ICER is sensitive to a shorter time horizon; a reduced number of urologist attendances by non-responders; a shorter mean time interval between requests for onabotulinumtoxinA re-treatment; the rate of utility degradation related to onabotulinumtoxinA re-treatment; and adopting one urodynamic assessment for non-responders and non-dry responders subsequent to initial treatment. All of these analyses increased the ICER relative to the base case to more than £4,000. For other analyses (Table 6), the ICER did not exceed £4,000. No scenario exceeded the willingness-to-pay threshold of £20,000/QALY.
3.1.1 Underlying Condition: Spinal Cord Injury or Multiple Sclerosis
Given the difference in the cause of NDO between MS and SCI patients, it was assumed that each would incur different resource uses and hence costs for the management of NDO. In addition, analyses of the pivotal trials show a difference in time to request re-treatment between MS and SCI patients (the mean re-treatment intervals are 9.224 months and 8.532 months for MS and SCI patients, respectively). These re-treatment intervals were used in the subgroup analyses.
For the 5-year time horizon, onabotulinumtoxinA + BSC compared with BSC alone yielded an ICER of £6,422/QALY and £1,767/QALY for MS and SCI, respectively. Although similar findings were noted for both aetiologies in terms of improved QALYs, total costs in both treatment groups were considerably higher for the SCI population than for the MS population. This was mainly driven by higher costs associated with greater CIC use in SCI patients in both the onabotulinumtoxinA + BSC and BSC groups. Despite this, lower incremental costs for SCI compared with MS resulted in a lower ICER for SCI.
3.2 Sensitivity Analyses
One-way sensitivity analyses were applied to the model in order to ascertain the cost effectiveness of onabotulinumtoxinA + BSC. Variations in assumptions regarding costs and outcomes were examined in order to establish the key drivers of the model and to verify the robustness of the primary results. Sensitivity analyses involving health outcomes and cost variables are shown in Fig. 2. Cost effectiveness was sensitive to the utility values used for the health states. As there is no benefit from reduced mortality, all QALY gains result from improvements in HRQoL as a result of fewer weekly UI episodes. The results also indicated that the main drivers of cost in the model are mean CIC and treatment administration costs. PSA indicated that, at a willingness to pay of £20,000 per QALY, onabotulinumtoxinA has a 100 % probability of being cost effective (Figs. 3, 4).
4 Discussion
The model presented here, which is adapted from the US model by Carlson et al. [13], assessed the cost effectiveness of onabotulinumtoxinA + BSC versus BSC alone for the treatment of UI in adult patients with NDO (due to SCI or MS) who are not adequately managed on ACHDs in the UK. In the base-case analysis, onabotulinumtoxinA + BSC represented a cost-effective alternative compared with BSC alone, at a cost of £3,850 per QALY gained. In the absence of long-term data, best possible assumptions were made. Uncertainty surrounding these assumptions was tested in PSA and scenario analyses. PSA demonstrated that, at a willingness to pay of £20,000/QALY gained, onabotulinumtoxinA has a 100 % probability of being cost effective; this remained robust in scenario analyses. The model was assessed by the All Wales Medicines Strategy Group (AWMSG) and the Scottish Medicines Consortium (SMC), who both accepted onabotulinumtoxinA 200 U for use within this population [25, 26]. The results are also in agreement with a cost-consequence study conducted from a UK NHS perspective, which concluded that onabotulinumtoxinA was cost effective in both idiopathic and neurogenic disease [27].
Although onabotulinumtoxinA is cost effective in both the MS and SCI subgroups, the clinical benefits and costs differ by aetiology. The model suggested that the cost effectiveness was greatest for SCI patients receiving onabotulinumtoxinA + BSC, yielding an ICER of £1,767. For MS, similar findings were noted with respect to a reduction in the number of UI episodes and improved QALYs; however, higher incremental costs resulted in an ICER of £6,422. The profile of the SCI population is the main driver of this difference in outcomes—a higher rate of CIC use in the BSC arm means that the incremental cost of CIC use in the onabotulinumtoxinA arm of the model is lower.
As the phase III trials were international, multicentre studies, clinical results would be expected to be generalizable to other countries. The rates of resource utilization and costs, however, may need adapting in order to be relevant to other countries.
This cost-effectiveness analysis has some limitations. There are no relevant active comparators for onabotulinumtoxinA, because patients comprising the target population have already failed on conservative pharmacotherapy with ACHDs but have not yet undergone more invasive procedures. For these patients, the treatment choices are to continue with BSC alone or to add onabotulinumtoxinA to BSC. Continued management with BSC was, therefore, considered to be the appropriate clinical comparator for the purposes of this economic analysis. In the trials, patients continued on ACHDs (if used at baseline), catheters and incontinence pads. The placebo arm achieved results that may not be matched in clinical practice, with almost 40 % of patients achieving a >50 % reduction in UI at 12 weeks [14]. This model assumes that the efficacy of BSC in clinical practice is similar to the efficacy of placebo injections in the pooled BSC groups from the trials. As the placebo in the trial was an injection, this was likely to have been greater than the efficacy of BSC in actual clinical practice and, as such, it was considered to be a conservative approach.
Utility values used in this model ranged from 0.240 to 0.562. The values were generated directly from the disease-specific I-QOL questionnaire by eliciting preferences directly from a UK population. Eliciting preferences from a condition-specific measure was favoured because mapping algorithms (such as I-QOL to EQ-5D) have been found to have poor predictive validity due to little overlap in the classification systems of the condition-specific and generic measures. The estimated mean utilities are in line with published evidence indicating that utility in MS patients was in the range of 0.1–0.92 [28], and that utility in the SCI population was in the range of 0.394–0.667 [29]. In addition, differences between incontinent and continent (i.e. dry) states correspond to those in previously published models, which have reported such utility differences ranging from 0.19 to 0.33 [30–34]. Scenario analyses, based on published utility estimates of 0.66–0.78 [35] and of 0.19–0.33 (obtained from studies in patients with overactive bladder/UI) [30–34], increase the ICER; however, onabotulinumtoxinA + BSC still maintains its cost effectiveness in line with the NICE threshold at £20,000 per QALY gained.
The most common AEs observed in the trials were UTIs. These were identified as being important because of the clinical relationship with the rates of UI episodes [1, 36]. The model includes UTIs at week 12 of the clinical trials. AEs were accounted for in the model only in terms of costs; no disutility was applied, given the limited evidence in the NDO population. In addition, as disutilities were embedded in the trial data used to generate the health state utilities, they were not included in the model, to avoid double counting. It should be noted that the trial definition of UTI was conservatively based on urinalysis and microscopy and not on clinical symptoms. As the latter were not recorded, it is not possible to say what proportion of UTIs found in the trial would be classified as UTIs in clinical practice, but it is likely that it would be <100 %, as asymptomatic bacteriuria or leukocyturia are common, especially in patients using CIC.
Finally, efficacy and safety assumptions were based on a pooled study dataset (ITT) within the first 12 weeks after treatment initiation. This time point was the furthest after treatment initiation at which randomization integrity was maintained—that is, no crossover from the BSC group to the onabotulinumtoxinA + BSC group. After week 12, patients in the studies were allowed to receive re-treatment if they requested it at any subsequent visit, provided that they met the re-treatment criteria. Therefore, beyond week 12, the trial population would consist of a mixture of patients who had had one or more treatments. Week 12, therefore, represents the most valid time point for comparing the efficacy of the two treatment options; these data were extrapolated to a 5-year time horizon. To allow extrapolation beyond this short-time horizon, long-term efficacy data for onabotulinumtoxinA are needed.
5 Conclusion
OnabotulinumtoxinA + BSC is associated with a utility benefit that is reflected in the reduction in the number of UI episodes experienced by patients. For adult patients with NDO who are not adequately managed with ACHDs, onabotulinumtoxinA + BSC, at £20,000/QALY, appears to be a cost-effective use of resources in the UK NHS.
Notes
Further details of the literature review that was completed are available from the corresponding author on request.
References
National Institute for Health and Care Excellence. Clinical guideline 148: urinary incontinence in neurological disease. London: NICE; 2012.
Abrams P, Andersson KE, Birder L, Brubaker L, Cardozo L, Chapple C, et al. Fourth International Consultation on Incontinence Recommendations of the International Scientific Committee: evaluation and treatment of urinary incontinence, pelvic organ prolapse, and fecal incontinence. Neurourol Urodyn. 2010;29:213–40.
Tapia CI, Khalaf K, Berenson K, Globe D, Chancellor M, Carr LK. Health-related quality of life and economic impact of urinary incontinence due to detrusor overactivity associated with a neurologic condition: a systematic review. Health Qual Life Outcomes. 2013;11:13.
National Institute for Health and Care Excellence. NICE pathways: treatment to improve bladder storage in people with neurological disease. London: NICE; 2013.
Haab F, Castro-Diaz D. Persistence with antimuscarinic therapy in patients with overactive bladder. Int J Clin Pract. 2005;59:931–7.
Manack A, Motsko SP, Haag-Molkenteller C, Dmochowski RR, Goehring EL Jr, Nguyen-Khoa BA, et al. Epidemiology and healthcare utilization of neurogenic bladder patients in a US claims database. Neurourol Urodyn. 2010;30:395–401.
Lawrence M, Guay DR, Benson SR, Anderson MJ. Immediate-release oxybutynin versus tolterodine in detrusor overactivity: a population analysis. Pharmacotherapy. 2000;20:470–5.
Gurung PM, Attar KH, Abdul-Rahman A, Morris T, Hamid R, Shah PJ. Long-term outcomes of augmentation ileocystoplasty in patients with spinal cord injury: a minimum of 10 years of follow-up. BJU Int. 2012;109:1236–42.
Chartier-Kastler EJ, Mongiat-Artus P, Bitker MO, Chancellor MB, Richard F, Denys P. Long-term results of augmentation cystoplasty in spinal cord injury patients. Spinal Cord. 2000;38:490–4.
Cruz F, Herschorn S, Aliotta P, Brin M, Thompson C, Lam W, et al. Efficacy and safety of onabotulinumtoxinA in patients with urinary incontinence due to neurogenic detrusor overactivity: a randomised, double-blind, placebo-controlled trial. Eur Urol. 2011;60:742–50.
Ginsberg D, Gousse A, Keppenne V, Sievert KD, Thompson C, Lam W, et al. Phase 3 efficacy and tolerability study of onabotulinumtoxinA for urinary incontinence from neurogenic detrusor overactivity. J Urol. 2012;187:2131–9.
Ginsberg D, Cruz F, Herschorn S, Gousse A, Keppenne V, Aliotta P, et al. OnabotulinumtoxinA is effective in patients with urinary incontinence due to neurogenic detrusor activity regardless of concomitant anticholinergic use or neurologic etiology. Adv Ther. 2013;30:819–33.
Carlson JJ, Hansen RN, Dmochowski RR, Globe DR, Colayco DC, Sullivan SD. Estimating the cost-effectiveness of onabotulinumtoxinA for neurogenic detrusor overactivity in the United States. Clin Ther. 2013;35:414–24.
All Wales Medicines Strategy Group Secretariat assessment report. Botulinum toxin type A (Botox) (50 units, 100 units, 200 units powder for solution for injection): reference number 1429 (full submission). Cardiff: All Wales Medicines Strategy Group; 2013.
Sonnenberg FA, Beck JR. Markov models in medical decision making a practical guide. Med Decision Making. 1993;13:322–38.
Giannantoni A, Mearini E, Del Zingaro M, Porena M. Six-year follow-up of botulinum toxin A intradetrusorial injections in patients with refractory neurogenic detrusor overactivity: clinical and urodynamic results. Eur Urol. 2009;55:705–11.
Khan S, Game X, Kalsi V, Gonzales G, Panicker J, Elneil S, et al. Long-term effect on quality of life of repeat detrusor injections of botulinum neurotoxin-A for detrusor overactivity in patients with multiple sclerosis. J Urol. 2011;185:1344–9.
Herschorn S, Hewitt RJ. Patient perspective of long-term outcome of augmentation cystoplasty for neurogenic bladder. Urology. 1998;52:672–8.
National Institute for Health and Care Excellence. Guide to the methods of technology appraisal 2013—NICE guidance. London: NICE; 2013.
Schurch B, Denys P, Kozma CM, Reese PR, Slaton T, Barron R. Reliability and validity of the Incontinence Quality of Life questionnaire in patients with neurogenic urinary incontinence. Arch Phys Med Rehabil. 2007;88:646–52.
Cuervo J, Castejon N, Khalaf KM, Waweru C, Globe D, Patrick DL. Development of the Incontinence Utility Index: estimating population-based utilities associated with urinary problems from the Incontinence Quality of Life questionnaire and Neurogenic Module. Health Qual Life Outcomes. 2014;12:147.
British Medical Association. British national formulary: No 65. British Medical Association and Royal Pharmaceutical Society of Great Britain; 2013.
Department of Health. NHS reference costs 2011–2012. London: Department of Health; 2013.
Briggs AH, Weinstein MC, Fenwick EA, Karnon J, Sculpher MJ, Paltiel AD. Model parameter estimation and uncertainty: a report of the ISPOR-SMDM Modeling Good Research Practices Task Force-6. Value Health. 2012;15:835–42.
Scottish Medicines Consortium. Detailed advice document: botulinum toxin type A 50, 100, 200 Allergan units/vial (Botox®): SMC # 916/13. Glasgow: Scottish Medicines Consortium; 2013.
All Wales Medicines Strategy Group Secretariat assessment report. Botulinum toxin type A (Botox) (50 units, 100 units, 200 units powder for solution for injection): reference number 1429 (Advice). Cardiff: All Wales Medicines Strategy Group; 2013.
Kalsi V, Popat RB, Apostolidis A, Kavia R, Odeyemi IA, Dakin HA, et al. Cost-consequence analysis evaluating the use of botulinum neurotoxin-A in patients with detrusor overactivity based on clinical outcomes observed at a single UK centre. Eur Urol. 2006;49:519–27.
Naci H, Fleurence R, Birt J, Duhig A. The impact of increasing neurological disability of multiple sclerosis on health utilities: a systematic review of the literature. J Med Econ. 2010;13:78–89.
Dijkers MP. Quality of life of individuals with spinal cord injury: a review of conceptualization, measurement, and research findings. J Rehabil Res Dev. 2005;42:87–110.
Arlandis S, Castro D, Errando C, Fernandez E, Jimenez M, Gonzalez P, et al. Cost-effectiveness of sacral neuromodulation compared to botulinum neurotoxin A or continued medical management in refractory overactive bladder. Value Health. 2011;14:219–28.
Lichstein JC, Biddle AK, Lavelle J. Cost-utility analysis of sacral nerve stimulation and botulinum-A for the treatment of urinary urge incontinence in women 65 and older. UroToday Int J. 2008;1(1 Suppl):9.
Schultz SE, Kopec JA. Impact of chronic conditions. Health Rep. 2003;14:41–53.
Siddiqui NY, Amundsen CL, Visco AG, Myers ER, Wu JM. Cost-effectiveness of sacral neuromodulation versus intravesical botulinum A toxin for treatment of refractory urge incontinence. J Urol. 2009;182:2799–804.
Wu JM, Siddiqui NY, Amundsen CL, Myers ER, Havrilesky LJ, Visco AG. Cost-effectiveness of botulinum toxin a versus anticholinergic medications for idiopathic urge incontinence. J Urol. 2009;181:2181–6.
Hollingworth W, Campbell JD, Kowalski J, Ravelo A, Girod I, Briggs A, et al. Exploring the impact of changes in neurogenic urinary incontinence frequency and condition-specific quality of life on preference-based outcomes. Qual Life Res. 2010;19:323–31.
Clinical key: urinary incontinence. Elsevier; http://www.clinicalkey.com/topics/urology/urinary-incontinence.html. Accessed 27 Jan 2014.
Acknowledgments
This study was funded by Allergan Limited (UK). SS and DG, employees of the LA-SER Group, were contracted by Allergan Limited to develop the model. At the time of study design and data analyses, CL, JM, CC, DC and DGl were employees of Allergan Limited. RH is an investigator for clinical studies funded by Allergan Limited and has been an invited speaker for Allergan Limited. All authors participated in drafting, critical revision and finalization of the manuscript. Medical writing and editorial support were provided by Hayward Medical Communications.
Author information
Authors and Affiliations
Corresponding author
Electronic Supplementary Material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and the source are credited.
About this article
Cite this article
Hamid, R., Loveman, C., Millen, J. et al. Cost-Effectiveness Analysis of OnabotulinumtoxinA (BOTOX®) for the Management of Urinary Incontinence in Adults with Neurogenic Detrusor Overactivity: A UK Perspective. PharmacoEconomics 33, 381–393 (2015). https://doi.org/10.1007/s40273-014-0245-8
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40273-014-0245-8