Abstract
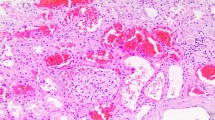
Anticoagulant-related nephropathy, a recently recognized entity, manifests as unexplained acute kidney injury in the setting of excessive anticoagulation with oral agents. Histologic findings in warfarin-related nephropathy include glomerular hemorrhage and renal tubular obstruction by red blood cells. Affected patients are at increased risk of mortality as well as irreversible kidney injury. Patients with chronic kidney disease are particularly vulnerable to this complication. Similar case reports of anticoagulant-related nephropathy have been linked to the more novel oral anticoagulant, dabigatran. Anticoagulant-related nephropathy has been successfully reproduced in rat models. These animal models shed light on the pathogenesis of the disease including the potential role of direct thrombin and protease-activated receptor-1 inhibition. Warfarin and dabigatran also cause an increase in systolic blood pressure in rats, a risk factor for developing nephropathy. This article reviews the current evidence for anticoagulant-related nephropathy and provides data for the suggested possible mechanisms underlying this adverse effect.

Similar content being viewed by others
References
Brodsky SV, Nadasdy T, Rovin BH, Satoskar AA, Nadasdy GM, Wu HM, et al. Warfarin-related nephropathy occurs in patients with and without chronic kidney disease and is associated with an increased mortality rate. Kidney Int. 2011;80(2):181–9.
Rizk DV, Warnock DG. Warfarin-related nephropathy: another newly recognized complication of an old drug. Kidney Int. 2011;80(2):131–3.
Limdi NA, Limdi MA, Cavallari L, Anderson AM, Crowley MR, Baird MF, et al. Warfarin dosing in patients with impaired kidney function. Am J Kidney Dis. 2010;56(5):823–31.
Di Maso V, Carraro M, Bevilacqua E, Bucconi S, Artero ML, Boscutti G. Warfarin-related nephropathy: possible role for the warfarin pharmacogenetic profile. Clin Kidney J. 2014;7(6):605–8.
Franco V, Polanczyk CA, Clausell N, Rohde LE. Role of dietary vitamin K intake in chronic oral anticoagulation: prospective evidence from observational and randomized protocols. Am J Med. 2004;116(10):651–6.
Ellis RJ, Mayo MS, Bodensteiner DM. Ciprofloxacin-warfarin coagulopathy: a case series. Am J Hematol. 2000;63(1):28–31.
Nemoto C, Ikegami Y, Shimada J, Tsukada Y, Abe Y, Tase C. Acute renal failure caused by severe coagulopathy induced by the interaction between warfarin potassium and levofloxacin: a case report. J Anesth. 2012;26(6):943–4.
Oake N, Fergusson DA, Forster AJ, van Walraven C. Frequency of adverse events in patients with poor anticoagulation: a meta-analysis. CMAJ. 2007;176(11):1589–94.
Yang E. A clinician’s perspective: novel oral anticoagulants to reduce the risk of stroke in nonvalvular atrial fibrillation—full speed ahead or proceed with caution? Vasc Health Risk Manag. 2014;10:507–22.
Rui P, Erik Lerkevang G, Steen H, Sergio B, Serge B, Joao M. A meta-analysis of phase III randomized controlled trials with novel oral anticoagulants in atrial fibrillation: comparisons between direct thrombin inhibitors vs. factor Xa inhibitors and different dosing regimens. Thromb Res. 2014;134(6):1253–64.
Bacchus F, Schulman S. Clinical experience with the new oral anticoagulants for treatment of venous thromboembolism. Arterioscler Thromb Vasc Biol. 2015;35(3):513–9.
Deal EN, Pope H, Ross W. Apixaban use among patients with severe renal impairment. Ann Pharmacother. 2014;48(12):1667.
Guyatt GH, Akl EA, Crowther M, Gutterman DD, Schuunemann HJ. Executive summary: antithrombotic therapy and prevention of thrombosis, 9th ed: American College of Chest Physicians Evidence-Based Clinical Practice Guidelines. Chest. 2012;141(2 Suppl):7s–47s.
Poulsen BK, Grove EL, Husted SE. New oral anticoagulants: a review of the literature with particular emphasis on patients with impaired renal function. Drugs. 2012;72(13):1739–53.
Dempfle C-E. Direct oral anticoagulants: pharmacology, drug interactions, and side effects. Semin Hematol. 2014;51(2):89–97.
Shafi ST, Negrete H, Roy P, Julius CJ, Sarac E. A case of dabigatran-associated acute renal failure. WMJ. 2014;112:173–5.
Ryan M, Ware K, Qamri Z, Satoskar A, Wu H, Nadasdy G, et al. Warfarin-related nephropathy is the tip of the iceberg: direct thrombin inhibitor dabigatran induces glomerular hemorrhage with acute kidney injury in rats. Nephrol Dial Transplant. 2014;29(12):2228–34.
Ozcan A, Ware K, Calomeni E, Nadasdy T, Forbes R, Satoskar A, et al. 5/6 nephrectomy as a validated rat model mimicking human warfarin-related nephropathy. Am J Nephrol. 2012;35(4):356–64.
Ware K, Brodsky P, Satoskar AA, Nadasdy T, Nadasdy G, Wu H, et al. Warfarin-related nephropathy modeled by nephron reduction and excessive anticoagulation. J Am Soc Nephrol. 2011;22(10):1856–62.
Ware KM, Vance JC, Muni N, Hebert LA, Satoskar AA, Nadasdy G, et al. Oral warfarin and the thrombin inhibitor dabigatran increase blood pressure in rats: hidden danger of anticoagulants? Am J Hypertens. 2015;28(2):182–9.
An JN, Ahn SY, Yoon CH, Youn TJ, Han MK, Kim S, et al. The occurrence of warfarin-related nephropathy and effects on renal and patient outcomes in korean patients. PLoS One. 2013;8(4):e57661.
Brodsky SV, Collins M, Park E, Rovin BH, Satoskar AA, Nadasdy G, et al. Warfarin therapy that results in an International Normalization Ratio above the therapeutic range is associated with accelerated progression of chronic kidney disease. Nephron Clin Pract. 2010;115(2):c142–6.
Lim AK, Campbell DA. Haematuria and acute kidney injury in elderly patients admitted to hospital with supratherapeutic warfarin anticoagulation. Int Urol Nephrol. 2013;45(2):561–70.
Santos C, Gomes AM, Ventura A, Almeida C, Seabra J. An unusual cause of glomerular hematuria and acute kidney injury in a chronic kidney disease patient during warfarin therapy. Nefrologia. 2013;33(3):400–3.
Brodsky SV, Satoskar A, Chen J, Nadasdy G, Eagen JW, Hamirani M, et al. Acute kidney injury during warfarin therapy associated with obstructive tubular red blood cell casts: a report of 9 cases. Am J Kidney Dis. 2009;54(6):1121–6.
Abt AB, Carroll LE, Mohler JH. Thin basement membrane disease and acute renal failure secondary to gross hematuria and tubular necrosis. Am J Kidney Dis. 2000;35(3):533–6.
Kabir A, Nadasdy T, Nadasdy G, Hebert LA. An unusual cause of gross hematuria and transient ARF in an SLE patient with warfarin coagulopathy. Am J Kidney Dis. 2004;43(4):757–60.
Brodsky SV. Anticoagulants and acute kidney injury: clinical and pathology considerations. Kidney Res Clin Pract. 2014;33(4):174–80.
Limdi NA, Beasley TM, Baird MF, Goldstein JA, McGwin G, Arnett DK, et al. Kidney function influences warfarin responsiveness and hemorrhagic complications. J Am Soc Nephrol. 2009;20(4):912–21.
Limdi NA, Nolin TD, Booth SL, Centi A, Marques MB, Crowley MR, et al. Influence of kidney function on risk of supratherapeutic international normalized ratio-related hemorrhage in warfarin users: a prospective cohort study. Am J Kidney Dis. 2014. (Article in press).
Homsi E, Janino P, de Faria JB. Role of caspases on cell death, inflammation, and cell cycle in glycerol-induced acute renal failure. Kidney Int. 2006;69(8):1385–92.
Patel RP, Svistunenko DA, Darley-Usmar VM, Symons MC, Wilson MT. Redox cycling of human methaemoglobin by H2O2 yields persistent ferryl iron and protein based radicals. Free Radical Res. 1996;25(2):117–23.
Tracz MJ, Alam J, Nath KA. Physiology and pathophysiology of heme: implications for kidney disease. J Am Soc Nephrol. 2007;18(2):414–20.
Ware K, Qamri Z, Ozcan A, Satoskar AA, Nadasdy G, Rovin BH, et al. N-Acetylcysteine ameliorates acute kidney injury but not glomerular hemorrhage in an animal model of warfarin-related nephropathy. Am J Physiol Renal Physiol. 2013;304(12):F1421–7.
Chang CC, Liou HH, Wu CL, Chang CB, Chang YJ, Chiu PF, et al. Warfarin slows deterioration of renal function in elderly patients with chronic kidney disease and atrial fibrillation. Clin Interv Aging. 2013;8:523–9.
Yanagita M. Gas6, warfarin, and kidney diseases. Clin Exp Nephrol. 2004;8(4):304–9.
Kapoor KG, Bekaii-Saab T. Warfarin-induced allergic interstitial nephritis and leucocytoclastic vasculitis. Intern Med J. 2008;38(4):281.
Leven C, Hudier L, Picard S, Longuet H, Lorcy N, Cam G, et al. Prospective study of drug-induced allergic nephropathy in eleven French nephrology units. Presse medicale (Paris, France: 1983). 2014;43:e369–76.
Hsu C-Y, Chen W-S, Sung S-H. Warfarin-induced leukocytoclastic vasculitis: a case report and review of literature. Intern Med. 2012;51(6):601–6.
Moll S, Huffman J. Cholesterol emboli associated with warfarin treatment. Am J Hematol. 2004;77(2):194–5.
Gultekin N, Akin F, Kucukates E. Warfarin-induced bilateral renal hematoma causing acute renal failure. Turk Kardiyoloji Dernegi arsivi: Turk Kardiyoloji Derneginin yayin organidir. 2011;39(3):228–30.
Kadiyala D, Brewster UC, Moeckel GW. Dabigatran induced acute kidney injury. In: The American Society of Nephrology annual meeting, November 1–4, 2012, San Diego, CA; 2012. p. FR-PO1122.
Perez A, Eraso LH, Merli GJ. Implications of new anticoagulants in primary practice. Int J Clin Pract. 2013;67(2):139–56.
Bachellerie B, Ruiz S, Conil JM, Crognier L, Seguin T, Georges B, et al. Patient with acute renal injury presenting dabigatran overdose: hemodialysis for surgery. Ann Fr Anesth Reanim. 2014;33(1):44–6.
Fountzilas C, George J, Levine R. Dabigatran overdose secondary to acute kidney injury and amiodarone use. NZ Med J. 2013;126(1370):110–2.
Maddry JK, Amir MK, Sessions D, Heard K. Fatal dabigatran toxicity secondary to acute renal failure. Am J Emerg Med. 2013;31(2):462.e1–2.
Wychowski MK, Kouides PA. Dabigatran-induced gastrointestinal bleeding in an elderly patient with moderate renal impairment. Ann Pharmacother. 2012;46(4):e10.
Mantha S, Cabral K, Ansell J. New avenues for anticoagulation in atrial fibrillation. Clin Pharmacol Ther. 2013;93(1):68–77.
Coughlin SR. Protease-activated receptors in hemostasis, thrombosis and vascular biology. J Thromb Haemost. 2005;3(8):1800–14.
Coughlin SR. Protease-activated receptors in vascular biology. Thromb Haemost. 2001;86(1):298–307.
Carlile-Klusacek M, Rizzo V. Endothelial cytoskeletal reorganization in response to PAR1 stimulation is mediated by membrane rafts but not caveolae. Am J Physiol Heart Circ Physiol. 2007;293(1):H366–75.
Krishnan S, Chawla N, Ezekowitz MD, Peixoto AJ. Warfarin therapy and systolic hypertension in men with atrial fibrillation. Am J Hypertens. 2005;18(12 Pt 1):1592–9.
Sergey V, Brodsky M, BH Rovin, LA Hebert. Anticoagulant-related nephropathy. In: UpToDate, Post TW, editor, UpToDate, Waltham; 2015. http://www.uptodate.com/contents/anticoagulant-related-nephropathy. Accessed 15 Feb 2015.
Funding and conflict of interest
No sources of funding were used to assist in the preparation of this article. Vinay Narasimha Krishna, David G. Warnock, Nakshatra Saxena, and Dana V. Rizk have no conflicts of interest that are directly relevant to the content of this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Narasimha Krishna, V., Warnock, D.G., Saxena, N. et al. Oral Anticoagulants and Risk of Nephropathy. Drug Saf 38, 527–533 (2015). https://doi.org/10.1007/s40264-015-0290-z
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-015-0290-z