Abstract
Purpose of Review
This review discusses the special considerations in the care of pregnant patients with congenital heart disease (CHD) to minimize obstetric risks and avoid cardiac complications.
Recent Findings
Multidisciplinary team planning is a cornerstone in the care of patients with CHD in pregnancy. Most patients with CHD should have neuraxial anesthesia and laboratory monitoring during labor and delivery, but the need for pulse oximetry, telemetry, and invasive hemodynamic monitoring should be individualized based on patient risk. Additionally, most patients with CHD can safely have a vaginal delivery at 39–40 weeks without additional maternal morbidity. Cesarean delivery should be reserved for typical obstetric indications with some exceptions.
Summary
With thoughtful multidisciplinary team management, pregnancy and labor can be well tolerated in those with congenital heart disease. There are some congenital cardiac lesions that require invasive cardiac monitoring and/or consideration of delivery in a cardiac care unit.

Similar content being viewed by others
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
Thompson JL, Kuklina EV, Bateman BT, Callaghan WM, James AH, Grotegut CA. Medical and obstetric outcomes among pregnant women with congenital heart disease. Obstetrics Gynecol. 2015;126:346–54.
Pfaller B, Sathananthan G, Grewal J, Mason J, D’Souza R, Spears D, Kiess M, Siu SC, Silversides CK. Preventing complications in pregnant women with cardiac disease. J Am Coll Cardiol. 2020;75:1443–52.
Silversides CK, Grewal J, Mason J, Sermer M, Kiess M, Rychel V, Wald RM, Colman JM, Siu SC. Pregnancy outcomes in women with heart disease: the CARPREG II Study. J Am Coll Cardiol. 2018;71:2419–30.
Greutmann M, Pieper PG. Pregnancy in women with congenital heart disease. Eur Heart J. 2015;36:2491–9.
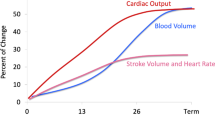
Sanghavi M, Rutherford JD. Cardiovascular physiology of pregnancy. Circulation. 2014;130:1003–8.
Hunter S, Robson SC. Adaptation of the maternal heart in pregnancy. Brit Heart J. 1992;68:540.
Silversides CK, Marelli A, Beauchesne L, et al. Canadian Cardiovascular Society 2009 Consensus Conference on the management of adults with congenital heart disease: Executive summary. Can J Cardiol. 2010;26:143–150.
Easter SR, Valente AM, Economy KE. Creating a multidisciplinary pregnancy heart team. Curr Treat Options Cardiovasc Medicine. 2020;22:3.
European Heart Journal. 2018;39:3165–3241. https://doi.org/10.1093/eurheartj/ehy340 Downloaded from https://academic.oup.com/eurheartj/article/39/34/3165/5078465 by guest on 19 March 2023.
Sharma G, Ying W, Silversides CK. The importance of cardiovascular risk assessment and pregnancy heart team in the management of cardiovascular disease in pregnancy. Cardiol Clin. 2021;39:7–19.
Sarma AA, Aggarwal NR, Briller JE, et al. The utilization and interpretation of cardiac biomarkers during pregnancy. JACC: Advances Expert Panel. Jacc Adv. 2022;1:100064.
Tanous D, Siu SC, Mason J, Greutmann M, Wald RM, Parker JD, Sermer M, Colman JM, Silversides CK. B-type natriuretic peptide in pregnant women with heart disease. J Am Coll Cardiol. 2010;56:1247–53.
Nguyen TX, Nguyen VT, Nguyen-Phan HN, Hoang BB. Serum levels of NT-proBNP in patients with preeclampsia. Integr Blood Press Control. 2022;15:43–51.
Sheikh M, Ostadrahimi P, Salarzaei M, Parooie F. Cardiac complications in pregnancy: a systematic review and meta-analysis of diagnostic accuracy of BNP and N-terminal pro-BNP. Cardiol Ther. 2021;10:501–14.
ACOG Practice Bulletin No. 106: Intrapartum fetal heart rate monitoring: nomenclature, interpretation, and general management principles. Obstet Gynecol. 2009;114(1):192–202.
Rossi A, Cornette J, Johnson MR, et al. Quantitative cardiovascular magnetic resonance in pregnant women: cross-sectional analysis of physiological parameters throughout pregnancy and the impact of the supine position. J Cardiov Magn Reson. 2011;13:31.
Intrapartum care for women with existing medical conditions or obstetric complications and their babies.
• Rouse CE, Easter SR, Duarte VE, Drakely S, Wu FM, Valente AM, Economy KE. Timing of delivery in women with cardiac disease. Am J Perinat. 2020;39:1196–203. Findings from this study showed that among pregnant patients with cardiac disease without complication, there is no maternal benefit to delivery before 39 weeks.
on Pregnancy PTF and American College of Obstetricians and Gynecologists. ACOG practice bulletin no. 212: pregnancy and heart disease. Obstet Gynecol. 2019;133(5):e320-e356.
Mok T, Woods A, Small A, et al. Delivery timing and associated outcomes in pregnancies with maternal congenital heart disease at term. J Am Heart Assoc. 2022;11: e025791.
Easter SR, Rouse CE, Duarte V, Hynes JS, Singh MN, Landzberg MJ, Valente AM, Economy KE. Planned vaginal delivery and cardiovascular morbidity in pregnant women with heart disease. Am J Obstet Gynecol. 2020;222:77.e1-77.e11.
Ruys TPE, Roos-Hesselink JW, Pijuan-Domènech A, et al. Is a planned caesarean section in women with cardiac disease beneficial? Heart. 2015;101:530.
(DGesGM) E by the ES of G (ESG) the Association for European Paediatric Cardiology (AEPC), and the German Society for Gender Medicine, Members AF, Regitz-Zagrosek V, et al. ESC Guidelines on the management of cardiovascular diseases during pregnancyThe Task Force on the Management of Cardiovascular Diseases during Pregnancy of the European Society of Cardiology (ESC). Eur Heart J. 2011;32:3147–3197.
• Mccoy JA, Kim YY, Nyman A, Levine LD. Prolonged labor and adverse cardiac outcomes in pregnant patients with congenital heart disease. Am J Obstet Gynecol. 2023. https://doi.org/10.1016/j.ajog.2022.11.1292. Findings from this study suggest that prolonged labor course in patient with congenital heart disease is associated with an increased risk of adverse peripartum cardiovascular outcomes. This risk is further increased among patient with a prolonged labor course who then undergo a cesarean section.
Roos-Hesselink J, Baris L, Johnson M, et al. Pregnancy outcomes in women with cardiovascular disease: evolving trends over 10 years in the ESC Registry Of Pregnancy And Cardiac disease (ROPAC). Eur Heart J. 2019;40:ehz136.
O’Kelly AC, Scott N, Yeh DD. Delivering coordinated cardio-obstetric care from preconception through postpartum. Cardiol Clin. 2021;39:163–73.
Roos-Hesselink JW, Budts W, Walker F, Backer JFAD, Swan L, Stones W, Kranke P, Sliwa-Hahnle K, Johnson MR. Organisation of care for pregnancy in patients with congenital heart disease. Heart. 2017;103:1854.
Curtis SL, Swan L. Aortopathy in pregnancy. Heart. 2022;108:1851–7.
Albright CM, Steiner J, Sienas L, Delgado C, Buber J. Main operating room deliveries for patients with high-risk cardiovascular disease. Open Hear. 2023;10: e002213.
Bredy C, Mongeon F-P, Leduc L, Dore A, Khairy P. Pregnancy in adults with repaired/unrepaired atrial septal defect. J Thorac Dis. 2017;10:S2945–52.
ACOG practice bulletin no. 211: critical care in pregnancy. Obstet Gynecol. 2019;133:e303–e319.
Valente AM, Landzberg MJ, Gauvreau K, et al. Standardized outcomes in reproductive cardiovascular care: The STORCC initiative. Am Heart J. 2019;217:112–20.
Prokšelj K, Brida M. Cardiovascular imaging in pregnancy. Int J Cardiol Congenit Hear Dis. 2021;5: 100235.
Millman AL, Payne B, Qu Z, Douglas MJ, Hutcheon JA, Lee T, Magee LA, Walley KR, Dadelszen P von, Group for the P (Pre-eclampsia IE of RS. Oxygen saturation as a predictor of adverse maternal outcomes in women with preeclampsia. J Obstet Gynaecol Can. 2011;33:705–14.
Author information
Authors and Affiliations
Contributions
The first two authors listed contributed equally to the manuscript
Corresponding authors
Ethics declarations
Ethical Standards
All reported studies/experiments involving human or animal subjects performed by the authors were in accordance with the ethical standards of institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Conflict of Interest
The authors declare that they have no conflict of interest.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Williams, A., Misra, A. & Economy, K. Intrapartum Management of Maternal Congenital Heart Disease. Curr Obstet Gynecol Rep 12, 215–224 (2023). https://doi.org/10.1007/s13669-023-00369-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13669-023-00369-4