Abstract
Background
Recent studies have compared CTA to stress testing and MPI using older Na-I SPECT cameras and traditional rest-stress protocols, but are limited by often using optimized CTA protocols but suboptimal MPI methodology. We compared CTA to stress testing with modern SPECT MPI using high-efficiency CZT cameras and stress-first protocols in an ED population.
Methods
In a retrospective, non-randomized study, all patients who underwent CTA or stress testing (ETT or Tc-99m sestamibi SPECT MPI) as part of their ED assessment in 2010-2011 driven by ED attending preference and equipment availability were evaluated for their disposition from the ED (admission vs discharge, length of time to disposition), subsequent visits to the ED and diagnostic testing (within 3 months), and radiation exposure. CTA was performed using a 64-slice scanner (GE Lightspeed VCT) and MPI was performed using a CZT SPECT camera (GE Discovery 530c). Data were obtained from prospectively acquired electronic medical records and effective doses were calculated from published conversion factors. A propensity-matched analysis was also used to compare outcomes in the two groups.
Results
A total of 1,458 patients underwent testing in the ED with 192 CTAs and 1,266 stress tests (327 ETTs and 939 MPIs). The CTA patients were a lower-risk cohort based on age, risk factors, and known heart disease. A statistically similar proportion of patients was discharged directly from the ED in the stress testing group (82% vs 73%, P = .27), but their time to disposition was longer (11.0 ± 5 vs 20.5 ± 7 hours, P < .0001). There was no significant difference in cardiac return visits to the ED (5.7% CTA vs 4.3% stress testing, P = .50), but more patients had follow-up studies in the CTA cohort compared to stress testing (14% vs 7%, P = .001). The mean effective dose of 12.6 ± 8.6 mSv for the CTA group was higher (P < .0001) than 5.0 ± 4.1 mSv for the stress testing group (ETT and MPI). A propensity score-matched cohort showed similar results to the entire cohort.
Conclusions
Stress testing with ETT, high-efficiency SPECT MPI, and stress-only protocols had a significantly lower patient radiation dose and less follow-up diagnostic testing than CTA with similar cardiac return visits. CTA had a shorter time to disposition, but there was a trend toward more revascularization than with stress testing.
Similar content being viewed by others
Introduction
Chest pain is the second most common symptom leading to emergency department (ED) visits with over 8 million visits annually that may represent an acute coronary syndrome (ACS), and there is a tremendous cost associated with the evaluation of these patients.1 As overcrowded emergency departments continue to see millions of patients each year with chest pain, chest pain units (CPU) have been established to efficiently and accurately identify patients with cardiac ischemia and rapidly exclude those without it.2 Noninvasive cardiac diagnostic testing has become a cornerstone of the evaluation and triage of these ED CPU patients.
Multidetector row computed tomography angiography (CTA), while a newer technology, has proven to be a clinically robust and efficient modality for the noninvasive diagnosis of coronary artery disease.3,4 Rapid improvement in CT scanner technology has occurred in the past few years which has resulted in improvement in image quality, reduction in imaging artifacts, increased percentage of diagnostic scans, and decreased radiation exposure.5 The diagnostic accuracy and overall prognostic power of SPECT myocardial perfusion imaging (MPI) are its major strengths.6 There have been a number of recent improvements to traditional stress SPECT protocols including stress-only imaging that can decrease the length of the test and lower the radiation dose with a documented benign prognosis similar to that of a normal rest-stress study.7-10 Additionally, new high-efficiency SPECT camera technology has also modernized MPI by allowing for shorter image acquisition and lower injected activity.11-13
Several recent randomized studies and two meta-analyses have been published examining the diagnostic utility of CTA in evaluating patients in the ED with possible ACS.14-19 Recent CTA studies have suggested efficient triage of patients, safe expedited discharge from the ED, cost effectiveness, and lower radiation dose when compared to standard diagnostic evaluation including MPI. However, this comparison has been to older conventional Na-I SPECT cameras using traditional rest-stress protocols.
We sought to compare CTA to modern SPECT MPI using high-efficiency CZT (cadmium-zinc-telluride) cameras and newer stress-first protocols in a real-world ED CPU population. The very fact of being in a trial may result in preferentially faster test performance, more attention to radiation doses, and more efficient discharges, so that previous studies might not represent the real-world experience. Both diagnostic modalities are available in our institution’s ED for use at the ED attending’s discretion in the evaluation of patients presenting to the ED with acute chest pain. We evaluated all consecutive patients in the ED CPU over a recent 2-year period of time using modern approaches to CTA and SPECT MPI.
Materials and Methods
Study Design
In a retrospective, non-randomized study, all patients who underwent CTA, ETT, or stress Tc-99m sestamibi SPECT MPI as part of their ED CPU assessment in 2010-2011 driven by ED attending preference and equipment availability were evaluated for their radiation dose and subsequent diagnostic testing. This study protocol was approved by our institutional IRB. ED patients were triaged through the ED Chest Pain Unit, an observational unit for patients presenting with possible ACS or unstable angina, based on their presenting complaints suggestive of cardiac ischemia. CTA was performed using a 64-slice scanner (GE Lightspeed VCT) and MPI was performed using either a CZT SPECT camera (GE Discovery 530c) or a conventional SPECT camera (Vertex Plus, Philips/ADAC Laboratories). The triage to stress testing or CTA was at the discretion of the attending ED physician and included such factors as patient characteristics, time of day, and equipment availability. Stress echocardiography at our institution is not routinely available for ED patients.
Study Setting
The Mount Sinai Medical Center Emergency Department is an urban ED which handles over 80,000 patient visits annually. Patients were referred for a SPECT MPI or ETT from the CPU after serial negative cardiac biomarkers (at least two sets 4-6 hours apart) and the absence of new ECG changes. Low-risk patients who were able to exercise adequately were triaged to ETT alone as opposed to MPI. Stress testing was available during daytime hours Monday through Saturday. Patients were referred to CTA after one set of negative cardiac biomarkers. CTA was available during daytime hours Monday through Friday. Patients with diagnostic ECG changes such as ST-segment elevation or ST-segment depression were excluded along with those with elevated cardiac biomarkers. Patients who had an abnormal result of noninvasive testing in the CPU routinely had a consultation by a cardiologist to decide on further clinical management.
Endpoints and Data Collection
The results of the initial diagnostic testing, CTA or SPECT MPI, were recorded. Both studies were considered as either normal, abnormal, or non-diagnostic. For CTA, abnormal studies were categorized as obstructive or non-obstructive based on the conclusion on the study report.
Follow-up cardiac testing at our institution including exercise stress testing, stress MPI, stress echocardiography, cardiac CTA, and invasive coronary angiography was recorded at 3 months after their index ED study. These results were obtained from the Cardiology Report database. The results of subsequent coronary angiography were categorized as normal, non-obstructive (epicardial coronary stenosis of <70%), or obstructive (epicardial coronary stenosis ≥70%). Coronary revascularization (PCI or CABG) by the end of follow-up was noted. Sensitivity, specificity, positive predictive value, and negative predictive value for the detection of obstructive coronary artery disease (CAD) were calculated for CTA and MPI using the results of subsequent invasive coronary angiography as the gold standard. The occurrence of return visits to the ED within 90 days of the index visit was noted from ED medical records. Return visits to the ED were classified as either cardiac or non-cardiac based on review of the medical records. A cardiac visit was defined as one for a possible CAD etiology including chest pain, unstable angina, acute coronary syndrome, or exclusion of any of these conditions.
During the final seven months of the study period (June 2011 through December 2011), electronic medical records were available in the ED (EPIC, Verona, Wisconsin). This allowed for the prospective recording in a subset of patients of the time of arrival to the ED, time of disposition from the ED, and disposition from the ED (admission to the hospital, discharge home, or assignment of observation status). Time of disposition from the ED was defined as the time at which the patient was admitted to the hospital, discharged home, or left the ED against medical advice. The time to disposition was defined as the amount of time between the time of arrival in the ED and the time of disposition.
Demographic and stress test variables were prospectively collected for all ETT and SPECT MPI patients at the time of stress testing in the Nuclear Cardiology Database. The demographic variable recorded included age, gender, height, weight, BMI, and patient location. Clinical variables included presenting symptoms of chest pain or shortness of breath; cardiac risk factors of diabetes, hypertension, hyperlipidemia, smoking (past or present), and family history of premature CAD; and known CAD by diagnostic testing or patient history, history of percutaneous coronary intervention (PCI), and history of coronary artery bypass grafting (CABG) surgery. Identical information was obtained on CTA patients retrospectively from ED medical record review and CTA reports.
Pre-test risk of cardiovascular outcomes was calculated using the ACC/AHA pre-test probability score.20 The ACC/AHA risk score incorporates age, gender, and presenting symptoms.
Effective dose from CTA was estimated from scanner-reported dose-length product using two recently derived cardiac, scanner-specific conversion factors.21,22 The lower Huda et al22 conversion factor of 0.026 was chosen to be used for all CTA calculations. The effective dose for MPI was determined from administered activity using separate conversion factors for stress and rest imaging provided in the International Commission on Radiological Protection (ICRP) Publication 80.23
Statistics
Characteristics of the study population were compared based on the diagnostic testing they received. A two-tailed student t test was used to compare continuous variables and a chi-squared test or Fisher’s exact test (used with small sample sizes) was used to compare categorical variables (InStat 3, Graph Pad). Sensitivity, specificity, positive predictive value, and negative predictive value were calculated in the usual fashion. Effective dose analyses were performed using STATA/SE 11.2 (StataCorp, College Station, TX).
Due to the differences in baseline characteristics between the CTA and stress testing groups, we compared outcomes using a propensity-matched analysis. A propensity score was generated in each study subject using a logistic regression model with CTA allocation as the dependent outcome. Candidate covariates included age, gender, BMI, history of CAD, diabetes, chest pain, shortness of breath, smoking, and ACC/AHA risk score using STATA 12.1, (StataCorp, College Station, TX). The matched cohort was generated using a 1:1 matching algorithm with each CTA subject matched to one stress test subject.
CTA Protocols
A standard imaging protocol as endorsed by SCCT was used for all patients.24 CTA was performed using a 64-slice scanner (LightSpeed VCT, XT; GE Healthcare, Milwaukee, Wisconsin) with either retrospective or prospective electrocardiographic gating. Retrospective gating was commonly used when the heart rate was faster (typically >65-70 beats·minute−1) and/or an irregular rhythm was present. All patients received sublingual nitroglycerin (0.4 mg) and beta blockers (intravenous metoprolol 5-30 mg) if their heart rates were >60 beats·minute−1, unless contraindications were present. After standard scouts in the supine position, a noncontrast scan was performed to assess coronary artery calcification. This consisted of a single inspiratory breath-hold craniocaudal acquisition covering from the carina to the inferior heart border. Prospectively triggered imaging was used, with a tube voltage and current of 120 kVp and typical 200 mA, respectively. Subsequently, contrast-enhanced angiography was performed after timing the arrival of contrast agent (Isovue 370; Schering AG, Berlin, Germany) with a threshold of 100 Hounsfield units in a region of interest in the ascending aorta (bolus-tracking technique). A 70- to 100-mL contrast bolus followed by 50 mL of saline was injected through a peripheral vein at 4-5 mL·s−1. For scanning, a detector collimation of 64 × 0.625 mm was used, with a gantry rotation time of 350 ms, pitch of 0.16, tube voltage of 100-120 kVp, and typical tube current of 400-700 mA. Tube current modulation was used if applicable in the retrospective protocols. When possible, mA and/or kV were adjusted based on patient weight or body habitus. A typical padding setting of 200 ms was employed in prospectively gated studies.
Axial images were reconstructed with an image matrix of 512 × 512 pixels and slice thickness of 0.625 mm. For retrospectively gated acquisitions, a half-scan algorithm with a temporal resolution of ~175 ms was performed, whereas a multisegment algorithm was used for heart rates >70 beats·minute−1. Images were preferentially reconstructed in the mid-diastolic phase (65%-85% of the cardiac cycle) for motion-free images of the coronary arteries. The results of CCTA were interpreted on a dedicated workstation (Aquarius; TeraRecon, Foster City, CA) by 2 experienced readers. Visual coronary assessment was performed on original axial sources images, thin-slice maximum-intensity projections, or multiplanar reformatted reconstructions. Significant or obstructive CAD was defined as ≥50% luminal diameter narrowing and considered moderate or severe when causing 50%-70% or >70% stenosis, respectively.25,26 Plaques causing <50% stenosis were considered non-significant disease. Non-diagnostic results of CCTA were considered when any coronary segment was not evaluable because of motion artifacts, calcification, or low contrast-to-noise ratio.
SPECT Imaging and Stress Protocols
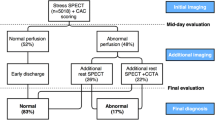
A standard imaging protocol as endorsed by ASNC was used for all patients.27,28 A rest-stress or stress-first imaging sequence was employed using Tc-99m sestamibi. If stress-first images demonstrated normal perfusion and normal left ventricular function (LVEF ≥ 50%), rest imaging was not performed. If stress imaging was abnormal, then a clinical decision was made to manage the patient medically, perform subsequent rest imaging, or refer the patient for cardiac catheterization. Low-risk patients with an interpretable rest ECG who were felt to have good exercise capacity underwent ETT alone without MPI, and those patients who did not attain ≥80% of their maximal predicted heart rate were converted to pharmacologic stress with MPI. While the high-efficiency CZT camera was the preferred camera, the decision to use the CZT SPECT camera or the conventional SPECT camera was determined by the patient’s body habitus, with patients >250 pounds preferentially being imaged on the conventional SPECT camera, and by the patient’s mobility, with patients who could not easily undergo prone imaging preferentially being imaged on the conventional SPECT camera.
Standard exercise and pharmacologic protocols as endorsed by ASNC were employed.29 Exercise testing was performed according to the Bruce or modified Bruce protocol, with heart rate, blood pressure, and 12-lead electrocardiogram recorded before, during, and after exercise. Exercise was terminated for limiting cardiac symptoms or for >2 mm horizontal or downsloping ST-segment depression measured 80 ms after the J-point over at least 3 consecutive beats. All pharmacologic stressors except regadenoson were given using weight-based protocols with an upper dose limit of 300 lbs (136 kg), with patients exceeding the upper limit receiving a dose based on a weight of 300 lbs (136 kg). Adenosine was administered as a 6-minute infusion at 140 mcg·kg−1·minute−1 which could be reduced to 110 mcg·kg−1·minute−1 if severe symptoms or hemodynamic effects were encountered. Dipyridamole was infused over 4 minutes at a dose of 0.56 mg·kg−1. Regadenoson was administered as a 0.4-mg/5-mL bolus followed by a 5-mL saline flush. The dobutamine protocol consisted of an initial infusion of 5 mcg·kg−1·minute−1, increasing incrementally every 3 minutes to 40 mcg·kg−1·minute−1 to achieve a target heart rate of >85% of predicted maximal.
Gated SPECT imaging was performed using one of two SPECT cameras: a CZT camera (Discovery NM 530c, GE Healthcare, Haifa, Israel), with a multi-pinhole collimator with 19 stationary CZT detectors simultaneously imaging 19 cardiac views without detector or collimator motion, and penalized maximum likelihood iterative reconstruction, or a conventional dual-head camera (Vertex Plus, Philips/ADAC Laboratories), stop and shoot acquisition with 64 stops, a 180° arc from right anterior oblique to left anterior oblique, a 64 × 64 × 16 matrix, iterative reconstruction, and a VXGP collimator. Image acquisition began 30-60 minutes after tracer injection for Tc-99m. Post-stress images were gated at rest. Left ventricular ejection fraction (EF) was determined using commercial software (QGS, Cedars-Sinai, Los Angeles, CA).
Isotope dose was weight based and dependent on the protocol performed. For a standard one-day Tc-99m rest-stress protocol, the rest dose was 8-12 mCi based on four weight groups (<150, 151-200, 201-250, and >250 lbs) and the stress dose was 24-36 mCi based on the same weight ranges. The stress-only protocol employed a low dose Tc-99m stress dose of 12.5-15 mCi if the weight was <150 lbs and a high dose Tc-99m stress dose of 25-38 mCi which was weight adjusted based on three weight groups (151-200, 201-250, and >250 lbs).
Attenuation reduction or correction, using either prone in addition to supine stress imaging with the CZT SPECT camera or a Gd-153 line source (Vantage Pro, Philips/ADAC) with the conventional SPECT camera, was performed routinely in all studies.
Results
Demographics
Over the 2-year period, 192 patients underwent CTA and 1,266 patients underwent stress testing including 939 Tc-99m sestamibi SPECT MPI and 327 ETT (Figure 1). Of the MPI studies, 86 (9.2%) were performed using a conventional SPECT camera instead of the high-efficiency CZT SPECT camera due to either patient’s obesity or poor mobility.
The CTA patients were a lower-risk cohort based on age, gender, cardiac risk factors, and known atherosclerotic heart disease (Table 1). In the MPI group, 708 (75.4%) underwent stress-only imaging, 184 (19.6%) rest-stress, and 47 (5.0%) stress-rest. There were 530 (56.4%) exercise stress studies and 409 (43.6%) pharmacologic stress tests with 99% being vasodilator stress. The ETT group was lower risk than both of the SPECT MPI groups based on age, fewer cardiac risk factors, known CAD, and ACC/AHA risk score (Table 2). Compared to the conventional SPECT cohort, the CZT SPECT group had a lower BMI, fewer cardiac risk factors, but more known CAD, and was skewed toward higher ACC/AHA risk scores.
The results of the initial diagnostic test in the ED CPU are found in Table 3. As CTA is an anatomic study and MPI a physiologic test, direct comparison of the results cannot be made. However, if normal stress tests consist of patients with both no CAD and non-obstructive disease, the proportion of 87.2% “normal” stress tests is similar to 86.5% normal and non-obstructive disease found in the CTA group. Patients in the MPI group with abnormal perfusion had an average stress total perfusion deficit of 15.0% ± 9.8% which became 11.2% ± 10.2% after applying attenuation correction. There was a non-significant trend toward more non-diagnostic CTA studies than stress tests (1.6% vs 0.3%, P = .08). In the 327 patients who underwent ETT, patients exercised on average for 10.1 ± 2.7 METs, to 89.5% ± 10.3% of their maximal predicted heart rate, and 4 (1.2%) had an abnormal ECG response. In the 939 MPI patients, 157 (16.7%) had abnormal perfusion results.
Follow-Up Testing, ED Return Visits, and Time to Disposition
Follow-up cardiac diagnostic testing by 3 months after the index ED visit showed more follow-up testing overall in the CTA group compared to the stress testing group (P = .001) (Table 3). While there was no significant difference in the proportion of subsequent angiograms between the CTA and stress testing groups, there were more follow-up stress tests in the CTA group (P < .0001). Of the 26 abnormal (obstructive) or non-diagnostic CTA studies, 50.0% had follow-up diagnostic testing within 3 months, compared to the 161 abnormal or non-diagnostic stress tests, where 37.9% had follow-up diagnostic testing within 3 months (P = .34).
A total of 22 and 115 coronary angiograms were performed in the CTA and stress testing groups, respectively, by the end of study follow-up (18.0 ± 6.6 months in the CTA group and 18.1 ± 7.5 months in the stress testing group) (Table 4). These anatomic studies included invasive angiograms for the CTA group and invasive angiograms (n = 102) and CT angiograms (n = 13) for the MPI group. There was no statistical difference in the number of normal invasive angiograms between the groups (22.7% vs 20.9%, P = .85). There was a trend toward more obstructive and less non-obstructive coronary disease in the CTA cohort compared to the stress testing group, but this did not reach statistical significance (P = .26 and .18). This resulted in a better sensitivity (80.0% vs 56.5%) and negative predictive value (75.0% vs 41.2%) for CTA and a better specificity (61.8% vs 54.6%) and positive predictive value (75.0% vs 61.5%) for MPI in this selected, relatively small cohort of patients who had subsequent angiography. There was a greater proportion of coronary revascularizations performed in the CTA group compared to the MPI group which did not attain statistical significance (6.8% vs 3.6%, P = .06). All but one of the revascularizations was percutaneous.
In looking at return visits to the ED within 3 months of the index ED visit, 55 patients (4.3%) in the stress testing group returned for cardiac visits, while 11 patients (5.7%) in the CTA cohort returned (P = .50). There were 206 non-cardiac visits (16.3%) in the stress testing patients and 21 (10.9%) in the CTA group (P = .07).
There were 40 CTA patients and 309 stress testing patients in the subgroup of patients who presented during the 7-month period when an electronic medical record was available in the ED (Figure 2; Table 5). There was no statistically significant difference in the proportion of ED discharges in the stress testing group compared to the CTA group (81.2% vs 72.5%, P = .28). The CTA group spent a significantly shorter period of time in the ED until a disposition was made (11.0 ± 5.2 vs 20.5 ± 7.0 hours, P < .0001).
Radiation Exposure
The CZT SPECT group had a mean stress-only activity of 17.0 ± 6.6 mCi and a total rest-stress activity of 32.2 ± 7.6 mCi. The conventional SPECT group had a substantially higher weight at 258.9 ± 56.7 lbs and BMI at 41.9 ± 7.8 kg·m−2 than both the CTA and CZT SPECT groups which resulted in an average total rest-stress activity of 44.5 ± 3.7 mCi and stress-only activity of 31.2 ± 5.9 mCi.
The radiation exposure to patients can be seen in Table 6. Using two scanner-specific cardiac conversion factors found in the literature for calculating effective dose from the dose-length product, the mean effective dose for the CTA was 12.6 ± 8.6 and 13.5 ± 9.2 mSv.21,22 The lower Huda et al22 conversion factor of 0.026 was subsequently used for all CTA calculations. The lowest effective dose was 1.8 mSv and the highest was 43.0 mSv with a median of 9.4 mSv (IQR 7.1-15.0 mSv). In comparison, the mean effective dose for the entire stress test group was 5.0 ± 4.1 mSv (P < .0001), 6.7 ± 3.4 mSv for the entire SEPCT MPI cohort (P < .0001), and 6.4 ± 3.3 mSv for the CZT SPECT group (P < .0001). The lowest effective dose in the overall stress testing group was 3.5 mSv and the highest was 16.4 mSv with a median of 3.9 mSv (IQR 0-7.9 mSv). Comparing CTA patients with BMI < 30 kg·m−2 to those with a BMI ≥ 30 kg·m−2, there was no significant difference in effective dose (12.5 ± 8.8 vs 14.4 ± 10.1, P = .25). Female patients received non-significantly more radiation than male patients (13.0 ± 9.5 vs 12.2 ± 7.5 mSv, P = .09). A total of 143 (74.5%) were prospectively gated, while 49 (25.5%) were retrospectively gated. Those patients undergoing prospective gating had a lower effective dose than those with retrospective gating (9.9 ± 6.6 vs 22.5 ± 7.9 mSv, P < .0001). Filtered back projection was used for CTA processing in 2010 and upgraded to iterative reconstruction in 2011, resulting in a decrease in mean effective dose from 14.8 ± 9.9 to 10.6 ± 6.6 mSv (P = .0009). The lowest effective dose protocol for CTA was a combination of prospective gating and iterative reconstruction with an average exposure of 8.4 ± 4.3 mSv. In the SPECT MPI group, comparing patients with BMI < 30 kg·m−2 to those with a BMI ≥ 30 kg·m−2, the non-obese patients had a significantly smaller effective dose than their obese counterparts (5.5 ± 3.2 vs 8.4 ± 2.8 mSv, P < .0001). Male patients received slightly more radiation than female patients (7.2 ± 3.7 vs 6.4 ± 3.1 mSv, P = .001). Using a stress-only protocol with the CZT camera resulted in the lowest effective dose in the stress testing group (not considering the ETT group which received no radiation) with an average exposure of 5.0 ± 1.9 mSv.
Propensity Score-Matched Cohort
Propensity score matching was employed to attempt to overcome the lack of randomization in this cohort. This model yielded a c-statistic of 0.68 for discrimination of CTA vs stress testing. The matched cohort was generated using a 1:1 matching algorithm with each CTA subject matched to one stress test subject, although when analyzed, the 2:1 matched model yielded similar results. After generating the propensity score, 28 CTA subjects were unable to be matched to stress test subjects, yielding a final matched cohort of 164 patients in each group. Baseline characteristics were well balanced in the matched cohort with no significant differences between groups (Table 8 in Appendix). The comparison of the endpoints in the propensity-matched groups can be seen in Table 7. This matching resulted in similar findings to the total cohort analysis. Once again, more functional stress tests and total follow-up studies within 3 months were seen in the CTA cohort than in the stress testing group. Radiation exposure remained higher in the CTA group than the stress testing group (13.0 ± 8.9 vs 4.2 ± 4.1 mSv, P < .0001). The time to disposition was again significantly shorter in the CTA group. The increased proportion of revascularizations in the CTA group reached statistical significance where it had been borderline in the large cohort (7.3% vs 1.2%, P = .01). The other new finding was a statistically significant greater number of patients returning to the ED for cardiac visits in the CTA group compared to the stress testing group (6.1% vs 0.6%, P = .01).
Discussion
This study was a non-randomized study of real-world use of CTA and stress testing in the ED CPU, which also employed propensity matching, whose findings are complimentary to the recent randomized trial results.30 We found that both strategies performed well in their selected patient groups with low rates of subsequent testing and follow-up visits, and as such, choices for diagnostic testing should be individualized and no one test is appropriate for all patients as espoused by both professional societies.31-33 An equivalent number of normals (normal and non-obstructive disease) and obstructive disease were found in both groups. There were similar numbers of follow-up anatomic studies in both groups, but statistically significantly more follow-up functional studies and overall follow-up studies in the CTA group than the MPI group. CTA maintained its significant advantage in time to disposition and had a trend toward more revascularization procedures which neared statistical significance. Patient radiation exposure was found to be lower in the entire stress testing cohort and in the CZT MPI group than in the CTA group. The propensity score-matched cohort found similar results to those seen in the larger group.
The three recent randomized studies of CTA in the ED, CT-STAT, ACRIN PA 4005, and ROMICAT-II, all found that CTA was a safe and efficient diagnostic modality for the ED triage of chest pain.14,16,17 The current study confirmed the significant time savings of CTA in efficiently triaging patients. In the ACRIN PA 4005 and ROMICAT-II studies, direct discharge from the ED was more common in the CTA group although the use of observation units clouds the picture to some extent as “admission to the hospital” in ROMICAT-II was reduced only modestly with 25.4% vs 31.7%. In our study, the modest reduction in admissions favored the stress testing group (16.8% vs 25.0%), but was not statistically significant. Similar to ROMICAT-II, we found greater use of downstream testing in the CTA group, with similar amounts of follow-up angiograms, but increased number of functional studies. All trials reported a higher rate of coronary revascularization with CTA which met statistical significance in the propensity matched cohort, and like previous reports where 30-day cardiac return visits to the ED were similar, we found no significant difference in the proportion of return visits to the ED in the entire cohort. In the ROMICAT-II study conducted in 2010 and 2011, the mean radiation exposure per CTA patient was 13.9 ± 10.4 mSv which was similar to this study cohort, although a different conversion factor was employed. The 4.7 ± 8.4 mSv in the standard evaluation group was also similar to our stress testing group as it included stress echocardiography and ETT as well as MPI.
Despite there being more cardiac risk factors and more cardiac disease in the stress testing group, the incidence of obstructive CAD on subsequent invasive angiogram was not statistically different, suggesting that CTA has better sensitivity for the detection of obstructive disease as well as having the ability to detect pre-clinical disease. The early identification of non-obstructive plaque may allow for disease progression modification with the intensification of preventative therapy. More CTA studies were followed by functional studies (5.2% vs 0.5%, P < .0001) as perhaps physicians have greater comfort treating a low- to intermediate-risk abnormal MPI medically, whereas abnormal CTAs with intermediate grade stenosis must be confirmed by another study to prove that they did not underestimate the severity of stenosis. This phenomenon was perhaps also seen by the finding that an abnormal CTA was followed by another study 50% of the time compared to 38% for abnormal stress tests. The frequency of follow-up coronary angiographies was similar in both groups (8.3% vs 6.2%) and was appropriately driven by detection of disease by either technique. The increase in the number of revascularizations in the CTA group (59% vs 40%) was likely related to finding more obstructive CAD (63.6% vs 47.8%) on the follow-up invasive angiograms.
Using a combination of ETT and high efficiency SPECT imaging in most patients needing MPI, and employing a stress-first protocol in the majority of the ED CPU patients (80%), radiation exposure was lower for the stress testing group when compared to the CTA cohort (5.0 vs 12.6-13.5 mSv, P < .0001). The newer MPI paradigm of CZT SPECT and stress-only protocols exposed the patients to less radiation even when prospective gating was used for CTA (5.0 vs 9.9-10.7 mSv, P < .0001) in patients with similar BMIs (28.5 vs 28.9 kg·m−2). Two recently derived cardiac, scanner-specific conversion factors were used to calculate effective dose for the CTA patients in this study, but if the older conversion factor of 0.014 was used,34 the effective dose in the CTA cohort fell to 6.8 ± 4.6 mSv. The patients who underwent ETT of course received no radiation exposure and were assigned to this testing modality because they were the youngest, with the fewest cardiac risk factors and lowest pre-test risk. Stress echocardiography which was not used in this study would provide a similarly efficient testing modality without radiation exposure, but would be suitable for higher-risk patients given the greater sensitivity and specificity of the modality.
CTA maintains a significant advantage in the time to diagnosis over the stress testing group given the brevity of the test and the lack of the need to wait 4-6 hours for a second set of cardiac enzymes. There are several possible ways that stress testing could decrease its test time and become more comparable to the performance of CTA. With the introduction of high-sensitivity troponins, the current waiting time might be abolished with a “rule out” accomplished in 1 hour.35,36 Stress-only adenosine could be done after one set of cardiac biomarkers as adenosine has been shown to be safe even in acute MI.37 As in this study, using a stress-only protocol instead of a rest-stress protocol and a CZT SPECT camera to decrease imaging time from 20-25 to 3-5 minutes, extraneous time can be eliminated. ETT is an even faster diagnostic test for the low-risk patient and a provisional isotope injection protocol might provide the time savings of ETT with the flexibility of imaging when needed.38
More progress can and has been made at reducing patient radiation exposure with both CTA and SPECT MPI since 2011. CTA has made great strides in a short period of time through software, hardware, and protocol advances.39 Prospective ECG-triggered scanning instead of retrospectively ECG-gated helical scanning, iterative image reconstruction software, dual-source scanners, reducing tube potential, tube current modulation, and decreasing scan length by reducing z-overscanning are all techniques which are employed with increasing frequency even in the short time since the end of this study period.40 CTA can now be performed in selected patients with effective doses of 1-2 mSv.41,42 In this study, 152 (79%) of the CTA patients also had a calcium score performed which contributed to the overall radiation exposure (the mean effective dose was 1.8 mSv greater in patients who had a calcium score performed compared to patients who did not have one). Reductions in radiation exposure in the MPI field are being driven by innovations in stress protocols and new camera technology.13,43 High-efficiency SPECT cameras have been shown to reduce radiation exposure to 5.8 mSv for a full rest-stress study and to 1 mSv for a stress-only study.44,45 The use of ½ time imaging software which incorporates iterative image reconstruction with resolution recovery thereby improving count statistics can decrease imaging time or decrease injected activity.46 Stress protocol changes such as performing more ETTs,47 developing a provisional isotope injection protocol,38 and stress-first imaging10 will all decrease radiation exposure to the patient by not giving it in the first place. Perhaps the greatest saving of radiation exposure and resources would be the elimination of any diagnostic testing for most of the very low- and low-risk patients (“less is more”).48
Limitations
The study is limited by its retrospective, non-randomized nature and the single-site, clinical experience. This assortment of patients, despite the greater proportion of patients studied by stress testing, does represent current clinical practice in an urban teaching hospital with a diverse population pool over a two-year period of time. Propensity score matching was used as an attempt to overcome the lack of randomization. Results of follow-up diagnostic testing and follow-up visits to the ED were only available if performed at our institution. Stress echocardiography is not routinely available at our institution for the ED CPU population and was not included, but is a viable option for stress testing in an ED population without radiation exposure and with higher accuracy than ETT alone. The selection of diagnostic imaging study, CTA vs stress testing, was made at the discretion of the ED attending physician and should reflect current ED practice. The decision to perform ETT without imaging was made at the discretion of the Nuclear Cardiology Attending based on a patient’s pre-test risk of CAD. Subsequent endpoints such as major adverse cardiac events (non-fatal myocardial infarction, unstable angina, and cardiac mortality) were not identified and not used in this study. We did not evaluate the costs associated with each diagnostic strategy. Efforts to decrease radiation exposure are continuing with both modalities, and lower patient exposure is more possible now in 2013 than in 2010-2011. However, attention to radiation exposure has been emphasized at our institution as far back as 2007.49,50 Iterative reconstruction upgrades to the CT scanner were installed at the end of 2010 and resulted in a further decrease in radiation exposure. There is ongoing controversy on how to calculate effective dose from CTA so we used two of the recently published conversion factors derived specifically for cardiac studies to be as current as possible.21,22 The older, more commonly used conversion factor of 0.014 was originally from the 2004 European Guidelines for Multislice Computed Tomography Appendix C based on work by Shrimpton et al using single-slice scanners.34 Effective dose from nuclear cardiology procedures was estimated using the most recent ICRP effective dose conversion factors for Tc-99m sestamibi, which are based on tissue-weighting factors from ICRP Publication 80, while CTA conversion factors were based on tissue-weighting factors from ICRP Publication 103. The MPI conversion factors would change little if recalculated based on ICRP Publication 103 tissue-weighting factors; specifically, they would result in estimates of effective dose ~5% less than those we report.
New Knowledge Gained
CPU triage strategies of stress testing, including high-efficiency SPECT MPI and ETT, and CTA compare favorably and perform well in this patient population. Modern SPECT technology and stress protocols have significant advantages over older techniques and have advantages and disadvantages compared to modern CTA.
Conclusions
Stress testing including ETT, high-efficiency SPECT MPI, and stress-only protocols had a significantly lower patient radiation dose, less follow-up diagnostic testing, and similar cardiac return visits to the ED than CTA. CTA had a shorter time to disposition than stress testing and a trend, although not quite statistically significant, toward more revascularization procedures.
References
Amsterdam EA, Kirk JD, Bluemke DA, Diercks D, Farkouh ME, Garvey JL, et al. Testing of low-risk patients presenting to the emergency department with chest pain: A scientific statement from the American Heart Association. Circulation 2010;122:1756-76.
Graff L, Joseph T, Andelman R, Bahr R, DeHart D, Espinosa J, et al. American College of Emergency Physicians information paper: Chest pain units in emergency departments—A report from the Short-Term Observation Services Section. Am J Cardiol 1995;76:1036-9.
Miller JM, Rochitte CE, Dewey M, Arbab-Zadeh A, Niinuma H, Gottlieb I, et al. Diagnostic performance of coronary angiography by 64-row CT. N Engl J Med 2008;359:2324-36.
Stein PD, Yaekoub AY, Matta F, Sostman HD. 64-slice CT for diagnosis of coronary artery disease: A systematic review. Am J Med 2008;121:715-25.
Sharma A, Arbab-Zadeh A. Assessment of coronary heart disease by CT angiography: Current and evolving applications. J Nucl Cardiol 2012;19:796-806.
Shaw LJ, Hendel R, Borges-Neto S, Lauer MS, Alazraki N, Burnette J, et al. Prognostic value of normal exercise and adenosine (99m)Tc-tetrofosmin SPECT imaging: Results from the multicenter registry of 4,728 patients. J Nucl Med 2003;44:134-9.
Gibson PB, Demus D, Noto R, Hudson W, Johnson LL. Low event rate for stress-only perfusion imaging in patients evaluated for chest pain. J Am Coll Cardiol 2002;39:999-1004.
Chang SM, Nabi F, Xu J, Raza U, Mahmarian JJ. Normal stress-only versus standard stress/rest myocardial perfusion imaging: Similar patient mortality with reduced radiation exposure. J Am Coll Cardiol 2010;55:221-30.
Duvall WL, Wijetunga MN, Klein TM, Razzouk L, Godbold J, Croft LB, et al. The prognosis of a normal stress-only Tc-99m myocardial perfusion imaging study. J Nucl Cardiol 2010;17:370-7.
Duvall WL, Wijetunga MN, Klein TM, Hingorani R, Bewley B, Khan SM, et al. Stress-only Tc-99m myocardial perfusion imaging in an emergency department chest pain unit. J Emerg Med 2011;42:642-50.
Slomka PJ, Patton JA, Berman DS, Germano G. Advances in technical aspects of myocardial perfusion SPECT imaging. J Nucl Cardiol 2009;16:255-76.
Garcia EV, Faber TL, Esteves FP. Cardiac dedicated ultrafast SPECT cameras: New designs and clinical implications. J Nucl Med 2011;52:210-7.
Henzlova MJ, Duvall WL. The future of SPECT MPI: Time and dose reduction. J Nucl Cardiol 2011;18:580-7.
Goldstein JA, Chinnaiyan KM, Abidov A, Achenbach S, Berman DS, Hayes SW, et al. The CT-STAT (Coronary Computed Tomographic Angiography for Systematic Triage of Acute Chest Pain Patients to Treatment) trial. J Am Coll Cardiol 2011;58:1414-22.
Hoffmann U, Bamberg F, Chae CU, Nichols JH, Rogers IS, Seneviratne SK, et al. Coronary computed tomography angiography for early triage of patients with acute chest pain: The ROMICAT (Rule Out Myocardial Infarction using Computer Assisted Tomography) trial. J Am Coll Cardiol 2009;53:1642-50.
Litt HI, Gatsonis C, Snyder B, Singh H, Miller CD, Entrikin DW, et al. CT angiography for safe discharge of patients with possible acute coronary syndromes. N Engl J Med 2012;366:1393-403.
Hoffmann U, Truong QA, Schoenfeld DA, Chou ET, Woodard PK, Nagurney JT, et al. Coronary CT angiography versus standard evaluation in acute chest pain. N Engl J Med 2012;367:299-308.
Samad Z, Hakeem A, Mahmood SS, Pieper K, Patel MR, Simel DL, et al. A meta-analysis and systematic review of computed tomography angiography as a diagnostic triage tool for patients with chest pain presenting to the emergency department. J Nucl Cardiol 2012;19:364-76.
Hulten E, Pickett C, Bittencourt MS, Villines TC, Petrillo S, Di Carli MF, et al. Outcomes after coronary computed tomography angiography in the emergency department. J Am Coll Cardiol 2013;61:880-92.
Hendel RC, Berman DS, Di Carli MF, Heidenreich PA, Henkin RE, Pellikka PA, et al. ACCF/ASNC/ACR/AHA/ASE/SCCT/SCMR/SNM 2009 appropriate use criteria for cardiac radionuclide imaging: A report of the American College of Cardiology Foundation Appropriate Use Criteria Task Force, the American Society of Nuclear Cardiology, the American College of Radiology, the American Heart Association, the American Society of Echocardiography, the Society of Cardiovascular Computed Tomography, the Society for Cardiovascular Magnetic Resonance, and the Society of Nuclear Medicine. Circulation 2009;119:e561-87.
Gosling O, Loader R, Venables P, Rowles N, Morgan-Hughes G, Roobottom C. Cardiac CT: Are we underestimating the dose? A radiation dose study utilizing the 2007 ICRP tissue weighting factors and a cardiac specific scan volume. Clin Radiol 2010;65:1013-7.
Huda W, Tipnis S, Sterzik A, Schoepf UJ. Computing effective dose in cardiac CT. Phys Med Biol 2010;55:3675-84.
ICRP. Radiation dose to patients from radiopharmaceuticals (addendum 2 to ICRP publication 53). Ann ICRP 1998;28:1-126.
Abbara S, Arbab-Zadeh A, Callister TQ, Desai MY, Mamuya W, Thomson L, et al. SCCT guidelines for performance of coronary computed tomographic angiography: A report of the Society of Cardiovascular Computed Tomography Guidelines Committee. J Cardiovasc Comput Tomogr 2009;3:190-204.
Rubinshtein R, Gaspar T, Halon DA, Goldstein J, Peled N, Lewis BS. Prevalence and extent of obstructive coronary artery disease in patients with zero or low calcium score undergoing 64-slice cardiac multidetector computed tomography for evaluation of a chest pain syndrome. Am J Cardiol 2007;99:472-5.
Goldstein JA, Gallagher MJ, O’Neill WW, Ross MA, O’Neil BJ, Raff GL. A randomized controlled trial of multi-slice coronary computed tomography for evaluation of acute chest pain. J Am Coll Cardiol 2007;49:863-71.
Hansen CL, Goldstein RA, Berman DS, Churchwell KB, Cooke CD, Corbett JR, et al. Myocardial perfusion and function single photon emission computed tomography. J Nucl Cardiol 2006;13:e97-120.
Holly TA, Abbott BG, Al-Mallah M, Calnon DA, Cohen MC, DiFilippo FP, et al. Single photon-emission computed tomography. J Nucl Cardiol 2010;17:941-73.
Henzlova MJ, Cerqueira MD, Hansen CL, Taillefer R, Yao SS. ASNC imaging guidelines for nuclear cardiology procedures: Stress protocols and tracers. J Nucl Cardiol 2009;16:331.
Califf RM, Sanderson I, Miranda ML. The future of cardiovascular clinical research: Informatics, clinical investigators, and community engagement. JAMA 2012;308:1747-8.
Depuey EG, Mahmarian JJ, Miller TD, Einstein AJ, Hansen CL, Holly TA, et al. Patient-centered imaging. J Nucl Cardiol 2012;19:185-215.
Sun Z, Aziz YF, Ng KH. Coronary CT angiography: How should physicians use it wisely and when do physicians request it appropriately? Eur J Radiol 2012;81:e684-7.
Berman DS, Hachamovitch R, Shaw LJ, Friedman JD, Hayes SW, Thomson LE, et al. Roles of nuclear cardiology, cardiac computed tomography, and cardiac magnetic resonance: Noninvasive risk stratification and a conceptual framework for the selection of noninvasive imaging tests in patients with known or suspected coronary artery disease. J Nucl Med 2006;47:1107-18.
Bongartz G, Golding SJ, Jurik AG, Leonardi M, van Persijn van Meerten E, Rodriguez R, et al. European Guidelines for Multislice Computed Tomography; March 2004. www.msct.eu/CT_Quality_Criteria.htm. Accessed 4 Apr 2013.
Reichlin T, Schindler C, Drexler B, Twerenbold R, Reiter M, Zellweger C, et al. One-hour rule-out and rule-in of acute myocardial infarction using high-sensitivity cardiac troponin T. Arch Intern Med 2012;172:1211-8.
Body R, Carley S, McDowell G, Jaffe AS, France M, Cruickshank K, et al. Rapid exclusion of acute myocardial infarction in patients with undetectable troponin using a high-sensitivity assay. J Am Coll Cardiol 2011;58:1332-9.
Mahmarian JJ, Shaw LJ, Filipchuk NG, Dakik HA, Iskander SS, Ruddy TD, et al. A multinational study to establish the value of early adenosine technetium-99m sestamibi myocardial perfusion imaging in identifying a low-risk group for early hospital discharge after acute myocardial infarction. J Am Coll Cardiol 2006;48:2448-57.
Duvall WL, Levine EJ, Moonthungal S, Fardanesh M, Croft LB, Henzlova MJ. A hypothetical protocol for the provisional use of perfusion imaging with exercise stress testing. J Nucl Cardiol 2013;2:739-47.
Halliburton S, Arbab-Zadeh A, Dey D, Einstein AJ, Gentry R, George RT, et al. State-of-the-art in CT hardware and scan modes for cardiovascular CT. J Cardiovasc Comput Tomogr 2012;6:154-63.
Halliburton SS, Abbara S, Chen MY, Gentry R, Mahesh M, Raff GL, et al. SCCT guidelines on radiation dose and dose-optimization strategies in cardiovascular CT. J Cardiovasc Comput Tomogr 2011;5:198-224.
Sabarudin A, Sun Z, Ng KH. A systematic review of radiation dose associated with different generations of multidetector CT coronary angiography. J Med Imaging Radiat Oncol 2012;56:5-17.
Hou Y, Xu S, Guo W, Vembar M, Guo Q. The optimal dose reduction level using iterative reconstruction with prospective ECG-triggered coronary CTA using 256-slice MDCT. Eur J Radiol 2012;81:3905-11.
Slomka PJ, Dey D, Duvall WL, Henzlova MJ, Berman DS, Germano G. Advances in nuclear cardiac instrumentation with a view towards reduced radiation exposure. Curr Cardiol Rep 2012;14:208-16.
Duvall WL, Croft LB, Ginsberg ES, Einstein AJ, Guma KA, George T, et al. Reduced isotope dose and imaging time with a high-efficiency CZT SPECT camera. J Nucl Cardiol 2011;18:847-57.
Bateman TM, McGhie A, Courter S, Burgett E, Cullom SJ, Case J. Prospective study of ultra-low dose stress-only solid-state SPECT: Comparison of efficiency, dosimetry and outcomes versus traditional-dose attenuation-corrected stress-only anger SPECT. J Am Coll Cardiol 2012;59:E1316.
Borges-Neto S, Pagnanelli RA, Shaw LK, Honeycutt E, Shwartz SC, Adams GL, et al. Clinical results of a novel wide beam reconstruction method for shortening scan time of Tc-99m cardiac SPECT perfusion studies. J Nucl Cardiol 2007;14:555-65.
Blankstein R, Ahmed W, Bamberg F, Rogers IS, Schlett CL, Nasir K, et al. Comparison of exercise treadmill testing with cardiac computed tomography angiography among patients presenting to the emergency room with chest pain: The Rule Out Myocardial Infarction Using Computer-Assisted Tomography (ROMICAT) study. Circ Cardiovasc Imaging 2012;5:233-42.
Prasad V, Cheung M, Cifu A. Chest pain in the emergency department: The case against our current practice of routine noninvasive testing. Arch Intern Med 2012;172:1-3.
Einstein AJ, Henzlova MJ, Rajagopalan S. Estimating risk of cancer associated with radiation exposure from 64-slice computed tomography coronary angiography. JAMA 2007;298:317-23.
Einstein AJ, Moser KW, Thompson RC, Cerqueira MD, Henzlova MJ. Radiation dose to patients from cardiac diagnostic imaging. Circulation 2007;116:1290-305.
Disclosures
The authors have nothing to disclose in relation to this research.
Author information
Authors and Affiliations
Corresponding author
Additional information
Funding
Mount Sinai School of Medicine; no outside sources of funding
Appendix
Rights and permissions
About this article
Cite this article
Duvall, W.L., Savino, J.A., Levine, E.J. et al. A comparison of coronary CTA and stress testing using high-efficiency SPECT MPI for the evaluation of chest pain in the emergency department. J. Nucl. Cardiol. 21, 305–318 (2014). https://doi.org/10.1007/s12350-013-9823-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12350-013-9823-y