Abstract
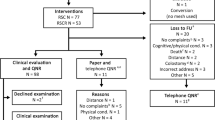
Awareness and reporting of mesh-related complications of pelvic organ prolapse repairs have increased in recent years. As a result, deciding whether to use a mesh or not has become a difficult task for urogynecologists. Our aim was to summarize reasons for and against the use of mesh in prolapse repair based on a review of relevant literature. Scopus and PubMed databases were searched for papers reporting on the efficacy and safety of native tissue versus non-absorbable, synthetic mesh prolapse repairs. Randomized controlled trials, systematic reviews, and meta-analyses were included. Evidence is presented for each vaginal compartment separately. In the anterior compartment, mesh repairs seem to offer clearly superior efficacy and durability of results compared to native tissue repairs, but with an equally clear increase in complication rates. In the isolated posterior compartment prolapse, high-quality evidence is sparse. As far as the apical compartment is concerned, sacrocolpopexy is the most efficacious, yet the most invasive procedure. Data on the comparison of transvaginal mesh versus native tissue repairs of the apical compartment are somewhat ambiguous. Given the inevitable coexistence of advantages and disadvantages of mesh use in each of the prolapsed vaginal compartments, an individualized treatment decision, based on weighing risks against benefits for each patient, seems to be the most rational approach.
Similar content being viewed by others
Introduction
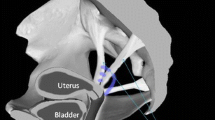
Pelvic organ prolapse (POP) is the sign of descent of one or more of the following: the anterior vaginal wall, the posterior vaginal wall, the uterus (cervix) or the apex of the vagina (vaginal vault or cuff scar after hysterectomy) [1]. Its prevalence is currently estimated to be approximately 40% in women 45–85 years of age, and around 30% of these women are symptomatic [2]. Symptomatic patients may complain of urinary, bowel, or sexual symptoms as well as symptoms of vaginal pressure, heaviness, or pain [3]. These symptoms have a major impact on patients’ physical and emotional well-being [4].
The pelvic organs can descend, as mentioned in the definition, in any of the three different anatomical compartments: the anterior, the posterior, and the apical, or in more than one compartment. The degree of pelvic organ descent was initially quantified using the Baden–Walker halfway scoring system [5]. However, the POP-Q grading system [6], with proven interobserver and intraobserver reliability [7], is more commonly used in the literature in the past few years [8].
Treatment of POP is commonly surgical [9] and the lifetime risk of undergoing a pelvic reconstruction surgery is estimated at about 11.8% by the age of 80 years [10]. The surgical prolapse repair aims primarily at restoring the anatomy of the structures supporting the pelvic organs. These structures have been described and classified in three different levels in the landmark paper by DeLancey [11].
Several techniques are available for pelvic organ prolapse repair. Depending on the material used to restore pelvic organ support, these techniques are classified as “native tissue repairs” when only pelvic organ support tissues are used or “reinforced or augmented repairs” when some other material is used to reinforce the defective support system. These include autologous or heterologous biological or synthetic, absorbable or non-absorbable, materials. As native tissue repairs showed discouraging rates of surgical failure in early studies [12, 13], reinforced repairs, using mainly synthetic mesh materials, became more popular [14]. This trend was facilitated by the marketing of numerous mesh kits (containing meshes and special introducing instruments), which were mainly used by the transvaginal route [15]. Approximately a decade later, complications of mesh usage started to emerge [16], leading to the US Food and Drug Administration (FDA) safety warnings regarding mesh complications, especially for meshes placed transvaginally [17].
Given the dilemmas regarding mesh use in pelvic reconstructive surgery, we aimed to summarize reasons for and against it based on a review of the current literature. The literature search was conducted in Scopus and PubMed databases until May 2016, for English-language papers on the efficacy and safety of native tissue versus non-absorbable, synthetic mesh prolapse repairs. Randomized controlled trials were included. Results of systematic reviews and meta-analyses were also included without reporting individual trials, for reasons of brevity. As the balance of benefits and disadvantages from native tissue or mesh augmented repairs may vary according to the prolapsed compartment, evidence is organized under anterior, posterior, and apical compartment prolapse.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not involve any new studies of human or animal subjects performed by any of the authors.
Results
Anterior Compartment Prolapse
Reasons For Using a Mesh
The main argument for using a mesh in the anterior repair would be its superior efficacy and durability in treating the signs and symptoms of prolapse, compared to native tissue repairs, with fewer recurrences and reoperations.
In the 2016 Cochrane systematic review on transvaginal permanent mesh repair versus native tissue repair [18], 15 trials were included in the meta-analysis of data concerning the anterior compartment: recurrent prolapse was demonstrated in 12.2% (107/870) of the patients who underwent a mesh repair compared to 39.6% (348/878) of the patients who underwent an anterior colporrhaphy (RR 0.33 and Tau2 = 0.02, Chi2 = 15.51, I 2 = 10%).
The high anatomic cure rates of around 90% with mesh repairs were evident in early mesh studies [19–21] and were later confirmed by several others [22–25]. A recent multicenter randomized controlled study compared the Avaulta® Plus anterior biosynthetic mesh procedure, with anterior colporrhaphy in a total of 138 women (70 and 68 women, respectively) [26]. The patients were 55 years old or older and had at least stage 2 anterior vaginal wall prolapse according to the POP-Q system. Anatomical success was defined as less than stage 2. At 3 years follow-up, the objective anatomic cure rate was 91.4% for the mesh group and 41.2% for the colporrhaphy group. A more recent randomized study also showed a significant difference of efficacy between the trocar-guided Nazca TC® kit and anterior colporrhaphy groups [27]. The trial reported on 86 patients with an anterior compartment prolapse stage 2 or more, according to the POP-Q system. The anatomical success rates, defined as Ba < 0, were 74.4% and 51.1% at 2 years follow-up (p = 0.022), for the mesh and native tissue repair groups, respectively.
Apart from superior objective efficacy, using a mesh seems to offer better prolapse symptom improvement, compared to native tissue repairs. In a prospective randomized controlled study, 68 patients were randomized into a native tissue repair group (n = 35) and the Perigee® transobturator anterior compartment repair system (n = 33) [28]. Patients had POP-Q stage 3 or 4 anterior compartment prolapse. Subjective awareness of prolapse was one of the study’s secondary outcomes. At 2 years follow-up, 5 out of 33 women in the mesh group (15.1%) were aware of the prolapse compared to 9 out of 35 women in the colporrhaphy group (25.7%). Similar results have been published by several previous randomized studies in the last 5 years [29–32].
The higher rates of objective and subjective cure rates with mesh repairs lead to lower rates of repeat surgery for prolapse. In a randomized controlled study, 201 patients underwent an anterior colporrhaphy or a mesh repair using the transobturator Ugytex® mesh (97 and 104 patients, respectively) [32]. The follow-up was set at 3 years, the recurrence of the prolapse was the primary endpoint, and the reoperation rate for prolapse was a secondary endpoint of the study. The authors found superior outcomes with mesh repair both for prolapse recurrence and reoperation. In the mesh group, 5.7% (6/104) women were reoperated on for recurrent prolapse compared to 10.3% (10/97) in the anterior colporrhaphy group. Similar results were published by another randomized controlled trial with short-term follow-up (6 months), where 56 women underwent a native tissue repair and 58 women a mesh repair for the anterior compartment [33]. While the primary endpoint of the study was sexual function, the study included the reoperation rate for prolapse as a secondary outcome: it was 7.1% (4/56 patients) in the native tissue repair group and 5.1% (3/58 patients) in the mesh group.
Reasons Against Using a Mesh
The main reason for not using a mesh in the anterior compartment is mesh-related complications including, primarily, mesh exposure for which a woman undergoing a native tissue repair has no risk. In the most recent meta-analysis of transvaginal mesh versus native tissue repairs, 14 randomized trials for the anterior compartment repair were analyzed [18]. The meta-analysis showed that mesh exposure was noted in 10.1% (76/753) of women after anterior mesh repair. In the same meta-analysis, 15 randomized trials (933 women) were included in the analysis for the rate of surgical intervention for mesh exposure in the anterior compartment. It was found that 7.7% (72/933) of women who underwent a mesh repair also had surgery for mesh exposure. This evidence is further supported by recent studies [26, 27].
Another reason against the use of meshes is the apparently increased rates of de novo stress urinary incontinence with mesh repairs in the anterior compartment. The most recent Cochrane review analyzed 12 randomized trials of transvaginal mesh repair versus native tissue repair to estimate the incidence of new stress urinary incontinence after surgery [18]. The follow-up of the studies was 1–3 years. The meta-analysis showed that 133 per 1000 women developed de novo stress urinary incontinence after mesh surgery compared to 96 per 1000 women after a native tissue repair. These findings are further supported by a recently published randomized controlled trial with a follow-up of 3 years [26]. Seventy women underwent anterior prolapse surgery using the Avaulta® Plus anterior biosynthetic mesh procedure and 68 women anterior colporrhaphy. Despite the higher anatomic cure rates in the mesh group, the rates of de novo stress urinary incontinence were lower in the anterior colporrhaphy group: 1.4% (1 of 68 patients) compared to 8.5% (6 of 70 patients) in the mesh group.
The increased rate of intraoperative bladder injury is another reason against using a mesh. This is supported by the results of a multicenter, parallel-group randomized controlled trial comparing a trocar-guided, transvaginal transobturator polypropylene-mesh repair kit, the Gynecare® Prolift Anterior Pelvic Floor Repair System, with anterior colporrhaphy [31]. The authors used the POP-Q system to quantify prolapse and set a composite anatomical and a functional outcome for efficacy evaluation: both Ba < −1 and subjective absence of vaginal bulging. A total of 389 patients were included, with 200 women undergoing the mesh kit repair and 189 women the anterior colporrhaphy. Despite a higher rate of success for the mesh group, bladder injury rate was lower in the colporrhaphy group: 0.5% (only 1 out of 183 patients) in the colporrhaphy group compared to 3.7% (7 out of 186 women) in the mesh group.
Posterior Compartment Prolapse
Similar to anterior compartment prolapse repair, the main argument for mesh use in the posterior compartment would be superior efficacy and durability of results, compared to native tissue repairs. Mesh-related complications would be the main argument against mesh use.
Several prospective and retrospective case series have demonstrated the high efficacy and safety of either mesh-augmented [34] or native tissue repairs [35–39]. Success rates in the range of 76–88% have been described, depending on the definition of success and length of follow-up.
Our literature search did not return any randomized controlled trials comparing permanent mesh repair with native tissue repair in isolated posterior compartment prolapse. Nevertheless, indirect data for the posterior compartment are available from randomized trials of patients with multicompartment prolapse, where restoration of apical support was the primary outcome. Τhe 2016 Cochrane systematic review and meta-analysis [18] summarized the results of three trials [40–42] of apical prolapse repairs, with optional concomitant anterior/posterior repairs, where follow-up data on the posterior compartment were reported. Data showed no statistically or clinically significant difference in objective failure rates in the posterior compartment between mesh and no mesh repairs of multicompartment prolapse: failure rate was 7.4% (8 of 107 repairs) with mesh repairs compared to 11.7% (14 of 119 repairs) with native tissue repairs (p = 0.92).
Apical Compartment Prolapse (Uterine-Vaginal Apex Vault)
The main argument for using a mesh to reinforce apical compartment prolapse repairs is the same as in other compartments: its superior efficacy and durability in treating prolapse, compared to native tissue repairs, with fewer recurrences and reoperations. An increased rate of adverse events would similarly be an argument against use of mesh. Nevertheless, the apical compartment represents some particularities in comparison to the others. The first is that because of the anatomical configuration of the pelvic organ support system [11], prolapse of the vaginal apex is frequently associated with defects in the anterior and posterior vaginal compartments. The second one is that there are two completely different modes of applying the mesh: the abdominal route and the vaginal route. Placing a mesh transabdominally, i.e., performing a sacrocolpopexy, can be done through open, laparoscopic or robotic-assisted approaches. Native tissue prolapse repairs are done transvaginally and include McCall’s culdoplasty/sacrospinous ligament fixation (SSLF), iliococcygeus fixation (ICS), and uterosacral ligament suspension (USLS). Because of the differences in the very nature of the surgical procedures, sacrocolpopexy and transvaginal mesh repairs are considered, and compared to native tissue repairs, separately below.
Mesh Sacrocolpopexy Versus Native Tissue Repairs
The 2013 Cochrane review on the surgical management of pelvic organ prolapse [9] reported five randomized controlled trials comparing sacrocolpopexy (open) to native tissue repairs. In four out of the five trials success rates were better for sacrocolpopexy: they ranged from 59% to 100% while they were 28–82% in native tissue repairs. Only one trial [43] reported better outcomes with native tissue repair: 87% with uterosacral ligament fixation versus 68% with open sacrocolpopexy. It has to be mentioned though that the outcome in this trial was subjective improvement of prolapse symptoms and that vaginal hysterectomy in the native tissue group was compared to uterine preservation in the abdominal group. On the basis of the above evidence, the authors of the Cochrane review concluded that sacrocolpopexy offers higher correction rates for apical vaginal prolapse compared to native tissue procedures. This conclusion was confirmed by another systematic review and meta-analysis of sacrocolpopexy versus native tissue repair published in 2015 [44].
Efficacy data from the aforementioned meta-analyses suggest that abdominal sacrocolpopexy may be preferred in comparison to native tissue repairs. However, for open sacrocolpopexy operating and recovery time was longer and cost was higher, compared to native tissue procedures. Adverse events were also more frequent: compiled data from 79 studies [44] showed higher incidences of bowel (2.7% compared to 0.2%, p < 0.01), mesh and suture (4.2% compared with 0.4%, p < 0.01), and thromboembolic adverse events (0.6% compared with 0.1%, p = 0.03) after mesh sacrocolpopexy compared with native tissue vaginal repairs. In sacrocolpopexy trials included in the 2013 Cochrane review, mesh exposure rates ranged from 2% to 10.7%. Furthermore, sacrocolpopexy may not be suitable for patients with significant medical and surgical comorbidities. Minimally invasive sacrocolpopexy, either laparoscopic or robot-assisted, promises to reduce limitations and adverse events of the open approach but relevant evidence has not yet matured [45] and such a comparison is beyond the scope of the present review.
Transvaginal Mesh Versus Native Tissue Repairs
The efficacy and safety of transvaginal mesh-augmented repairs compared to vaginal native tissue repairs for middle- or multi-compartment prolapse have been reported in four randomized controlled trials.
In 2012, outcomes of a double-blind, multicenter randomized controlled trial comparing traditional vaginal prolapse surgery without mesh and mesh repairs in patients with symptomatic POP-Q stage 2–4 prolapse were published [46]. No-mesh operations included anterior or posterior colporrhaphy, or both; uterosacral ligament suspension; or sacrospinous ligament fixation. Repair with mesh included synthetic mesh implant kits such as Anterior Prolift™, Modified Anterior Prolift™ with apical arms, or Total Prolift™. Sixty-five operations (33 mesh/32 no mesh) were done before the trial was halted as a result of a mesh exposure rate of 15.6% which did not match the predetermined safety criteria. At 12 months postoperatively, mesh use resulted in a higher reoperation rate and did not improve cure rates. Three-year follow-up data of the same trial were reported in 2013 [47]. Objective cure, defined as a composite of no prolapse beyond the hymen and adequate apical support, was 85% and 71% for mesh and no mesh, respectively, a difference that was not statistically significant (p = 0.45). Subjective cure, including lack of symptoms and satisfaction, was high in both groups, also with no statistical significance between them.
A multicenter randomized controlled study compared prolapse recurrence and complication rates for Prolift™ mesh repair and sacrospinous fixation in the treatment of post-hysterectomy vaginal vault prolapse [48]. A total of 168 patients were randomized, 85 to the mesh and 83 to the native tissue repair groups, respectively. Prolapse recurrence 1 year postoperatively was noted in 16.9% of the mesh group compared to 39.4% in the native tissue repair group (p = 0.003). The mesh exposure rate was 20.8%.
In 2014, another single-center, randomized trial compared the transvaginal mesh procedure Prolift® Total with sacrospinous fixation for post-hysterectomy vaginal vault prolapse [49]. Seventy patients with at least two-compartment prolapse were randomized into the mesh (n = 36) or the native tissue repair (n = 34) groups. One of the primary outcomes of the study was anatomical failure defined as prolapse to the level of the hymen or below at clinical examination. At 1-year follow-up anatomical failures were significantly less common in the mesh group: 3% (only one case) versus 65% (22 cases) in the native tissue repair group (p < 0.001). There were three cases (8%) of minor mesh exposure.
One more multicenter, randomized trial compared the polypropylene mesh repair Prolift™ to sacrospinous ligament fixation for apical defects as well other, site-specific, native tissue repairs in 184 women with POP-Q prolapse stage 3 or 4 [50]. Ninety-four patients underwent the mesh repair and 90 the native tissue repair. Prolapse was considered cured when the POP-Q point evaluation was equal to or less than 0 and POP-Q point C better than or equal to half the total vaginal length. At 1-year follow-up, anatomical cure rates were better in the mesh group in the anterior compartment (86.4% versus 70.4%, p = 0.019) but there was no statistically significant difference as far as the apical compartment is concerned (92% versus 84%, p = 0.165). There were 18 patients with mesh exposure (20%).
Discussion
The main advantage of mesh-augmented pelvic reconstruction is superior efficacy and durability of results compared to native tissue repairs. Indeed, the majority of studies confirm the benefits of mesh use in terms of increased success rates.
Nevertheless, interpreting such evidence and using it in clinical decision-making are not straightforward. First of all, there is significant variation in the definition of surgical success among studies [51]. Using different outcomes may have considerable impact on the results even of a single study. As an example, in a recent randomized controlled trial comparing vaginal mesh repair to anterior colporrhaphy, anatomic cure rates were 74.4% and 51.1%, respectively at 2 years, but dropped to 40% for each group when the definition of a successful outcome was changed from postoperative prolapse POP-Q stage 2 or less to stage 1 or less [27].
Caution is also advised when reoperation rates are interpreted as a measure of success. Very often reoperation rates for mesh repairs include procedures for stress urinary incontinence and mesh complications in addition to those for prolapse recurrence. The 2016 Cochrane systematic review and meta-analysis on vaginal prolapse repairs [18], for example, showed a significantly higher reoperation rate with mesh procedures (11.4% versus 4.8% with native tissue repairs) but this was driven predominantly, even though not exclusively, by reoperations due to mesh-related complications: reoperations for prolapse recurrences, specifically, were only slightly more common with mesh repairs (3.2% versus 1.7% in the native tissue group) while anti-incontinence procedures were similar (2.8% in the mesh group and 2.6% in the native tissue group).
Another issue when interpreting literature results on efficacy of repairs is that there is not a direct and predictable relationship between objective anatomical cure and subjective improvement of prolapse symptoms or overall patient satisfaction. Hopefully, future trials will indicate “how much anatomical correction” is needed if we are aiming primarily for satisfied women.
The increased efficacy of mesh-augmented repairs over native tissue ones comes with a cost of increased complications. Mesh exposure, in particular, is a mesh-specific complication and represents the most important safety concern. Fear of this complication has considerably altered clinical practice in recent years. It has to be admitted that mesh complications may have significant negative impact on patients’ quality of life and require multiple, on occasions, complex operations for their management. On the other hand, it has to be argued that not all mesh exposures require surgical intervention. Many of those are asymptomatic and are discovered incidentally during regular follow-up clinical examinations. In most cases such asymptomatic exposures do not require a surgical intervention and, in fact, the American Association of Urology recommends against mesh removal in asymptomatic patients [52].
As there are pros and cons in using a mesh in each vaginal compartment repair, the question whether to use it or not should be answered on an individual basis. When there is higher risk for prolapse recurrence, it becomes more reasonable to use a mesh repair. Prolapse stage 3 or 4 (POP-Q), age less than 60 years, diabetes mellitus, and recurrent prolapse are all factors associated with increased failure of native tissue repairs [53] and should be taken into consideration. On the other hand, it is of paramount importance to minimize complications, mesh exposure in particular, when mesh is used. Surgeon- and patient-related risk factors should be carefully addressed [54, 55].
Appropriate patient selection and information are the only current means of overcoming the dilemmas regarding the use of mesh in prolapse repairs. Data from ongoing and future trials will hopefully provide information for safer evidence-based decisions.
Conclusion
In the anterior compartment, mesh repairs are associated with better objective and subjective results, compared to native tissue repairs. In the same compartment, mesh-related complications, higher rates of de novo stress incontinence, and bladder injury are arguments against use of mesh. With regards to isolated posterior compartment prolapse, lack of high-quality evidence does not allow us to reach safe conclusions. In the apical compartment, sacrocolpopexy offers better results compared to the other surgical options and causes fewer mesh-related complications than transvaginal procedures, but is an invasive procedure. Minimally invasive, laparoscopic or robot-assisted, sacrocolpopexy promises to reproduce results of the open procedure.
References
Haylen BT, de Ridder D, Freeman RM, et al. An International Urogynecological Association (IUGA)/International Continence Society (ICS) joint report on the terminology for female pelvic floor dysfunction. Neurourol Urodyn. 2010;29(1):4–20.
Slieker-Ten Hove MCP, Pool-Goudzwaard AL, Eijkemans MJC, Steegers-Theunissen RPM, Burger CW, Vierhout ME. Prediction model and prognostic index to estimate clinically relevant pelvic organ prolapse in a general female population. Int Urogynecol J Pelvic Floor Dysfunct. 2009;20(9):1013–21.
Younger A, Rac G, Quentin C, et al. Pelvic organ prolapse surgery in academic female pelvic medicine and reconstructive surgery urology practice in the setting of the Food and Drug Administration public health notifications. Urology. 2016;91:46–50.
Abdel-Fattah M, Familusi A, Fielding S, Ford J, Bhattacharya S. Primary and repeat surgical treatment for female pelvic organ prolapse and incontinence in parous women in the UK: a register linkage study. BMJ Open. 2011;1(2):e000206.
Baden WF, Walker TA, Lindsey JH. The vaginal profile. Tex Med. 1968;64(5):56–8.
Bump RC, Mattiasson A, Bø K, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996;175(1):10–7.
Hall AF, Theofrastous JP, Cundiff GW, et al. Interobserver and intraobserver reliability of the proposed International Continence Society, Society of Gynecologic Surgeons, and American Urogynecologic Society pelvic organ prolapse classification system. Am J Obstet Gynecol. 1996;175(6):1467–71.
Muir TW, Stepp KJ, Barber MD. Adoption of the pelvic organ prolapse quantification system in peer-reviewed literature. Am J Obstet Gynecol. 2003;189(6):1632–6.
Maher C, Feiner B, Baessler K, Schmid C. Surgical management of pelvic organ prolapse in women. Cochrane Database Syst Rev. 2013;4:CD004014.
Fialkow MF, Newton KM, Lentz GM, Weiss NS. Lifetime risk of surgical management for pelvic organ prolapse or urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(3):437–40.
DeLancey JOL. Anatomic aspects of vaginal eversion after hysterectomy. Am J Obstet Gynecol. 1992;166(6 PART 1):1717–28.
Olsen AL, Smith VJ, Bergstrom JO, Colling JC, Clark AL. Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol. 1997;89(4):501–6.
Weber AM, Walters MD, Piedmonte MR, Ballard LA. Anterior colporrhaphy: a randomized trial of three surgical techniques. Am J Obstet Gynecol. 2001;185(6):1299–306.
Jonsson Funk M, Edenfield AL, Pate V, Visco AG, Weidner AC, Wu JM. Trends in use of surgical mesh for pelvic organ prolapse. Am J Obstet Gynecol. 2013;208(1):79.e1–7.
Kapur K, Dalal V. Mesh repair of vaginal wall prolapse. Med J Armed Forces India. 2014;70(2):105–10.
Maher C. Anterior vaginal compartment surgery. Int Urogynecol J Pelvic Floor Dysfunct. 2013;24(11):1791–802.
Food and Drug Administration. Safety communications—UPDATE on serious complications associated with transvaginal placement of surgical mesh for pelvic organ prolapse: FDA safety communication. 2011. http://www.fda.gov/MedicalDevices/Safety/AlertsandNotices/ucm262435.htm. Accessed 23 May 2016.
Maher C, Feiner B, Baessler K, Christmann-Schmid C, Haya N, Marjoribanks J. Transvaginal mesh or grafts compared with native tissue repair for vaginal prolapse. Cochrane Database Syst Rev. 2016;2:CD012079.
Nicita G. A new operation for genitourinary prolapse. J Urol. 1998;160(3 Pt 1):741–5.
Flood CG, Drutz HP, Waja L. Anterior colporrhaphy reinforced with Marlex mesh for the treatment of cystoceles. Int Urogynecol J Pelvic Floor Dysfunct. 1998;9(4):200–4.
Migliari R, De Angelis M, Madeddu G, Verdacchi T. Tension-free vaginal mesh repair for anterior vaginal wall prolapse. Eur Urol. 2000;38(2):151–5.
Nguyen J, Burchette R. Outcome after anterior vaginal prolapse repair: a randomized controlled trial. Obstet Gynecol. 2008;111(4):891–8.
Amrute KV, Eisenberg ER, Rastinehad AR, Kushner L, Badlani GH. Analysis of outcomes of single polypropylene mesh in total pelvic floor reconstruction. Neurourol Urodyn. 2007;26(1):53–8.
Jo H, Kim JW, Park NH, Kang SB, Lee HP, Song Y-S. Efficacy and outcome of anterior vaginal wall repair using polypropylene mesh (Gynemesh). J Obstet Gynaecol Res. 2007;33(5):700–4.
Cervigni M, Natale F, La Penna C, Panei M, Mako A. Transvaginal cystocele repair with polypropylene mesh using a tension-free technique. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19(4):489–96.
Rudnicki M, Laurikainen E, Pogosean R, Kinne I, Jakobsson U, Teleman P. A 3-year follow-up after anterior colporrhaphy compared with collagen-coated transvaginal mesh for anterior vaginal wall prolapse: a randomised controlled trial. BJOG Int J Obstet Gynaecol. 2016;123(1):136–42.
Dias MM, De AC, Bortolini MAT, et al. Two-years results of native tissue versus vaginal mesh repair in the treatment of anterior prolapse according to different success criteria: a randomized controlled trial. Neurourol Urodyn. 2016;35(4):509–14.
Lamblin G, Van-Nieuwenhuyse A, Chabert P, Lebail-Carval K, Moret S, Mellier G. A randomized controlled trial comparing anatomical and functional outcome between vaginal colposuspension and transvaginal mesh. Int Urogynecol J Pelvic Floor Dysfunct. 2014;25(7):961–70.
de Tayrac R, Cornille A, Eglin G, et al. Comparison between trans-obturator trans-vaginal mesh and traditional anterior colporrhaphy in the treatment of anterior vaginal wall prolapse: results of a French RCT. Int Urogynecol J. 2013;24(10):1651–61.
El-Nazer MA, Gomaa IA, Ismail Madkour WA, Swidan KH, El-Etriby MA. Anterior colporrhaphy versus repair with mesh for anterior vaginal wall prolapse: a comparative clinical study. Arch Gynecol Obstet. 2012;286(4):965–72.
Altman D, Väyrynen T, Engh ME, Axelsen S, Falconer C, Nordic Transvaginal Mesh Group. Anterior colporrhaphy versus transvaginal mesh for pelvic-organ prolapse. N Engl J Med. 2011;364(19):1826–36.
Nieminen K, Hiltunen R, Takala T, et al. Outcomes after anterior vaginal wall repair with mesh: a randomized, controlled trial with a 3 year follow-up. Am J Obstet Gynecol. 2010;203(3):235.e1–8.
Vollebregt A, Fischer K, Gietelink D, van der Vaart CH. Effects of vaginal prolapse surgery on sexuality in women and men; results from a RCT on repair with and without mesh. J Sex Med. 2012;9(4):1200–11.
Nyyssönen V, Santala M, Ala-Nissilä S, Bloigu R, Haarala M. Posterior transvaginal mesh without concurrent surgery: how does it have an effect on the untreated vaginal compartment. Gynecol Obstet Invest. 2016. doi:10.1159/000445742.
Abramov Y, Gandhi S, Goldberg RP, Botros SM, Kwon C, Sand PK. Site-specific rectocele repair compared with standard posterior colporrhaphy. Obstet Gynecol. 2005;105(2):314–8.
Arnold MW, Stewart WR, Aguilar PS. Rectocele repair. Four years’ experience. Dis Colon Rectum. 1990;33(8):684–7.
Mellgren A, Anzén B, Nilsson BY, et al. Results of rectocele repair. A prospective study. Dis Colon Rectum. 1995;38(1):7–13.
Kahn MA, Stanton SL. Posterior colporrhaphy: its effects on bowel and sexual function. BJOG Int J Obstet Gynaecol. 1997;104(1):82–6.
Maher CF, Qatawneh AM, Baessler K, Schluter PJ. Midline rectovaginal fascial plication for repair of rectocele and obstructed defecation. Obstet Gynecol. 2004;104(4):685–9.
Meschia M, Gattei U, Pifarotti P, Spennacchio M, Longatti D, Barbacini P. Randomized comparison between infracoccygeal sacropexy (posterior IVS) and sacrospinous ligament fixation in the management of vault prolapse. http://www.ics.org/Abstracts/Publish/42/000614.pdf. Accessed 11 May 2016.
de Tayrac R, Mathé M-L, Bader G, Deffieux X, Fazel A, Fernandez H. Infracoccygeal sacropexy or sacrospinous suspension for uterine or vaginal vault prolapse. Int J Gynecol Obstet. 2008;100(2):154–9.
Qatawneh A, Thekrallah F, Bata M, Al-Kazaleh F, Almustafa M, Abu-Kader I. Risk factors of surgical failure following sacrospinous colpopexy for the treatment of uterovaginal prolapse. Arch Gynecol Obstet. 2013;287(6):1159–65.
Roovers J-PWR, van der Vaart CH, van der Bom JG, van Leeuwen JHS, Scholten PC, Heintz APM. A randomised controlled trial comparing abdominal and vaginal prolapse surgery: effects on urogenital function. BJOG Int J Obstet Gynaecol. 2004;111(1):50–6.
Siddiqui NY, Grimes CL, Casiano ER, et al. Mesh sacrocolpopexy compared with native tissue vaginal repair: a systematic review and meta-analysis. Obstet Gynecol. 2015;125(1):44–55.
Barber MD, Maher C. Apical prolapse. Int Urogynecol J. 2013;24(11):1815–33.
Sokol AI, Iglesia CB, Kudish BI, et al. One-year objective and functional outcomes of a randomized clinical trial of vaginal mesh for prolapse. Am J Obstet Gynecol. 2012;206(1):86.e1–9.
Gutman RE, Nosti PA, Sokol AI, et al. Three-year outcomes of vaginal mesh for prolapse: a randomized controlled trial. Obstet Gynecol. 2013;122(4):770–7.
Halaska M, Maxova K, Sottner O, et al. A multicenter, randomized, prospective, controlled study comparing sacrospinous fixation and transvaginal mesh in the treatment of posthysterectomy vaginal vault prolapse. Am J Obstet Gynecol. 2012;207(4):301.e1–7.
Svabik K, Martan A, Masata J, El-Haddad R, Hubka P. Comparison of vaginal mesh repair with sacrospinous vaginal colpopexy in the management of vaginal vault prolapse after hysterectomy in patients with levator ani avulsion: a randomized controlled trial. Ultrasound Obstet Gynecol. 2014;43(4):365–71.
Brandão Dos Reis, da Silveira S, Haddad JM, et al. Multicenter, randomized trial comparing native vaginal tissue repair and synthetic mesh repair for genital prolapse surgical treatment. Int Urogynecol J. 2015;26(3):335–42.
Barber MD, Brubaker L, Nygaard I, et al. Defining success after surgery for pelvic organ prolapse. Obstet Gynecol. 2009;114(3):600–9.
American Urological Association. Choosing Wisely: ten things physicians and patients should question. 2016.http://www.choosingwisely.org/societies/american-urological-association/. Accessed 26 Μay 2016.
Whiteside JL, Weber AM, Meyn LA, Walters MD. Risk factors for prolapse recurrence after vaginal repair. Am J Obstet Gynecol. 2004;191(5):1533–8.
Wang AC, Lee LY, Lin CT, Chen JR. A histologic and immunohistochemical analysis of defective vaginal healing after continence taping procedures: a prospective case-controlled pilot study. Am J Obstet Gynecol. 2004;191(6):1868–74.
Achtari C, Hiscock R, O’Reilly BA, Schierlitz L, Dwyer PL. Risk factors for mesh erosion after transvaginal surgery using polypropylene (Atrium) or composite polypropylene/polyglactin 910 (Vypro II) mesh. Int Urogynecol J Pelvic Floor Dysfunct. 2005;16(5):389–94.
Acknowledgments
No funding or sponsorship was received for this study or publication of this article.
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval for the version to be published.
Disclosures
S. Kontogiannis, E. Goulimi, and K. Giannitsas have nothing to disclose.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not involve any new studies of human or animal subjects performed by any of the authors.
Open Access
This article is distributed under the terms of the Creative Commons Attribution-NonCommercial 4.0 International License (http://creativecommons.org/licenses/by-nc/4.0/), which permits any noncommercial use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced content
To view enhanced content for this article go to http://www.medengine.com/Redeem/8E07F06048A86CAF.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by/4.0), which permits use, duplication, adaptation, distribution, and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made.
About this article
Cite this article
Kontogiannis, S., Goulimi, E. & Giannitsas, K. Reasons for and Against Use of Non-absorbable, Synthetic Mesh During Pelvic Organ Prolapse Repair, According to the Prolapsed Compartment. Adv Ther 33, 2139–2149 (2016). https://doi.org/10.1007/s12325-016-0425-3
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-016-0425-3