Abstract
Purpose
This case report describes two successful pregnancies after intracytoplasmic sperm injection (ICSI) with testicular spermatozoa that were transported under refrigeration.
Methods
Two first-time couples consulted our clinic concerned about their primary infertility. No sperm were present in the semen samples from either of the husbands and they were referred to the urology department (UD) of a neighbouring hospital. At the UD, seminiferous tubules were obtained by testicular sperm extraction. The tissue samples were put in a centrifuge tube with phosphate-buffered saline at 6°C and placed with refrigerant in a cushioned styrofoam box that was then transported to our clinic. Immediately upon arrival at our clinic, testicular spermatozoa were extracted. On the same day, ovum pickup was performed and mature oocytes were extracted that were then inseminated by conventional ICSI. Fertilized eggs were cultured for 2 days, and then cleaved embryos were cryopreserved. In one case after 4 months and in the other case after 2 months of cryopreservation, the frozen-thawed embryos were transferred.
Result
Both patients became pregnant and normal, healthy babies were born.
Conclusions
These results suggest that cases of obstructive azoospermia can be treated with ICSI by refrigerated transport of the seminiferous tubules, in cooperation with a UD, in a small single departmental obstetrics and gynecology clinic.
Similar content being viewed by others
References
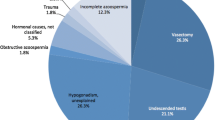
Irvine DS. Epidemiology and aetiology of male infertility. Hum Reprod. 1998;13:33–44.
Schoysman R, Vanderzwalmen P, Nijs M, Segal-Bertin G, van de Casseye M. Successful fertilization by testicular spermatozoa in an in-vitro fertilization programme (Letter). Hum Reprod. 1993;8:1339–40.
Schoysman R, Vanderzwalmen P, Nijs M, Segal L, Segal-Bertin G, Geerts L, et al. Pregnancy after fertilization with human testicular spermatozoa. Lancet. 1993;342:1237.
Tournaye H, Devroey P, Liu J, Nagy Z, Lissens W, Van Steirteghem A. Microsurgical epididymal sperm aspiration and intracytoplasmic sperm injection: a new effective approach to infertility as a result of congenital bilateral absence of the vas deferens. Fertil Steril. 1994;61:1045–50.
Bunge RG, Sherman JK. Fertilizing capacity of frozen human spermatozoa. Nature. 1953;172:767–8.
Cohen J, Garrisi GJ, Congedo-Ferrara TA, Kieck KA, Schimmel TW, Scott RT. Cryopreservation of single human spermatozoa. Hum Reprod. 1997;12:994–1001.
Schuster TG, Keller LM, Dunn RL, Ohl DA, Smith GD. Ultra-rapid freezing of very low numbers of sperm using cryoloops. Hum Reprod. 2003;18:788–95.
Friedler S, Raziel A, Soffer Y, Strassburger D, Komarovsky D, Ron-EI R. The outcome of intracytoplasmic injection of fresh and cryopreserved epididymal spermatozoa from patients with obstructive azoospermia—a comparative study. Hum Reprod. 1998;13:1872–7.
De Croo I, Van der Elst J, Everaert K, De Sutter P, Dhont M. Fertilization, pregnancy and embryo implantation rates after ICSI with fresh or frozen-thawed testicular spermatozoa. Hum Reprod. 1998;13:1893–7.
Konc J, Kanyó K, Cseh S. The effect of condition/state of testicular spermatozoa injected to the outcome of TESE–ICSI–ET cycle. Eur J Obstet Gynecol Reprod Biol. 2008;141:39–43.
Jaskey DG, Cohen MR. Twenty-four to ninety-six-hour storage of human spermatozoa in test-yolk buffer. Fertil Steril. 1981;35:205–8.
Johnson AR, Syms AJ, Lipshultz LI, Smith RG. Conditions influencing human sperm capacitation and penetration of zona-free hamster ova. Fertil Steril. 1984;41:603–8.
Kimura Y, Yanagimachi R. Intracytoplasmic sperm injection in the mouse. Biol Reprod. 1995;52:709–20.
Yokota Y, Sakamoto H. Essential manual of assisted reproductive technology for embryologists. In: Suzuki S, Hukuda A, Araki Y, Sato K, editors. Luteal support. Tokyo: Ishiyaku Publishers; 2005. p. 353–6. (in Japanese).
Kuwayama M. Highly efficient vitrification for cryopreservation of human oocytes and embryos: the cryotop method. Theriogenology. 2007;67:73–80.
De Oliveira NM, Vaca Sánchez R, Rodriguez Fiesta S, Lopez Salgado T, Rodríguez R, Bethencourt JC, et al. Pregnancy with frozen-thawed and fresh testicular biopsy after motile and immotile sperm microinjection, using the mechanical touch technique to assess viability. Hum Reprod. 2004;19:262–5.
O’Connell M, McClure N, Lewis SE. The effects of cryopreservation on sperm morphology, motility and mitochondrial function. Hum Reprod. 2002;17:704–9.
Donnelly ET, Steele EK, McClure N, Lewis SE. Assessment of DNA integrity and morphology of ejaculated spermatozoa from fertile and infertile men before and after cryopreservation. Hum Reprod. 2001;16:1191–9.
Dondero F, Rossi T, Delfino M, Imbrogno N, Cannistrà S, Mazzilli F. Human semen refrigeration at +4°C: bio-kinetic characteristics. Cell Tissue Bank. 2006;7:61–4.
Van Thuan N, Wakayama S, Kishigami S, Wakayama T. New preservation method for mouse spermatozoa without freezing. Biol Reprod. 2005;72:444–50.
Mochida K, Ohkawa M, Inoue K, Valdez DM Jr, Kasai M, Ogura A. Birth of mice after in vitro fertilization using C57BL/6 sperm transported within epididymides at refrigerated temperatures. Theriogenology. 2005;64:135–43.
Fan ZQ, Li XW, Liu Y, Meng QG, Wang YP, Hou YP, et al. Piezo-assisted in vitro fertilization of mouse oocytes with spermatozoa retrieved from epididymides stored at 4°C. J Reprod Dev. 2008;54:107–12.
An TZ, Wada S, Edashige K, Sakurai T, Kasai M. Viable spermatozoa can be recovered from refrigerated mice up to 7 days after death. Cryobiology. 1999;38:27–34.
Soler AJ, Esteso MC, Fernández-Santos MR, Garde JJ. Characteristics of Iberian red deer (Cervus elaphus hispanicus) spermatozoa cryopreserved after storage at 5°C in the epididymis for several days. Theriogenology. 2005;64:1503–17.
Kaneko T, Fukumoto K, Haruguchi Y, Kondo T, Machida H, Koga M, et al. Fertilization of C57BL/6 mouse sperm collected from cauda epididymides after preservation or transportation at 4°C using laser-microdissected oocytes. Cryobiology. 2009;59:59–62.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Inoue, T., Sugimoto, H., Okubo, K. et al. Successful pregnancy after intracytoplasmic sperm injection with testicular spermatozoa transported only under refrigeration. Reprod Med Biol 9, 173–177 (2010). https://doi.org/10.1007/s12522-010-0053-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12522-010-0053-6