Abstract
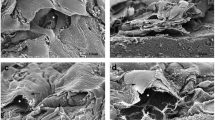
Development of a natural alternative to cardiac assist devices (CADs) will pave the way to a heart failure therapy which overcomes the disadvantages of current mechanical devices. This work provides the framework for fabrication of a tissue engineered heart pump (TEHP). Artificial heart muscle (AHM) was first fabricated by culturing 4 million rat neonatal cardiac cells on the surface of a fibrin gel. To form a TEHP, AHM was wrapped around an acellular goat carotid artery (GCA) and a chitosan hollow cylinder (CHC) scaffold with either the cardiac cells directly contacting the construct periphery or separated by the fibrin gel. Histology revealed the presence of cardiac cell layer cohesion and adhesion to the fibrin gel scaffold, acellular GCA, and synthesized CHC. Expression of myocytes markers, connexin43 and α-actinin, was also noted. Biopotential measurements revealed the presence of ~2.5 Hz rhythmic propagation of action potential throughout the TEHP. Degradation of the fibrin gel scaffold of the AHM via endogenous proteases may be used as a means of delivering the cardiac cells to cylindrical scaffolds. Further development of the TEHP model by use of multi-stimulus bioreactors may lead to the application of bioengineered CADs.







Similar content being viewed by others
References
Ahmed, T. A. E., E. V. Dare, and M. Hincke. Fibrin: a versatile scaffold for tissue engineering applications. Tissue Eng. Part B. Rev. 14:199–215, 2008.
Anversa, P., J. Kajstura, M. Rota, and A. Leri. Regenerating new heart with stem cells. J. Clin. Invest. 123:62–70, 2013.
Barsotti, M. C., F. Felice, A. Balbarini, and R. Di Stefano. Fibrin as a scaffold for cardiac tissue engineering. Biotechnol. Appl. Biochem. 58:301–310, 2011.
Birla, R. K., D. E. Dow, Y.-C. Huang, F. Migneco, L. Khait, G. H. Borschel, et al. Methodology for the formation of functional, cell-based cardiac pressure generation constructs in vitro. In Vitro Cell. Dev. Biol. Anim. 44:340–350, 2008.
Camelliti, P., T. K. Borg, and P. Kohl. Structural and functional characterisation of cardiac fibroblasts. Cardiovasc. Res. 65:40–51, 2005.
Cereghetti, C., C. Kaiser, and S. Cook. Ventricular assist devices in acute heart failure. Minerva Cardioangiol. 60:395–403, 2012.
Cohn, L. H. The role of mechanical devices. J. Card. Surg. 5:278–281, 1990.
Engin, C., F. Ayik, E. Oguz, B. Eygi, T. Yagdi, S. Karakula, et al. Ventricular assist device as a bridge to heart transplantation in adults. Transplant. Proc. 43:927–930, 2011.
Frazier, O. H. New technologies in the treatment of severe cardiac failure: the Texas Heart Institute experience. Ann. Thorac. Surg. 59:S31–S37, 1995; ((Discussion S38)).
Fujimoto, K. L., K. C. Clause, L. J. Liu, J. P. Tinney, S. Verma, W. R. Wagner, et al. Engineered fetal cardiac graft preserves its cardiomyocyte proliferation within postinfarcted myocardium and sustains cardiac function. Tissue Eng. Part A 17:585–596, 2011.
Gandaglia, A., R. Huerta-Cantillo, M. Comisso, R. Danesin, F. Ghezzo, F. Naso, et al. Cardiomyocytes in vitro adhesion is actively influenced by biomimetic synthetic peptides for cardiac tissue engineering. Tissue Eng. Part A 18:725–736, 2012.
Gilbert, T. W., T. L. Sellaro, and S. F. Badylak. Decellularization of tissues and organs. Biomaterials 27:3675–3683, 2006.
Hecker, L., L. Khait, D. Radnoti, and R. Birla. Novel bench-top perfusion system improves functional performance of bioengineered heart muscle. J. Biosci. Bioeng. 107:183–190, 2009.
Huang, Y.-C., L. Khait, and R. K. Birla. Contractile three-dimensional bioengineered heart muscle for myocardial regeneration. J. Biomed. Mater. Res. A. 80:719–731, 2007.
Khait, L., and R. K. Birla. Cell-based cardiac pumps and tissue-engineered ventricles. Regen. Med. 2:391–406, 2007.
Kubo, H., T. Shimizu, M. Yamato, T. Fujimoto, and T. Okano. Creation of myocardial tubes using cardiomyocyte sheets and an in vitro cell sheet-wrapping device. Biomaterials 28:3508–3516, 2007.
Kupcsik, L., M. Alini, and M. J. Stoddart. Epsilon-aminocaproic acid is a useful fibrin degradation inhibitor for cartilage tissue engineering. Tissue Eng. Part A 15:2309–2313, 2009.
Melchiorri, A. J., N. Hibino, and J. P. Fisher. Strategies and techniques to enhance the in situ endothelialization of small-diameter biodegradable polymeric vascular grafts. Tissue Eng. Part B. Rev. 19:292–307, 2013.
Tao, Z.-W., M. Mohamed, M. Hogan, L. Gutierrez, and R. K. Birla. Optimizing a spontaneously contracting heart tissue patch with rat neonatal cardiac cells on fibrin gel. J. Tissue Eng. Regen. Med. 2014. doi:10.1002/term.1895.
Villalona, G. A., B. Udelsman, D. R. Duncan, E. McGillicuddy, R. F. Sawh-Martinez, N. Hibino, et al. Cell-seeding techniques in vascular tissue engineering. Tissue Eng. Part B. Rev. 16:341–350, 2010.
Acknowledgments
The researchers would like to acknowledge NIH for provision of funding for this research. We would also like to thank the Department of Biomedical Engineering and the Cullen College of Engineering at University of Houston for further financial support.
Conflict of interest
Research was funded by NIH (Grant number: R01-EB011516).
Statement of Human Studies
No human studies were carried out by the authors for this article.
Statement of Animal Studies
Approval for animal use was granted by the Institutional Animal Care and Use Committee (IACUC) at the University of Houston, in accordance with the “Guide for the Care and Use of Laboratory Animals” (NIH publication 86-23, 1996).
Author information
Authors and Affiliations
Corresponding author
Additional information
Associate Editor Ajit P. Yoganathan oversaw the review of this article.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplementary material 1 (AVI 1090 kb)
Supplementary material 2 (AVI 781 kb)
Rights and permissions
About this article
Cite this article
Mohamed, M.A., Hogan, M.K., Patel, N.M. et al. Establishing the Framework for Tissue Engineered Heart Pumps. Cardiovasc Eng Tech 6, 220–229 (2015). https://doi.org/10.1007/s13239-015-0211-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13239-015-0211-4