Abstract
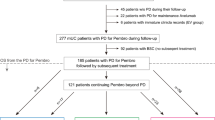
The purpose of this clinical trial was to evaluate the efficacy of 2-year consolidation therapy using nilotinib (NIL) for achieving a molecular response (MR4.5, BCR-ABL1IS ≤ 0.0032% on the International Scale) in patients with chronic myeloid leukemia in the chronic phase (CML-CP) who had achieved a major molecular response (MMR, BCR-ABL1IS ≤ 0.1%) with imatinib (IM). We recruited 76 Japanese patients for this trial. Nilotinib 300 mg, twice daily, was administered for 2 years, and 74 patients were evaluated in the study. The median age was 55.0 years. The median duration of IM treatment was 69.0 months. All patients showed MMR at the time of entry into the study; the median time to MMR on IM therapy was 20.4 months. The proportion of patients who achieved MR4.5 increased over time. The rates of MR4.5 in the 74 evaluable patients were 27.0% [90% confidence interval (CI) (18.7–36.8%)] and 44.6% [90% CI (34.7–54.8%)] at 12 and 24 months, respectively. The frequency of ABCG2 421C/A + A/A was an independent predictive biomarker for achieving a 24-month MR4.5. Switching to NIL led to safer, deeper molecular responses in patients with MMR on long-term IM therapy for future treatment-free remission.

Similar content being viewed by others
References
Kantarjian HM, Hochhaus A, Saglio G, De Souza C, Flinn IW, Stenke L, et al. Nilotinib versus imatinib for the treatment of patients with newly diagnosed chronic phase, Philadelphia chromosome-positive, chronic myeloid leukaemia: 24-month minimum follow-up of the phase 3 randomised ENESTnd trial. Lancet Oncol. 2011;12:841–51.
Larson RA, Hochhaus A, Hughes TP, Clark RE, Etienne G, Kim DW, et al. Nilotinib vs imatinib in patients with newly diagnosed Philadelphia chromosome-positive chronic myeloid leukemia in chronic phase: ENESTnd 3-year follow-up. Leukemia. 2012;26:2197–203.
Hochhaus A, Saglio G, Hughes TP, Larson RA, Kim DW, Issaragrisil S, et al. Long-term benefits and risks of frontline nilotinib vs imatinib for chronic myeloid leukemia in chronic phase: 5-year update of the randomized ENESTnd trial. Leukemia. 2016;30:1044–54.
Hughes TP, Lipton JH, Spector N, Cervantes F, Pasquini R, Clementino NC, et al. Deep molecular responses achieved in patients with CML-CP who are switched to nilotinib after long-term imatinib. Blood. 2014;124:729–36.
Hughes TP, Ross DM. Moving treatment-free remission into mainstream clinical practice in CML. Blood. 2016;128:17–23.
Dulucq S, Mahon FX. Deep molecular responses for treatment-free remission in chronic myeloid leukemia. Cancer Med. 2016;5:2398–411.
Rea D, Cayuela JM. Treatment-free remission in patients with chronic myeloid leukemia. Int J Hematol. 2017. https://doi.org/10.1007/s12185-017-2295-0. (epub ahead of print).
Mahon FX, Rea D, Guilhot J, Guilhot F, Huguet F, Nicolini F, et al. Discontinuation of imatinib in patients with chronic myeloid leukaemia who have maintained complete molecular remission for at least 2 years: the prospective, multicentre Stop Imatinib (STIM) trial. Lancet Oncol. 2010;11:1029–35.
Ross DM, Branford S, Seymour JF, Schwarer AP, Arthur C, Yeung DT, et al. Safety and efficacy of imatinib cessation for CML patients with stable undetectable minimal residual disease: results from the TWISTER study. Blood. 2013;122:515–22.
Rousselot P, Charbonnier A, Cony-Makhoul P, Agape P, Nicolini FE, Varet B, et al. Loss of major molecular response as a trigger for restarting tyrosine kinase inhibitor therapy in patients with chronic-phase chronic myelogenous leukemia who have stopped imatinib after durable undetectable disease. J Clin Oncol. 2014;32:424–30.
Takahashi N, Tauchi T, Kitamura K, Miyamura K, Saburi Y, Hatta Y, et al. Deeper molecular response is a predictive factor for treatment-free remission after imatinib discontinuation in patients with chronic phase chronic myeloid leukemia: the JALSG-STIM213 study. Int J Hematol. 2018;107:185–193.
Miura M, Takahashi N, Sawada K. High-performance liquid chromatography with solid-phase extraction for the quantitative determination of nilotinib in human plasma. Biomed Chromatogr. 2010;24:789–93.
Miura M, Takahashi N. Routine therapeutic drug monitoring of tyrosine kinase inhibitors by HPLC-UV or LC-MS/MS methods. Drug Metab Pharmacokinet. 2016;31:12–20.
Fukuen S, Fukuda T, Maune H, Ikenaga Y, Yamamoto I, Inaba T, et al. Novel detection assay by PCR-RFLP and frequency of the CYP3A5 SNPs, CYP3A5*3 and *6, in a Japanese population. Pharmacogenetics. 2002;12:331–4.
Itoda M, Saito Y, Maekawa K, Hichiya H, Komamura K, Kamakura S, et al. Seven novel single nucleotide polymorphisms in the human SLC22A1 gene encoding organic cation transporter 1 (OCT1). Drug Metab Pharmacokinet. 2004;19:308–12.
Cascorbi I, Gerloff T, Johne A, Meisel C, Hoffmeyer S, Schwab M, et al. Frequency of single nucleotide polymorphisms in the P-glycoprotein drug transporter MDR1 gene in white subjects. Clin Pharmacol Ther. 2001;69:169–74.
Kobayashi D, Ieiri I, Hirota T, Takane H, Maegawa S, Kigawa J, et al. Functional assessment of ABCG2 (BCRP) gene polymorphisms to protein expression in human placenta. Drug Metab Dispos. 2005;33:94–101.
Miura M, Kagaya H, Satoh S, Inoue K, Saito M, Habuchi T, et al. Influence of drug transporters and UGT polymorphisms on pharmacokinetics of phenolic glucuronide metabolite of mycophenolic acid in Japanese renal transplant recipients. Ther Drug Monit. 2008;30:559–64.
Girard H, Villeneuve L, Court MH, Fortier LC, Caron P, Hao Q, et al. The novel UGT1A9 intronic I399 polymorphism appears as a predictor of 7-ethyl-10-hydroxycamptothecin glucuronidation levels in the liver. Drug Metab Dispos. 2006;34:1220–8.
Mailliard RB, Son YI, Redlinger R, Coates PT, Giermasz A, Morel PA, et al. Dendritic cells mediate NK cell help for Th1 and CTL responses: two-signal requirement for the induction of NK cell helper function. J Immunol. 2003;171:2366–73.
Chai-Adisaksopha C, Lam W, Hillis C. Major arterial events in patients with chronic myeloid leukemia treated with tyrosine kinase inhibitors: a meta-analysis. Leuk Lymphoma. 2016;57:1300–10.
Itoda M, Saito Y, Shirao K, Minami H, Ohtsu A, Yoshida T, et al. Eight novel single nucleotide polymorphisms in ABCG2/BCRP in Japanese cancer patients administered irinotacan. Drug Metab Pharmacokinet. 2003;18:212–217.
de Jong FA, Marsh S, Mathijssen RH, King C, Verweij J, Sparreboom A, et al. ABCG2 pharmacogenetics: ethnic differences in allele frequency and assessment of influence on irinotecan disposition. Clin Cancer Res. 2004;10:5889–94.
Takahashi N, Miura M, Scott SA, Kagaya H, Kameoka Y, Tagawa H, et al. Influence of CYP3A5 and drug transporter polymorphisms on imatinib trough concentration and clinical response among patients with chronic phase chronic myeloid leukemia. J Hum Genet. 2010;55:731–7.
Shinohara Y, Takahashi N, Nishiwaki K, Hino M, Kashimura M, Wakita H, et al. A multicenter clinical study evaluating the confirmed complete molecular response rate in imatinib-treated patients with chronic phase chronic myeloid leukemia by using the international scale of real-time quantitative polymerase chain reaction. Haematologica. 2013;98:1407–13.
Mandery K, Glaeser H, Fromm MF. Interaction of innovative small molecule drugs used for cancer therapy with drug transporters. Br J Pharmacol. 2012;165:345–62.
Acknowledgements
This study was supported by research funding from Novartis Pharmaceuticals to N.T. The authors thank all study participants and their families. We also thank Ms. Saori Takahashi and the STAT data center (EPS, Co.) for monitoring the clinical trial, and Dr. Toshihiro Miyamoto, Dr. Yosuke Minami, and Dr. Hidetaka Niitsu for cooperation as members of the data and safety monitoring committee, and all investigators in the STAT study group. The STAT study group (46 institutions and investigators): Akita University Hospital, Dr. Naoto Takahashi; Asahi Hospital, Dr. Masayuki Koizumi; Asahikawa Medical University Hospital, Dr. Motohiro Shindo; Chiba Aoba Municipal Hospital, Dr. Akira Yokota; Chiba Rosai Hospital, Dr. Kenji Kimura; Chiba University Hospital, Dr. Chiaki Nakaseko; Chibaken Saiseikai Narashino Hospital, Dr. Kazuhisa Fujikawa; Dokkyo Medical University Hospital, Dr. Kinuko Mitani; Eiju Hospital, Dr. Masao Hagihara; Fukushima Medical University Hospital, Dr. Hideki Noji; Gumna prefectural Cancer Center, Dr. Tadahiko Igarashi; Gunma University Hospital, Dr. Hiroshi Handa; Hokkaido University Hospital, Dr. Takeshi Kondo; Inoue Memorial Hospital, Dr. Hirotoshi Nakamura; Japanese Red Cross Narita Hospital, Dr. Hisashi Wakita; Jikei University Kashiwa Hospital, Dr. Kaichi Nishiwaki; Jikei University The Third Hospital, Dr. Noriko Usui; Juntendo University Urayasu Hospital, Dr. Masaaki Noguchi; Kameda Medical Center, Dr. Kosei Matsue; Kurokawa Hospital, Dr. Hironao Yokomichi; Mie University Hospital, Dr. Kohshi Ohishi; National Defense Medical College Hospital, Dr. Fumihiko Kimura; Nihonkai General Hospital, Dr. Soichi Saito; Niigata University Hospital, Dr. Masayoshi Masuko; Northern Fukushima Medical Center, Dr. Hideo Kimura; NTT Medical Center Tokyo, Dr. Kensuke Usuki; Odate Municipal General Hospital, Dr. Hitoshi Ogasawara; Okitama Public General Hospital, Dr. Shinji Sato; Omagari Kosei Medical Center, Dr. Mutsuhito Motegi; Saitama Medical Center, Saitama Medical University, Dr. Michihide Tokuhira; Sapporo City General Hospital, Dr. Satoshi Yamamoto; Sapporo Hokuyu Hospital, Dr. Kiyotoshi Imai; Sapporo Medical University Hospital, Dr. Tsutomu Sato; Sendai City Hospital, Dr. Joji Yamamoto; Sendai Medical Center, Dr. Toshiyuki Yokoyama; Shirakawa Kosei General Hosptal, Dr. Masayuki Mita; The Fraternity Memorial Hospital, Dr. Sakae Tanozaki; Tohoku University Hospital, Dr. Hideo Harigae; Tokyo Medical and Dental University Hospital, Dr. Tetsuya Fukuda; Tokyo Medical University Hachioji Medical Center, Dr. Osamu Iwase; Tokyo Metropolitan Cancer and Infectious Diseases Center Komagome Hospital, Dr. Noriko Doki; Tokyo Women’s Medical University Yachiyo Medical Center, Dr. Michihiko Masuda; Yamagata Prefectural Central Hospital, Dr. Eijiro Omoto; Yamagata University Hospital, Dr. Yuichi Kato; Yamanashi University Hospital, Dr. Toru Mitsumori; Yuri General Hospital, Dr. Jun Kuroki.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
N.T received grants from Novartis Pharmaceuticals, during the conduct of the study; grants and personal fees from Novartis Pharmaceuticals, grants and personal fees from Otsuka, grants and personal fees from Pfizer, personal fees from Bristol-Myers Squibb, outside the submitted work; C.N received personal fees from Novartis, grants and personal fees from Bristol-Myers Squibb, grants and personal fees from Pfizer, grants and personal fees from Takeda pharmaceuticals, grants and personal fees from Kyowa Hakko Kirin, grants and personal fees from Otsuka Pharmaceutical, grants and personal fees from Ono Pharmaceutical, grants and personal fees from Chugai Pharmaceutical, grants and personal fees from Asahi Kasei Pharma, grants and personal fees from Shionogi, personal fees from Shire, personal fees from Jannsen, personal fees from Celgene, outside the submitted work; K.N received grants from Zenyaku Kogyo Company, Limited, grants from Chugai Pharmaceutical, grants from Novartis Pharma K.K., grants from Kyowa Hakko Kirin Co, Ltd, grants from Nippon Shinyaku Co, Ltd, outside the submitted work; M.T. received personal fees from Bristol-Myers Squib, personal fees from Pfizer, outside the submitted work; K.M received grants from Kyowa Hakko Kirin Co. Ltd., grants from Chugai Pharmaceutical Co. Ltd., grants from Takeda Pharmaceutical Co. Ltd., grants from Novartis Pharma K. K., personal fees from Kyowa Hakko Kirin Co. Ltd., personal fees from Celgene Co., personal fees from Pfizer Inc., personal fees from Alexion Pharmaceuticals Inc., personal fees from BML Inc., personal fees from Shire Japan K.K., personal fees from Bristol-Myers Squibb K.K., personal fees from Abbvie Inc., personal fees from Mochida Pharmaceutical Co. Ltd., personal fees from Novartis Pharma K. K., personal fees from Takeda Pharmaceutical Co. Ltd., personal fees from Kyowa Hakko Kirin Co. Ltd., personal fees from Ono Pharmaceutical Co. Ltd., personal fees from Nippon Shinyaku Co. Ltd., outside the submitted work. The other authors declare that they have no conflicts of interest.
About this article
Cite this article
Noguchi, S., Nakaseko, C., Nishiwaki, K. et al. Switching to nilotinib is associated with deeper molecular responses in chronic myeloid leukemia chronic phase with major molecular responses to imatinib: STAT1 trial in Japan. Int J Hematol 108, 176–183 (2018). https://doi.org/10.1007/s12185-018-2459-6
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-018-2459-6