Abstract
Introduction
High-dose intravenous esomeprazole is the only approved pharmacological treatment for the prevention of peptic ulcer rebleeding (currently approved in over 100 countries worldwide), but has not yet been approved in China. This study aimed to evaluate a high-dose esomeprazole intravenous regimen vs. an active control (cimetidine) for the prevention of rebleeding in Chinese patients with a high risk of peptic ulcer rebleeding who had undergone primary endoscopic hemostatic treatment.
Methods
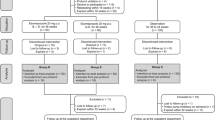
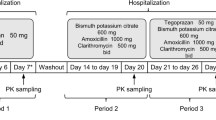
This was a parallel-group study conducted at 20 centers in China. The study comprised a randomized, double-blind, intravenous treatment phase of 72 h in which 215 patients received either high-dose esomeprazole (80 mg + 8 mg/h) or cimetidine (200 mg + 60 mg/h), followed by an open-label oral treatment phase in which all patients received esomeprazole 40 mg tablets once daily for 27 days. The primary outcome was the rate of clinically significant rebleeding within the first 72 h after initial endoscopic hemostatic therapy. Secondary outcomes included the rates of clinically significant rebleeding within 7 and 30 days; proportions of patients who had endoscopic retreatment and other surgery due to rebleeding; and number of blood units transfused.
Results
The rate of clinically significant rebleeding within 72 h was low overall (3.3%) and numerically lower in patients treated with esomeprazole compared with cimetidine (0.9% vs. 5.6%). Overall, the results of the secondary outcomes also showed a numerical trend towards superiority of esomeprazole over cimetidine. All treatments were well tolerated.
Conclusion
In this phase 3, multicenter, randomized trial conducted in China, esomeprazole showed a numerical trend towards superior clinical benefit over cimetidine in the prevention of rebleeding in patients who had successfully undergone initial hemostatic therapy of a bleeding peptic ulcer, with a similar safety and tolerability profile. These findings suggest that esomeprazole may be an alternative treatment option to cimetidine for this indication in China.
Funding
AstraZeneca.
Trial registration
ClinicalTrials.gov identifier, NCT01757275.


Similar content being viewed by others
References
Sung J. Current management of peptic ulcer bleeding. Nat Clin Pract Gastroenterol Hepatol. 2006;3(1):24–32.
Lau JY, Sung J, Hill C, Henderson C, Howden CW, Metz DC. Systematic review of the epidemiology of complicated peptic ulcer disease: incidence, recurrence, risk factors and mortality. Digestion. 2011;84(2):102–13.
Barkun AN, Bardou M, Kuipers EJ, et al. International consensus recommendations on the management of patients with nonvariceal upper gastrointestinal bleeding. Ann Intern Med. 2010;152(2):101–13.
Blatchford O, Davidson LA, Murray WR, Blatchford M, Pell J. Acute upper gastrointestinal haemorrhage in west of Scotland: case ascertainment study. BMJ. 1997;315(7107):510–4.
Leontiadis GI, Sharma VK, Howden CW. Proton pump inhibitor treatment for acute peptic ulcer bleeding. Cochrane Database Syst Rev. 2006;1:CD002094.
van Leerdam ME, Vreeburg EM, Rauws EA, et al. Acute upper GI bleeding: did anything change? Time trend analysis of incidence and outcome of acute upper GI bleeding between 1993/1994 and 2000. Am J Gastroenterol. 2003;98(7):1494–9.
Bai Y, Du YQ, Wang D, et al. Peptic ulcer bleeding in China: a multicenter endoscopic survey of 1006 patients. J Dig Dis. 2014;15(1):5–11.
Kupfer Y, Cappell MS, Tessler S. Acute gastrointestinal bleeding in the intensive care unit. The intensivist’s perspective. Gastroenterol Clin North Am. 2000;29(2):275–307.
Rockall TA, Logan RF, Devlin HB, Northfield TC. Risk assessment after acute upper gastrointestinal haemorrhage. Gut. 1996;38(3):316–21.
Green FW Jr, Kaplan MM, Curtis LE, Levine PH. Effect of acid and pepsin on blood coagulation and platelet aggregation. A possible contributor prolonged gastroduodenal mucosal hemorrhage. Gastroenterology. 1978;74(1):38–43.
Patchett SE, Enright H, Afdhal N, O’Connell W, O’Donoghue DP. Clot lysis by gastric juice: an in vitro study. Gut. 1989;30(12):1704–7.
Li Y, Sha W, Nie Y, et al. Effect of intragastric pH on control of peptic ulcer bleeding. J Gastroenterol Hepatol. 2000;15(2):148–54.
Lau JY, Sung JJ, Lee KK, et al. Effect of intravenous omeprazole on recurrent bleeding after endoscopic treatment of bleeding peptic ulcers. N Engl J Med. 2000;343(5):310–6.
Khuroo MS, Yattoo GN, Javid G, et al. A comparison of omeprazole and placebo for bleeding peptic ulcer. N Engl J Med. 1997;336(15):1054–8.
Sung JJ, Barkun A, Kuipers EJ, et al. Intravenous esomeprazole for prevention of recurrent peptic ulcer bleeding: a randomized trial. Ann Intern Med. 2009;150(7):455–64.
Liu N, Liu L, Zhang H, et al. Effect of intravenous proton pump inhibitor regimens and timing of endoscopy on clinical outcomes of peptic ulcer bleeding. J Gastroenterol Hepatol. 2012;27(9):1473–9.
Forrest JA, Finlayson ND, Shearman DJ. Endoscopy in gastrointestinal bleeding. Lancet. 1974;2(7877):394–7.
ClinicalTrials.gov. High-dose esomeprazole sodium for prevention of rebleeding after successful endoscopic therapy of a bleeding peptic ulcer. Available from: https://clinicaltrials.gov/show/NCT01757275. Accessed 13 Oct 2015.
Leontiadis GI, Sharma VK, Howden CW. Systematic review and meta-analysis: enhanced efficacy of proton-pump inhibitor therapy for peptic ulcer bleeding in Asia–a post hoc analysis from the Cochrane Collaboration. Aliment Pharmacol Ther. 2005;21(9):1055–61.
Lam SK, Hasan M, Sircus W, Wong J, Ong GB, Prescott RJ. Comparison of maximal acid output and gastrin response to meals in Chinese and Scottish normal and duodenal ulcer subjects. Gut. 1980;21(4):324–8.
Caraco Y, Lagerstrom PO, Wood AJ. Ethnic and genetic determinants of omeprazole disposition and effect. Clin Pharmacol Ther. 1996;60(2):157–67.
Goldstein JA. Clinical relevance of genetic polymorphisms in the human CYP2C subfamily. Br J Clin Pharmacol. 2001;52(4):349–55.
Leontiadis GI, Sharma VK, Howden CW. Proton pump inhibitor therapy for peptic ulcer bleeding: Cochrane collaboration meta-analysis of randomized controlled trials. Mayo Clin Proc. 2007;82(3):286–96.
Lau J, Sung J, Lind T, Persson T, Eklund S. High-dose intravenous proton pump inhibitors for prevention of recurrent peptic ulcer bleeding in Chinese and Western populations: rebleeding is not influenced by ethnicity. Digestive Diseases Week; May 3–6; Chicago, IL, 2014.
Li Z, Zou D, Ma X, et al. Epidemiology of peptic ulcer disease: endoscopic results of the systematic investigation of gastrointestinal disease in China. Am J Gastroenterol. 2010;105:2570–7.
Garcia-Iglesias P, Villoria A, Suarez D, et al. Meta-analysis: predictors of rebleeding after endoscopic treatment for bleeding peptic ulcer. Aliment Pharmacol Ther. 2011;34(8):888–900.
van Herwaarden MA, Samsom M, van Nispen CH, Mulder PG, Smout AJ. The effect of Helicobacter pylori eradication on intragastric pH during dosing with lansoprazole or ranitidine. Aliment Pharmacol Ther. 1999;13(6):731–40.
Sung JJ, Tsoi KK, Ma TK, Yung MY, Lau JY, Chiu PW. Causes of mortality in patients with peptic ulcer bleeding: a prospective cohort study of 10,428 cases. Am J Gastroenterol. 2010;105(1):84–9.
Somberg L, Morris J Jr, Fantus R, et al. Intermittent intravenous pantoprazole and continuous cimetidine infusion: effect on gastric pH control in critically ill patients at risk of developing stress-related mucosal disease. J Trauma. 2008;64(5):1202–10.
McRorie JW, Kirby JA, Miner PB. Histamine2-receptor antagonists: rapid development of tachyphylaxis with repeat dosing. World J Gastrointest Pharmacol Ther. 2014;5(2):57–62.
Fujisawa T, Adachi K, Komazawa Y, et al. Helicobacter pylori infection prevents the occurrence of the tolerance phenomenon of histamine H2 receptor antagonists. Aliment Pharmacol Ther. 2004;20(5):559–65.
Barkun AN, Martel M, Toubouti Y, Rahme E, Bardou M. Endoscopic hemostasis in peptic ulcer bleeding for patients with high-risk lesions: a series of meta-analyses. Gastrointest Endosc. 2009;69(4):786–99.
Acknowledgments
This study was funded by AstraZeneca. The article processing charges for this publication were funded by AstraZeneca Gothenburg, Mölndal, Sweden. Medical writing support was provided by Richard Claes (PhD) from Oxford PharmaGenesis, Oxford, UK, and was funded by AstraZeneca Gothenburg, Mölndal, Sweden. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval to the version to be published. We thank the study participants, the study centers and the clinical teams of the Chinese Peptic Ulcer Bleeding Research Group, whose principal investigators are as follows: Zhao-Shen Li, Changhai Hospital, Shanghai; Min-Hu Chen, First Affiliated Hospital of Sun Yat-Sen University, Guangzhou; Dong-Feng Chen, The Third Affiliated Hospital of the Third Military Medical University of PLA, Chongqing; Jiang Bo, Nanfang Hospital, Guangzhou; Feng Ji, The First Affiliated Hospital of Medicine School of Zhejiang University, Hangzhou; Wei-Hong Sha, Guangdong General Hospital, Guangzhou; You-Xiang Chen, The First Affiliated Hospital of Nanchang University, Nanchang; Xiao-Hua Hou, Union Hospital of Tongji Medical College, Huazhong University of Science and Technology, Wuhan; De-An Tian, Tongji Hospital of Tongji Medical College, Huazhong University of Science and Technology, Wuhan; Yong-Dong Wu, Beijing Friendship Hospital, Beijing; Lun-Gen Lu, Shanghai First People’s Hospital, Shanghai; Rong-Quan Wang, The First Affiliated Hospital of the Third Military Medical University of PLA, Chongqing; Yao-Zong Yuan, Shanghai Ruijin Hospital, Shanghai; Rui-Hua Shi, Jangsu Province People’s Hospital, Jiangsu General Hospital, Nanjing; Ji-Yong Liu, Shandong Province Hospital, Jinan; Yi-You Zou, Xiangya Hospital Central South University, Changsha; Shou-Rong Shen, The Third Xiangya Hospital of Central South University, Changsha; Kai-Chun Wu, Xijing Hospital, Xian; Xiao-Ping Zou, Nanjing Drum Tower Hospital, Nanjing; Bing-Rong Liu, The Second Hospital of Harbin Medical University, Harbin.
Disclosures
Yu Bai is supported by the 2014 Shanghai Rising-Star Program (A type, No. 14QA1404800) and Outstanding Young Scholars Fund of the Second Military Medical University, Shanghai. Huifang Chen is an employee of AstraZeneca. Stefan Eklund is an employee of AstraZeneca. Dong-Feng Chen, Rong-Quan Wang, You-Xiang Chen, Rui-Hua Shi, De-An Tian, and Zhao-Shen Li have no financial relationships to declare.
Compliance with ethics guidelines
All participants provided written informed consent. The study protocol was approved by the Shanghai Changhai Hospital Ethics Committee and the appropriate ethics committees for each center before the study began. The study was conducted in accordance with the Declaration of Helsinki, International Conference on Harmonization and Good Clinical Practice guidelines.
Author information
Authors and Affiliations
Corresponding author
Additional information
Y. Bai, D.-F. Chen, and R.-Q. Wang are co-first authors of this article.
On behalf of the Chinese Peptic Ulcer Bleeding Research Group.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Bai, Y., Chen, DF., Wang, RQ. et al. Intravenous Esomeprazole for Prevention of Peptic Ulcer Rebleeding: A Randomized Trial in Chinese Patients. Adv Ther 32, 1160–1176 (2015). https://doi.org/10.1007/s12325-015-0265-6
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-015-0265-6