Abstract
Knowledge in the field of inherited thrombocytopenias (ITs) has considerably improved over the recent years. In the last 5 years, nine new genes whose mutations are responsible for thrombocytopenia have been identified, and this also led to the recognition of several novel nosographic entities, such as thrombocytopenias deriving from mutations in CYCS, TUBB1, FLNA, ITGA2B/ITGB3, ANKRD26 and ACTN1. The identification of novel molecular alterations causing thrombocytopenia together with improvement of methodologies to study megakaryopoiesis led to considerable advances in understanding pathophysiology of ITs, thus providing the background for proposing new treatments. Thrombopoietin-receptor agonists (TPO-RAs) represent an appealing therapeutic hypothesis for ITs and have been tested in a limited number of patients. In this review, we provide an updated description of pathogenetic mechanisms of thrombocytopenia in the different forms of ITs and recapitulate the current management of these disorders. Moreover, we report the available clinical and preclinical data about the role of TPO-RAs in ITs and discuss the rationale for the use of these molecules in view of pathogenesis of the different forms of thrombocytopenia of genetic origin.
Similar content being viewed by others
Introduction
Knowledge in the field of inherited thrombocytopenias (ITs) has remarkably improved over the recent years. In the last 5 years, nine new genes whose mutations are responsible for thrombocytopenia have been identified [1–9], and this led to the recognition of 6 novel nosographic entities [1]. To date, ITs encompass 20 forms caused by mutations of 21 genes (Table 1). The identification of novel molecular alterations causing IT, together with improvement of methodologies to study megakaryopoiesis of patients or animal models, led to considerable advances in understanding pathophysiology of these disorders, thus providing the background for proposing new treatments. Thrombopoietin-receptor agonists (TPO-RAs) represent an appealing therapeutic hypothesis for ITs. Based on achievements on pathophysiology of the disorder, one of these molecules was successfully tested in MYH9-related disease, one of the less rare forms of IT [10]. The growing knowledge on pathogenesis of thrombocytopenias of genetic origin will drive future experimental work to ascertain if TPO-RAs are effective also in other IT forms.
ITs include syndromic disorders, in which thrombocytopenia can associate with other clinical features, and non-syndromic forms, in which the platelet defect is the only manifestation of the disease. In this review, I will focus on pathogenetic mechanisms underlying thrombocytopenia in the different IT forms. I will then discuss the current treatment of ITs, with emphasis on the available clinical or preclinical data about the role of TPO-RAs. First, I will include a brief overview of the process of platelet biogenesis, which exclusively aims to introduce some physiological mechanisms that are relevant to discussion of pathogenesis. I refer to several recent reviews for detailed treatment of this topic [11–14].
Overview of platelet biogenesis
Platelet biogenesis can be schematically divided in three steps: megakaryocyte (Mk) differentiation from hematopoietic stem cells (HSCs), Mk maturation, and platelet release from mature Mks (Fig. 1). Mks arise from pluripotent HSCs, which develop into burst- and colony-forming precursors, through a differentiation process that implies progressive lineage restriction and loss of proliferative capacity [11]. The thrombopoietin receptor (TPO-R) pathway is essential for maintenance of HSCs compartment and regulates the entire process of platelet biogenesis until platelet release. Mk maturation is characterized by cell polyploidization through endomitosis, a modification of the cell cycle leading to formation of large polylobulated nuclei having up to 256 times the normal chromosome content [12]. Mk maturation also implies intense protein synthesis and considerable increase in cytoplasmic mass with development of platelet-specific structures (such as organelles, granules, membrane integrins, cytoskeletal proteins) and of multiple surface-connected membrane invaginations (demarcation membrane system, DMS) that are regarded as a membrane reservoir for proplatelet extension. The main transcription factors that regulate Mk differentiation and maturation are RUNX1, FLI1, GATA-1, GATA-2, NF-E2, and TAL1/SCL. These factors act synergistically, often bound in complexes, for the coordinated activation and repression of genes required for development of mature Mks [15]. Mk development is also regulated by a complex cross-talk between Mk and cells, cytokines, and extra-cellular matrix (ECM) proteins of the surrounding bone marrow (BM) microenvironments [13]. During maturation, Mks migrate from the bone-proximal microenvironment supporting their proliferation, differentiation and maturation, designated osteoblastic niche, to the BM spaces enriched in sinusoids, the vascular niche [13]. Mk migration is driven by a positive gradient of stromal cell-derived factor 1 (SDF1). The vascular niche is the physiological site of proplatelet formation (PPF). Mature Mks remodel their cytoplasm into multiple, long and branching projections, called proplatelets, with platelet-sized buds at their ends (tips). Proplatelets protrude and are released into the sinusoid lumen. Released proplatelets mature in the circulation and ultimately release individual platelets from their tips [14]. An intermediate stage, designated preplatelet, was recently identified in human blood [13]. PPF is strictly dependent on the reorganization of microtubules and acto-myosin cytoskeleton. Microtubule rearrangement initiates PPF, and proplatelets projections elongate by microtubule polymerization at their free ends and dynein-powered sliding of overlapping microtubules. The acto-myosin cytoskeleton is responsible for repeated bending and branching of the proplatelet projections which multiply the number of free proplatelet ends from which platelets are released [13, 14]. In turn, reorganization of actin cytoskeleton is regulated by membrane glycoproteins (GPs), which transduce signals initiated by Mk adhesion to proteins of BM ECM and link cytoskeleton to plasma membrane. The same cytoskeletal components that regulate PPF are probably involved in proplatelet maturation. A localized activation of the intrinsic apoptotic pathway, initiated by release of cytochrome c from mitochondria, is responsible for triggering PPF [16].
Schematic representation of platelet biogenesis (see text). Mk megakaryocyte, BM bone marrow, HSCs hematopoietic stem cell, MPP multipotent progenitor stem cell, CMP common myeloid progenitor, MEP common megakaryocyte/erythroid progenitor, BFU burst-forming unit, CFU colony forming unit, TPO thrombopoietin, IL interleukin, SCF stem cell factor, SDF1 stromal cell-derived factor 1
Pathogenesis of inherited thrombocytopenias
Table 1 reports a classification of ITs according to the main pathogenetic mechanism underlying thrombocytopenia. Most ITs are caused from defects in platelet biogenesis and only two forms mainly derive from reduced platelet lifespan.
Defective Mk differentiation
These IT forms derive from defective commitment-differentiation of HSC to Mks. The hallmark of these forms is therefore the absence or marked reduction of the number of Mks at examination of BM specimens (amegakaryocytic thrombocytopenias).
In congenital amegakaryocytic thrombocytopenia (CAMT), this hematological picture is caused by absent or reduced activity of TPO-R due to homozygous or compound heterozygous mutations in MPL. The evolution of the disease in trilineage BM failure within the first years of life reflects the non-redundant role of TPO-R pathway in maintenance of the HSC compartment in postnatal life [17]. As a consequence of reduced clearance by Mks and platelets, plasma TPO levels of CAMT patients are exceedingly high [18, 19]. Nonsense or frameshift MPL mutations always cause the complete loss of TPO-R through ablation of the entire intracellular domain. The consequences of missense or splice-site variations are more difficult to predict and could be associated with some residual receptor activity and a less rapid evolution to pancytopenia [20]. The effects of missense and splice-site mutations have been investigated using in vitro cell models. Most of these variations were shown to cause absence or reduced expression of TPO-R on cell surface though different mechanisms, such as defective glycosylation or protein instability [21–23]. Fox and colleagues [23] characterized the p.F104S variation, which, in contrast, resulted in a TPO-R normally expressed on cell surface that was unable to bind TPO via canonical extracellular binding sites.
Patients affected by thrombocytopenia with absent radii (TAR) at birth present a hematological picture similar to that of CAMT. However, their platelet counts ameliorate spontaneously over time to nearly normal levels. TAR originates from defective expression of the RBM8A gene, due to compound heterozygosity for one null allele and one of two hypomorphic SNPs located in regulatory regions of the gene [7]. RBM8A encodes for the Y14 subunit of the exon-junction complex involved in RNA processing, but the link of its reduced expression with TAR phenotype is still unclear. Studies on patient-derived samples suggested that thrombocytopenia arises from defective Mk differentiation and maturation, possibly associated with impaired signaling downstream the TPO-R. HSCs of TAR patients showed reduced commitment and maturation to Mks when cultured in the presence of TPO [24]. After stimulation with TPO, platelets of TAR children failed to phosphorylate JAK2 and activate the other signaling pathways downstream of TPO-R, despite normal expression of both TPO-R and JAK2 [25, 26]. This defect correlated with age and platelet counts, but it is controversial if it could have a pathogenetic role at the level of Mk precursors [25]. As with CAMT, plasma TPO levels of TAR patients are exceedingly high [26].
Amegakaryocytic thrombocytopenia with radio-ulnar synostosis (ATRUS) is a rare IT which often evolves in trilineage BM failure [27]. Genetic analysis of two pedigrees identified one mutation in HoxA11, a member of a family of genes encoding for DNA-binding proteins involved in regulation of early hematopoiesis [28]. No consistent data are currently available about pathophysiology of ATRUS. However, the associated development of aplastic anemia suggests that the defect is at the level of the HSC [29].
Defective Mk maturation
Three ITs derive from defective function of transcription factors with key roles in terminal Mk maturation. Since each of these factors regulates the expression of different genes involved in Mk development, pathogenesis of thrombocytopenia of these forms is complex and involves early as well as late stages of megakaryopoiesis. The common denominator is the evidence, at examination of BM specimens, of Mks with defects in both nuclear and cytoplasmic maturation (dysmegakaryopoiesis) [30–33].
Familial platelet disorder with predisposition to acute myeloid leukemia (FPD-AML) is caused by mutations in RUNX1 encoding for the DNA-binding subunit of the CBF transcription complex [34]. Most mutations result in haploinsufficiency, though some variations are predicted to cause dominant-negative effects [35]. Patients have increased risk to develop hematological malignancies, mainly acute myeloid leukemia and myelodysplastic syndromes, which occur in over 40% of cases [36]. The predisposition to myeloid neoplasms reflects the role of RUNX1 in regulating the equilibrium between HSC proliferation and differentiation in adults [37]. By studies on patients’ Mks, Bluteau and colleagues showed that RUNX1 mutations affect different steps of megakaryopoiesis, including Mk differentiation from HSCs, Mk polyploidization and maturation to GPIbα+ cells, as well as formation and maturation of proplatelets [30]. The defect in polyploidization in vitro paralleled the finding of hypolobulated Mks at examination of BM biopsies, and could be explained by absent downregulation of MYH10, encoding for non-muscle myosin heavy chain (NMMHC)-IIB, whose silencing by RUNX1 is essential for the switch from mitosis to endomitosis in Mks [38]. Reduced transcription of MYH9 and MYL9, encoding for NMMHC-IIA and myosin regulatory light chains, respectively, could instead contribute to defective PPF [30].
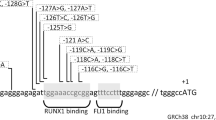
Paris-Trousseau syndrome (TCPT) and Jacobsen syndrome (JBS) are the overlapping disorders deriving from partial deletions in 11q23 [31, 39]. The distinction between TCPT and JBS is based on the severity of the syndrome, which, in turn, reflects the size and breakpoints of the causative deletion [1]. Thrombocytopenia of TCPT/JBS is caused by reduced expression of FLI1, which is included in the deleted region. FLI1 activates transcription of several genes associated with production of mature Mks, including MPL, ITGA2B, GP9, GPIBA, and PF4 [40], and its overexpression in human pluripotent HSCs induces Mk differentiation [41]. Raslova and colleagues showed that the lentivirus-mediated FLI1 overexpression in the CD34+ progenitors of three TCPT children rescued normal in vitro megakaryopoiesis, by increasing the number of mature polyploid Mks and of proplatelet-bearing Mks [40].
Mutations of GATA-1 are responsible for X-Linked thrombocytopenia with thalassemia (XLTT), caused by the p.R216Q change disrupting GATA-1 binding to DNA, and X-Linked dyserythropoietic anemia with thrombocytopenia (XLDT), deriving from missense mutations that impair GATA-1 association with its co-factor FOG1 [32, 33]. In both disorders, thrombocytopenia associate with various degrees of anemia, reflecting the role of GATA-1 in both erythropoieis and megakaryopoiesis [42, 43]. Investigations of GATA-1-deficient mice showed that aberrant Mk maturation is the main mechanism of thrombocytopenia. Mks of these mice exhibited hyperproliferation but defects of both polyploidization and cytoplasmic development associated with reduced transcription of key genes in Mk maturation, including GpIba, GpIbb, Pf4, Mpl, and Nfe2 [42]. Consistently, BM of patients with XLTT or XLDT presented increased number of Mks with marked dysmegakaryopoiesis [32, 33].
Defective PPF from mature Mks
In these ITs, the main mechanism of thrombocytopenia consists in quantitative and/or qualitative defects of PPF, while Mk differentiation and maturation are essentially preserved. In most cases, these ITs derive from mutations in genes for components of the acto-myosin cytoskeleton or alterations of membrane GPs that are predicted to affect cytoskeletal structure or reorganization (Fig. 2). BM examination is not required for diagnosis of these forms: however, in the few analyzed cases, it demonstrated normal or increased number of mature Mks with normal morphology [3, 44, 45].
MYH9-related disease (MYH9-RD) derives from mutations in the gene for the heavy chain of non-muscle myosin IIA [45]. Myosin IIA belongs to a superfamily of cytoskeletal proteins which generate mechanical forces by ATP hydrolysis and sliding along actin filaments. In Mks, myosin IIA was found to negatively regulate PPF. In particular, it mediates the inhibition of PPF initiated by Mk adhesion to type I collagen through GPIaIIa (Fig. 3) [46–48]. As type I collagen is an abundant ECM protein in the osteoblastic niche (Fig. 1), this pathway prevents Mks from premature release of proplatelets in this space. This mechanism can be disrupted in MYH9-RD, as Mks cultured from patients with two different MYH9 mutations extended proplatelets in vitro even in adhesion to type I collagen, suggesting that thrombocytopenia derives from an ectopic PPF resulting in ineffective platelet production [49]. Studies on cell lines transfected with MYH9 mutants suggested that impaired Mk migration in response to SDF1 could contribute to ectopic proplatelet release [50]. Moreover, Mks of MYH9-RD patients exhibited reduced complexity of proplatelet architecture and enlarged tips (Fig. 4), two aspects that could be directly associated with thrombocytopenia and platelet macrocytosis and that are consistent with dysfunction of acto-myosin cytoskeleton during proplatelet development [13]. Studies on a mouse model of MYH9-RD were only in part consistent with findings in human Mks, since they showed morphological abnormalities of PPF resembling those of MYH9-RD patients, but a quantitatively reduced, rather than increased, PPF [51]. However, all investigations on pathogenesis of MYH9-RD thrombocytopenia evidenced alterations of PPF in the face of a preserved Mk differentiation and maturation [49, 51, 52].
The Rho A-Rho associated kinase (ROCK)-myosin regulatory light chains (RLCs)-non muscle myosin II pathway in platelet biogenesis. It has been hypothesized that the interaction of megakaryocytes with fibrillar type I collagen through GPIaIIa results in phosphorylation of the regulatory light chain of non-muscle myosin II that, in turn, inhibits proplatelet formation [46]. Since type I collagen is an abundant extracellular protein in the osteoblastic niche, this mechanism prevents premature proplatelet extension before megakaryocytes reach the marrow space around sinusoids. The inhibitory effect of collagen type I is disrupted in MYH9-RD and it has been suggested that an ectopic proplatelet release contributes to thrombocytopenia of this condition
Proplatelets extended by megakaryocytes of MYH9-RD patients present an altered morphology. Megakaryocytes cultured from circulating progenitors separated from one control subject (Control) and three patients with p.D1424N or p.R1933X mutations of MYH9 (1/A, 2/B, and 3/C) were allowed to extend proplatelets and stained for α-tubulin (green). Hoechst (blue) was used to label the nuclear structures. Proplatelets formed by MYH9-RD megakaryocytes present an obvious defect in branching despite a normal elongation of the individual proplatelet projections. This results in a reduced complexity of proplatelet architecture and in a greatly reduced number of proplatelet tips, the structures that generate nascent platelets (arrows). Another evident abnormality of proplatelet formation of MYH9-RD patients was the larger size of proplatelet tips with respect to controls, which can be directly related to platelet macrocytosis of this disorder. Scale bars 20 μm. Reproduced from Pecci et al. [49], with permission
Kunishima and colleagues [9] reported six Japanese pedigrees with autosomal-dominant (AD) macrothrombocytopenia caused by mutations in ACTN1, the gene for the isoform 1 of α-actinin. ACTN1 is member of a superfamily of proteins involved in the organization of cytoskeleton: in non-muscle cells, ACTN1 stabilizes the filamentous actin network by cross-linking actin filaments in bundles (Fig. 2). All causative mutations were point substitutions located in the actin-binding or calmodulin-like functional domains. Mouse Mks transduced with these ACTN1 variants presented qualitative abnormalities of PPF, such as reduced number of tips with enlarged size, which therefore resembled those observed in MYH9-RD patients or mouse models [9]. Disorganization of actin filaments upon adhesion to fibrinogen or fibronectin was observed in Mks as well as CHO cells transfected with mutant ACTN1. In Mks and platelets, ACTN1 negatively regulates GPIIbIIIa inside-out signaling [9, 53]. Therefore, enhanced activation of GPIIbIIIa signaling could contribute to altered PPF, as with thrombocytopenia caused by ITGA2B-ITGA3 mutations (see below) [9, 54].
Filamin A, encoded by FLNA located on chromosome Xq28, is a ubiquitously expressed cytoskeletal protein. Filamin A functions in Mks and platelets include connection of cytoplasmic tail of GPIbα with F-actin (Fig. 2) and transduction of Syk-mediated signaling [55, 56]. Nurden and colleagues described three female patients with thrombocytopenia caused by monoallelic FLNA mutations. In two subjects with large FLNA deletions, thrombocytopenia associated with periventricular nodular heterotopia, a neurologic disorder due to impaired neuronal migration, while in the third patient macrothrombocytopenia was the only manifestation of a missense mutation [6, 57]. Mks of these subjects showed preserved in vitro development and a quantitative defect in PPF. In addition, mature Mks had ultrastructural abnormalities consistent with reduced cytoskeletal stability [6].
The molecular basis of the classical recessive form of Bernard–Soulier syndrome (BSS) is the absence or severe reduction of the GPIb–IX–V complex in Mks and platelets [58]. These patients have macrothrombocytopenia and severe bleeding tendency caused by loss of GPIb–IX–V receptor functions as well as low platelet count [59]. Several experimental evidences indicated that defective PPF is the mechanism of thrombocytopenia of BSS. GPIbβ-null mice recapitulated the phenotype of human disease. The main alterations of megakaryopoiesis of these mice were a reduced proportion of Mks extending proplatelets and decreased complexity of proplatelet architecture, associated with Mk ultrastructural abnormalities consistent with underdevelopment of DMS and defective reorganization of cytoskeleton and microtubules [60]. Mks differentiated from HSCs of biallelic BSS patients presented no ability to extend proplatelets in vitro, in the face of a preserved differentiation and maturation [61, 62]. The monoallelic variant of BSS caused by heterozygous p.A156V mutation is characterized by an only partial defect of the GPIb–IX–V complex and a less severe degree of thrombocytopenia and platelet macrocytosis than biallelic BSS [63]. Consistent with this milder phenotype, Mks cultured from these patients showed reduced PPF, but the severity of the defect was lower than that observed with biallelic BSS subjects [64]. In both mice and men, the PPF defects were the same in Mks cultured in suspension or upon adhesion to different ECM proteins, suggesting that they were intrinsic to Mks rather than depending on defective GPIb–IX–V/VWF binding [60, 64]. Consistently, in GPIbα-null mice, macrothrombocytopenia could be partially rescued by transduction of the intracellular domain of GPIbα alone. This emphasizes the role in platelet production of this portion of the molecule, which links the acto-myosin cytoskeleton through Filamin A, even in the absence of extracellular ligand binding properties [65].
Five different heterozygous mutations in either ITGA2B or ITGB3 resulting in a constitutive, albeit partial, activation of GPIIbIIIa have been reported as responsible for AD macrothrombocytopenia [4, 54]. Mks, platelets or transfected cell lines expressing these GPIIbIIIa mutants showed spontaneous binding of PAC1 (a monoclonal antibody that binds only the activated receptor) under resting conditions, and constitutive phosphorylation of downstream effectors of GPIIbIIIa signaling, such as FAK and Src [54, 66, 67]. Patients’ Mks, or murine Mks transduced with ITGA2B mutants, showed similar defects of proplatelet architecture and premature PPF [54, 66, 67]. These alterations may be explained by defective cytoskeleton remodeling consequent to constitutive Src/FAK activation [54], while other studies showed that the inappropriate GPIIbIIIa activation caused decreased RhoA activity, which, as with MYH9-related thrombocytopenia, could result in premature PPF [68].
Despite the key role of microtubules in PPF, mutation of a component of the microtubule system was identified in only one family with IT [3]. The p.R318W change in β1-tubulin was predicted to affect microtubule assembly by disrupting interaction between α- and β-tubulin to form heterodimers. Mks of the proband showed normal development, but abnormal morphology of mature forms suggested impaired PPF. Reduced lifespan of platelets with defective microtubules could contribute to thrombocytopenia [3].
Morison and colleagues [2] reported a large family with AD thrombocytopenia caused by a mutation in CYCS increasing the proapoptotic activity of cytochrome c. Increased intrinsic apoptosis in Mks was responsible for premature PPF within BM and consequent ineffective platelet production. Mks showed premature and enhanced in vitro PPF and signs of ectopic platelet release were found at examination of BM biopsy of one patient [2].
Reduced platelet lifespan
Wiskott–Aldrich syndrome (WAS) is a complex disease deriving from mutations in WAS leading to defective expression or activity of its product WASp. X-linked thrombocytopenia (XLT) is a variant with milder phenotype, characterized by thrombocytopenia as the unique or the preponderant clinical feature. WASp levels correlate with disease phenotype [69]. WASp is expressed exclusively in hematopoietic cells and has a key role in actin polymerization and reorganization of actin cytoskeleton. Studies on WASp-null mice and WAS patients demonstrated that defective platelets are cleared at a faster rate by macrophages [70–72]. Anti-platelet autoantibodies could contribute to this process [73]. Investigations on murine models also suggested an ineffective platelet production deriving from premature PPF within BM and impaired SDF1-driven migration of Mks [74]. However, the observation that splenectomy normalizes platelet count in WAS and XLT patients suggests that increased platelet clearance is the preponderant mechanism of thrombocytopenia of these disorders.
Other pathogenetic mechanisms
Macrothrombocytopenia often associated to hemolytic anemia and/or stomatocytosis can be the clinical presentation of sitosterolemia (STSL) [75]. STSL is caused by accumulation in the body of plant sterols as a consequence of mutations in the transporter responsible for their excretion in bile and gut [76]. Macrothrombocytopenia of STSL derives from a direct toxic effect of plant sterols on Mks and platelets [75–77].
Unknown pathogenesis
The genetic defect of two IT forms was discovered recently and very scarce data are available about pathogenesis of thrombocytopenia.
ANKRD26-related thrombocytopenia (ANKRD26-RT) derives from monoallelic mutations in the 5′UTR of ANKRD26 that probably lead to overexpression of this gene during megakaryopoiesis [5]. ANKRD26 is implicated in regulation of adipogenesis by interaction with signal transduction pathways expressed also in Mks [78], but its role in platelet biogenesis is unknown. Examination of patients’ BM biopsies demonstrated marked dysmegakaryopoiesis [79]. A recent study identified deregulation of the ubiquitin–proteasome system in ANKRD26-RT platelets and Mks [80]. The evaluation of a large case series of patients suggested that ANKRD26-RT predisposes to development of hematological malignancies [79].
Gray platelet syndrome (GPS) is characterized by progressive macrothrombocytopenia and severe alpha-granule deficiency. GPS is caused by mutations in NBEAL2, a gene probably implicated in vesicle trafficking [8]. Early studies demonstrated reduced survival of GPS platelets [81] and inability of Mks to mature normally is thought to contribute to reduced platelet count. Amelioration of thrombocytopenia after splenectomy in one patient is consistent with increased platelet clearance. Progression of myelofibrosis and splenomegaly are likely to contribute to the worsening of thrombocytopenia over time [82].
Management of inherited thrombocytopenias
HSC transplantation (HSCT) is the treatment of choice for the most severe forms of ITs that endanger life of patients. For all the other forms, the standard care is essentially based on general measures and platelet transfusions. As the use of transfusions has several limitations, the knowledge that TPO-RAs may be effective in ITs represents an important innovation.
General measures
Prevention of bleeding is a major aspect for the management of ITs. Patients and their family physicians should be instructed to avoid drugs that impair platelet function. These medications should be administered only after a careful assessment of the ratio between risks and benefits. Nonsteroidal anti-inflammatory drugs are well-known inhibitors of platelet aggregation, but other drugs also affect platelet function: some antibiotics, cardiovascular, psychotropic, and oncologic treatments, drugs that affect platelet cAMP, anesthetics, volume expanders, antihistamines, and radiographic contrast agents [83]. Regular dental care and oral hygiene are recommended to prevent gum bleeding and limit the need for invasive dental procedures. Hormonal contraceptives are effective in preventing menorrhagia. However, even in thrombocytopenic subjects, these drugs should be administered only after assessment of the risk of thrombotic complications.
Platelet transfusion
Transfusion of platelet concentrates is highly effective in increasing platelet count, but it exposes patients to the risks of infectious diseases, allergic reactions and alloimmunization that can lead to refractoriness to subsequent platelet transfusions. Thus, platelet transfusion should be used only for severe bleedings that cannot be managed by local measures, such as nasal packing in the case of epistaxis, and, if needed, as prophylaxis before surgery or other major hemostatic stresses. The need for prophylactic platelet transfusion before surgery should be carefully assessed in relation to the type of procedure and patient’s features (platelet count and function, history of bleeding, overall evaluation of hemostasis) in order to avoid unnecessary transfusions. Whenever possible, platelets from HLA-matched donors should be used to prevent or overcome alloimmunization.
A peculiar problem of patients with biallelic BSS, whose platelets may completely lack the GPIb–IX–V complex, is isoimmunization against components of this complex of donor platelets. In this case, it is not possible to find compatible donors and the only chance to restore efficacy of platelet transfusion is immune suppression and/or plasmapheresis to eliminate isoantibodies [84].
Hemopoietic stem cell transplantation
HSCT is the treatment of choice for children with WAS and CAMT. The outcome of HSCT in WAS is related to donor source, age and clinical status of the recipient. A recent multicentre study in 194 patients showed that overall 5-year survival for patients who received a transplant since the year 2000 was 90 %. The 5-year survival was 100 % for subjects transplanted from HLA-matched sibling donors. Age more than 5 years at HSCT correlated with worst outcome for patients transplanted from HLA-matched unrelated donors [85]. A total of 52 CAMT patients treated with HSCT have been reported [17], and in about half of cases a family member was used as donor. Long-term overall survival was about 80 % and most of these patients achieved normal donor hemopoiesis and good quality of life. The HSCT-related mortality was 7.7 % using matched related donors and 27.8 % using unrelated donors [17]. Two twin girls and one 28-year-old woman with biallelic BSS were treated by HSCT [86, 87]. In these patients, the use of HSCT was justified by the severe clinical picture, as all of them had repeated, life-threatening bleeding episodes. All three patients were cured by transplant from HLA-identical siblings.
Gene therapy
Gene therapy is an experimental alternative to HSCT for patients affected by WAS and no HLA-matched donors. Several clinical studies are currently open in Europe and United States for the use of HSCs transduced with WAS by a lentiviral vector [69].
Splenectomy
Splenectomy is a therapeutic option for patients with XLT. In these subjects, splenectomy increases platelet count up to normal levels, but also results in higher incidence of severe infectious episodes [88]. These data indicate that the pros and cons of this treatment should be weighed for individual XLT patients. Splenectomy is effective in increasing platelet count also in WAS patients. However, because of the severe dysfunction of immune system, HSCT is the treatment of choice for this disease [69]. In all the other forms of ITs, splenectomy has no therapeutic role. Several patients with ITs other than WAS/XLT have been splenectomized as a consequence of a wrong diagnosis of immune thrombocytopenia. Transient increases in platelet count have been reported in some individuals, but no long-term benefits.
Other treatments
Desmopressin (1-deamino-8-d-arginine vasopressin, DDAVP) shortened the bleeding time by about 50 % in a few individuals with ITs [89]. This effect could be mediated by multiple mechanisms, including increased release of high molecular weight multimers of VWF, changes in circulating catecholamines, and a direct priming effect on platelets promoting aggregation induced by physiological agonists. Since not all patients respond, a test dose is recommended to identify those who may benefit from receiving DDAVP for future bleeding episodes or to prevent bleeding from minor, invasive procedures. However, this treatment has not yet been validated, and has to be considered as experimental.
Antifibrinolytic agents, such as epsilon aminocaproic or tranexamic acid, are used by local application or systemic administration for prevention or treatment of bleeding episodes. However, no data supporting the effectiveness of these drugs in ITs are available, and this therapy has to be considered as empirical. Some data support the use of activated recombinant factor VII to treat severe bleedings in IT patients who are refractory to platelet transfusions [90].
Role of thrombopoietin-receptor agonists
TPO-RAs could be theoretically useful in IT patients in two clinical contexts. Short-term treatment courses could be used to transiently increase platelet count in preparation for elective surgery or invasive procedures. Moreover, patients at high risk of spontaneous bleeding may benefit from long-term administration. Results obtained so far are promising in that they indicate that TPO-RAs may be effective, but experience in this field is still limited.
In a small clinical trial, 12 consecutive patients with MYH9-RD and platelet counts lower than 50 × 109/L were treated with eltrombopag for 3–6 weeks. Eleven patients responded, and 8 of them achieved major responses (platelet count higher than 100 × 109/L or three times the baseline value). Treatment was well tolerated and bleeding diathesis disappeared in 8 of 10 patients with spontaneous bleeding at baseline [10]. Based on these results, one patient with MYH9-RD and <20 × 109 platelets/L received eltrombopag for preparation to a major surgical procedure, which was successfully performed when her platelet count normalized after 17 days of treatment [91]. Gröpper and colleagues reported one MYH9-RD patient successfully treated with romiplostim. Platelet response and remission of spontaneous bleeding were maintained for 20 months: subsequently, patient’s platelet count returned to baseline levels despite continuous romiplostim administration [92].
These results demonstrate that TPO-RAs are effective in increasing platelet counts in most patients with MYH9-RD. In general, we suggest that TPO-RAs could be effective in all the forms of IT in which an altered PPF is the main mechanism of thrombocytopenia and the in vitro differentiation and maturation of Mks in response to TPO is preserved (Table 1). In these forms, increasing the number of BM Mks could compensate for the reduced efficiency of platelet production. Moreover, the normal or only moderately high levels of baseline serum TPO observed in MYH9-RD [10] are consistent with the fact that Mk production could be increased by further stimulation of TPO-R. Interestingly, in other IT forms deriving from defective PPF, such as monoallelic or biallelic BSS, serum TPO levels similar to those of MYH9-RD were measured (Pecci, unpublished data).
A study published in abstract form investigated the effects of short-term TPO-RAs in WAS/XTL [93]. Two infants with WAS were treated with romiplostim, while two older patients, one with XLT and one with WAS, received eltrombopag. The XLT patient obtained an increase in platelet count and amelioration of bleeding tendency. One WAS infant had transient responses, but the platelet count was maintained over 20–30 × 109/L only in intervals between infectious episodes. The other two WAS patients did not respond to TPO-RAs. Although the effect of TPO-RAs in XLT/WAS deserves further investigations, these results suggest that they could have a role in these forms, especially for XLT patients for whom splenectomy is contraindicated.
In CAMT, the rationale for the use of TPO-RAs is lacking in cases caused by nonsense and frameshift mutations that abrogate the expression of TPO-R, while the effects of TPO-RAs on MPL mutants with single amino acid substitutions have been investigated in transduced cell lines. For most mutations, results of these in vitro studies were poor, consistent with the absent or very scarce expression of these mutants TPO-Rs on cell surface [22, 23, 94]. In contrast, the p.F104S mutation results in a TPO-R unable to bind TPO via the canonical extracellular binding sites, but otherwise normally expressed on cell surface. Intriguingly, in cell lines expressing this mutant, the TPO-R signaling was activated by LGD-4667, a TPO-RA that binds the TPO-R transmembrane domain, but not by agonists targeting the extracellular domain, demonstrating that the signaling defect could be bypassed by use of an alternative binding site [23]. This mutation was identified so far in only one CAMT pedigree, but it is possible that other mutants behave similarly. In summary, in CAMT the use of TPO-RAs as an alternative therapeutic option can be hypothesized only in a minority of patients selected on the basis of molecular characterization of their mutations and in vitro preclinical studies. No studies directly addressed the role of TPO-RAs in TAR. The information obtained so far on disease pathogenesis suggests that TPO-RAs, at least those targeting canonical binding sites, are unlikely to work in TAR patients. These evidences include the exceedingly high endogenous plasma TPO levels of TAR subjects [26], the defective signaling downstream TPO-R observed in platelets [25, 26], and the failure to improve the in vitro differentiation of HSCs from one TAR patient to Mks by increasing doses of TPO [24]. Finally, no data are available to predict the effectiveness of TPO-RAs in patients with ITs deriving from defective Mk maturation.
In some IT forms, the use of TPO-RAs could be limited by the fact that, because of concomitant defects in platelet function, the increase in platelet count could not result in significant improvement of hemostasis. In particular, in patients with biallelic BSS, the lack of GPIb–IX–V in platelets is probably more relevant than thrombocytopenia by itself in pathogenesis of bleeding [58]. In fact, bleeding diathesis is always much more severe than expected from platelet counts, and its severity varies among patients without any apparent association with platelet counts [59]. Platelet functional defects with probable clinical impact have been reported in other ITs, including FDP-AML, WAS/XLT, and thrombocytopenias deriving from ITGA2B/ITGB3 or FLNA mutations, but the relative contribution of these defects to bleeding tendency is still to be assessed [4, 36, 57, 69, 95].
As regards safety issues of TPO-RAs, some aspects related to the specific features of some forms of ITs deserve comments. In acquired thrombocytopenias, TPO-RAs could increase the risk of thromboembolic events (TEE) [96]. TEE have been reported in patients with ITs [97, 98], and some authors hypothesized that the increased platelet size of some IT forms could favor these complications [99, 100]. Thus, increased production of large platelets by TPO-RAs administration could particularly predispose to thrombosis. In the 14 short-term courses of TPO-RAs given to patients with MYH9-RD (the form of IT with the largest platelet size), no TEE occurred [10, 91, 92]. However, in all the IT forms, a careful evaluation of the balance between benefits and risk of thrombosis in individual patients is strongly recommended before TPO-RAs administration. In two clinical trials of romiplostim in myelodysplastic syndromes, some patients experienced increases in peripheral blood blasts and increased risk of transformation to acute leukemia was suggested [101, 102]. FPD-AML and ANKR26-RT predispose to myeloid malignancies. Therefore, the risk of favoring leukemic transformation by TPO-RAs administration should be considered in these patients. Finally, Léon and colleagues [103] found that thrombocytopenic Myh9−/− mice developed significant BM fibrosis after romiplostim treatment. On this basis, myelofibrosis should be regarded as a potential adverse effect of long-term administration of TPO-RAs in MYH9-RD patients.
References
Balduini CL, Savoia A. Genetics of familial forms of thrombocytopenia. Hum Genet. 2012;131:1821–32.
Morison IM, Cramer Bordé EM, Cheesman EJ, Cheong PL, Holyoake AJ, Fichelson S, et al. A mutation of human cytochrome c enhances the intrinsic apoptotic pathway but causes only thrombocytopenia. Nat Genet. 2008;40:387–9.
Kunishima S, Kobayashi R, Itoh TJ, Hamaguchi M, Saito H. Mutation of the beta1-tubulin gene associated with congenital macrothrombocytopenia affecting microtubule assembly. Blood. 2009;113:458–61.
Nurden AT, Pillois X, Fiore M, Heilig R, Nurden P. Glanzmann thrombasthenia-like syndromes associated with macrothrombocytopenias and mutations in the genes encoding the αIIbβ3 integrin. Semin Thromb Hemost. 2011;37:698–706.
Pippucci T, Savoia A, Perrotta S, Pujol-Moix N, Noris P, Castegnaro G, et al. Mutations in the 5′ UTR of ANKRD26, the ankirin repeat domain 26 gene, cause an autosomal-dominant form of inherited thrombocytopenia, THC2. Am J Hum Genet. 2011;88:115–20.
Nurden P, Debili N, Coupry I, Bryckaert M, Youlyouz-Marfak I, Solé G, et al. Thrombocytopenia resulting from mutations in filamin A can be expressed as an isolated syndrome. Blood. 2011;118:5928–37.
Albers CA, Paul DS, Schulze H, Freson K, Stephens JC, Smethurst PA, et al. Compound inheritance of a low-frequency regulatory SNP and a rare null mutation in exon-junction complex subunit RBM8A causes TAR syndrome. Nat Genet. 2012;44:435–9.
Albers CA, Cvejic A, Favier R, Bouwmans EE, Alessi MC, Bertone P, et al. Exome sequencing identifies NBEAL2 as the causative gene for gray platelet syndrome. Nat Genet. 2011;43:735–7.
Kunishima S, Okuno Y, Yoshida K, Shiraishi Y, Sanada M, Muramatsu H, et al. ACTN1 mutations cause congenital macrothrombocytopenia. Am J Hum Genet. 2013;92:431–8.
Pecci A, Gresele P, Klersy C, Savoia A, Noris P, Fierro T, et al. Eltrombopag for the treatment of the inherited thrombocytopenia deriving from MYH9 mutations. Blood. 2010;116:5832–7.
Chang Y, Bluteau D, Debili N, Vainchenker W. From hematopoietic stem cells to platelets. J Thromb Haemost. 2007;5(Suppl 1):318–27.
Bluteau D, Lordier L, Di Stefano A, Chang Y, Raslova H, Debili N, et al. Regulation of megakaryocyte maturation and platelet formation. J Thromb Haemost. 2009;7(Suppl 1):227–34.
Thon JN, Italiano JE. Platelets: production, morphology and ultrastructure. Handb Exp Pharmacol. 2012;210:3–22.
Thon JN, Italiano JE Jr. Does size matter in platelet production? Blood. 2012;120:1552–61.
Tijssen MR, Cvejic A, Joshi A, Hannah RL, Ferreira R, Forrai A, et al. Genome-wide analysis of simultaneous GATA1/2, RUNX1, FLI1, and SCL binding in megakaryocytes identifies hematopoietic regulators. Dev Cell. 2011;20:597–609.
De Botton S, Sabri S, Daugas E, Zermati Y, Guidotti JE, Hermine O, et al. Platelet formation is the consequence of caspase activation within megakaryocytes. Blood. 2002;100:1310–7.
Ballmaier M, Germeshausen M. Congenital amegakaryocytic thrombocytopenia: clinical presentation, diagnosis, and treatment. Semin Thromb Hemost. 2011;37:673–81.
Ballmaier M, Germeshausen M, Schulze H, Cherkaoui K, Lang S, Gaudig A, et al. c-mpl mutations are the cause of congenital amegakaryocytic thrombocytopenia. Blood. 2001;97:139–46.
Savoia A, Dufour C, Locatelli F, Noris P, Ambaglio C, Rosti V, et al. Congenital amegakaryocytic thrombocytopenia: clinical and biological consequences of five novel mutations. Haematologica. 2007;92:1186–93.
Germeshausen M, Ballmaier M, Welte K. MPL mutations in 23 patients suffering from congenital amegakaryocytic thrombocytopenia: the type of mutation predicts the course of the disease. Hum Mutat. 2006;27:296.
Gandhi MJ, Pendergrass TW, Cummings CC, Ihara K, Blau CA, Drachman JG. Congenital amegakaryocytic thrombocytopenia in three siblings: molecular analysis of atypical clinical presentation. Exp Hematol. 2005;33:1215–21.
Fox NE, Chen R, Hitchcock I, Keates-Baleeiro J, Frangoul H, Geddis AE. Compound heterozygous c-Mpl mutations in a child with congenital amegakaryocytic thrombocytopenia: functional characterization and a review of the literature. Exp Hematol. 2009;37:495–503.
Fox NE, Lim J, Chen R, Geddis AE. F104S c-Mpl responds to a transmembrane domain-binding thrombopoietin receptor agonist: proof of concept that selected receptor mutations in congenital amegakaryocytic thrombocytopenia can be stimulated with alternative thrombopoietic agents. Exp Hematol. 2010;38:384–91.
Letestu R, Vitrat N, Massé A, Le Couedic JP, Lazar V, Rameau P, et al. Existence of a differentiation blockage at the stage of a megakaryocyte precursor in the thrombocytopenia and absent radii (TAR) syndrome. Blood. 2000;95:1633–41.
Fiedler J, Strauss G, Wannack M, Schwiebert S, Seidel K, Henning K, et al. Two patterns of thrombopoietin signaling suggest no coupling between platelet production and thrombopoietin reactivity in thrombocytopenia-absent radii syndrome. Haematologica. 2012;97:73–81.
Ballmaier M, Schulze H, Strauss G, Cherkaoui K, Wittner N, Lynen S, et al. Thrombopoietin in patients with congenital thrombocytopenia and absent radii: elevated serum levels, normal receptor expression, but defective reactivity to thrombopoietin. Blood. 1997;90:612–9.
Thompson AA, Woodruff K, Feig SA, Nguyen LT, Schanen NC. Congenital thrombocytopenia and radio-ulnar synostosis: a new familial syndrome. Br J Haematol. 2001;113:866–70.
Thompson AA, Nguyen LT. Amegakaryocytic thrombocytopenia and radio-ulnar synostosis are associated with HOXA11 mutation. Nat Genet. 2000;26:397–8.
Geddis AE, Kaushansky K. Inherited thrombocytopenias: toward a molecular understanding of disorders of platelet production. Curr Opin Pediatr. 2004;16:15–22.
Bluteau D, Glembotsky AC, Raimbault A, Balayn N, Gilles L, Rameau P, et al. Dysmegakaryopoiesis of FPD/AML pedigrees with constitutional RUNX1 mutations is linked to myosin II deregulated expression. Blood. 2012;120:2708–18.
Favier R, Jondeau K, Boutard P, Grossfeld P, Reinert P, Jones C, et al. Paris–Trousseau syndrome: clinical, hematological, molecular data of ten new cases. Thromb Haemost. 2003;90:893–7.
Balduini CL, Pecci A, Loffredo G, Izzo P, Noris P, Grosso M, et al. Effects of the R216Q mutation of GATA-1 on erythropoiesis and megakaryocytopoiesis. Thromb Haemost. 2004;91:129–40.
Nichols KE, Crispino JD, Poncz M, White JG, Orkin SH, Maris JM, et al. Familial dyserythropoietic anaemia and thrombocytopenia due to an inherited mutation in GATA1. Nat Genet. 2000;24:266–70.
Song WJ, Sullivan MG, Legare RD, Hutchings S, Tan X, Kufrin D, et al. Haploinsufficiency of CBFA2 causes familial thrombocytopenia with propensity to develop acute myelogenous leukaemia. Nat Genet. 1999;23:166–75.
Matheny CJ, Speck ME, Cushing PR, Zhou Y, Corpora T, Regan M, et al. Disease mutations in RUNX1 and RUNX2 create nonfunctional, dominant-negative, or hypomorphic alleles. EMBO J. 2007;26:1163–75.
Liew E, Owen C. Familial myelodysplastic syndromes: a review of the literature. Haematologica. 2011;96:1536–42.
Link KA, Chou FS, Mulloy JC. Core binding factor at the crossroads: determining the fate of the HSC. J Cell Physiol. 2010;222:50–6.
Lordier L, Bluteau D, Jalil A, Legrand C, Pan J, Rameau P, et al. RUNX1-induced silencing of non-muscle myosin heavy chain IIB contributes to megakaryocyte polyploidization. Nat Commun. 2012;3:717.
Mattina T, Perrotta CS, Grossfeld P. Jacobsen syndrome. Orphanet J Rare Dis. 2009;4:9.
Raslova H, Komura E, Le Couédic JP, Larbret F, Debili N, Feunteun J, et al. FLI1 monoallelic expression combined with its hemizygous loss underlies Paris–Trousseau/Jacobsen thrombopenia. J Clin Invest. 2004;114:77–84.
Athanasiou M, Mavrothalassitis G, Sun-Hoffman L, Blair DG. FLI-1 is a suppressor of erythroid differentiation in human hematopoietic cells. Leukemia. 2000;14:439–45.
Vyas P, Ault K, Jackson CW, Orkin SH, Shivdasani RA. Consequences of GATA-1 deficiency in megakaryocytes and platelets. Blood. 1999;93:2867–75.
Fujiwara Y, Browne CP, Cunniff K, Goff SC, Orkin SH. Arrested development of embryonic red cell precursors in mouse embryos lacking transcription factor GATA-1. Proc Natl Acad Sci USA. 1996;93:12355–8.
Tomer A, Scharf RE, McMillan R, Ruggeri ZM, Harker LA. Bernard–Soulier syndrome: quantitative characterization of megakaryocytes and platelets by flow cytometric and platelet kinetic measurements. Eur J Haematol. 1994;52:193–200.
Balduini CL, Pecci A, Savoia A. Recent advances in the understanding and management of MYH9-related inherited thrombocytopenias. Br J Haematol. 2011;154:161–74.
Chen Z, Naveiras O, Balduini A, Mammoto A, Conti MA, Adelstein RS, et al. The May–Hegglin anomaly gene MYH9 is a negative regulator of platelet biogenesis modulated by the Rho-ROCK pathway. Blood. 2007;110:171–9.
Chang Y, Auradé F, Larbret F, et al. Proplatelet formation is regulated by the Rho/ROCK pathway. Blood. 2007;109:4229–36.
Balduini A, Pallotta I, Malara A, Lova P, Pecci A, Viarengo G, et al. Adhesive receptors, extracellular proteins and myosin IIA orchestrate proplatelet formation by human megakaryocytes. J Thromb Haemost. 2008;6:1900–7.
Pecci A, Malara A, Badalucco S, Bozzi V, Torti M, Balduini CL, et al. Megakaryocytes of patients with MYH9-related thrombocytopenia present an altered proplatelet formation. Thromb Haemost. 2009;102:90–6.
Pecci A, Bozzi V, Panza E, Barozzi S, Gruppi C, Seri M, et al. Mutations responsible for MYH9-related thrombocytopenia impair SDF-1-driven migration of megakaryoblastic cells. Thromb Haemost. 2011;106:693–704.
Zhang Y, Conti MA, Malide D, Dong F, Wang A, Shmist YA. Mouse models of MYH9-related disease: mutations in nonmuscle myosin II-A. Blood. 2012;119:238–50.
Kunishima S, Hamaguchi M, Saito H. Differential expression of wild-type and mutant NMMHC-IIA polypeptides in blood cells suggests cell-specific regulation mechanisms in MYH9 disorders. Blood. 2008;111:3015–23.
Tadokoro S, Nakazawa T, Kamae T, Kiyomizu K, Kashiwagi H, Honda S, et al. A potential role for α-actinin in inside-out αIIbβ3 signaling. Blood. 2011;117:250–8.
Bury L, Malara A, Gresele P, Balduini A. Outside-in signalling generated by a constitutively activated integrin αIIbβ3 impairs proplatelet formation in human megakaryocytes. PLoS ONE. 2012;7:e34449.
Nakamura F, Pudas R, Heikkinen O, Permi P, Kilpeläinen I, Munday AD, et al. The structure of the GPIb-filamin A complex. Blood. 2006;107:1925–32.
Falet H, Pollitt AY, Begonja AJ, Weber SE, Duerschmied D, Wagner DD, et al. A novel interaction between FlnA and Syk regulates platelet ITAM-mediated receptor signaling and function. J Exp Med. 2010;207:1967–79.
Berrou E, Adam F, Lebret M, Fergelot P, Kauskot A, Coupry I, et al. Heterogeneity of platelet functional alterations in patients with filamin A mutations. Arterioscler Thromb Vasc Biol. 2013;33:11–8.
Berndt MC, Andrews RK. Bernard–Soulier syndrome. Haematologica. 2011;96:355–9.
Savoia A, Pastore A, De Rocco D, Civaschi E, Di Stazio M, Bottega R, et al. Clinical and genetic aspects of Bernard–Soulier syndrome: searching for genotype/phenotype correlations. Haematologica. 2011;96:417–23.
Strassel C, Eckly A, Léon C, Petitjean C, Freund M, Cazenave JP, et al. Intrinsic impaired proplatelet formation and microtubule coil assembly of megakaryocytes in a mouse model of Bernard–Soulier syndrome. Haematologica. 2009;94:800–10.
Vettore S, Tezza F, Malara A, Vianello F, Pecci A, Scandellari R, et al. A A386G biallelic GPIbα gene mutation with anomalous behavior: a new mechanism suggested for Bernard–Soulier syndrome pathogenesis. Haematologica. 2011;96:1878–82.
Balduini A, Malara A, Balduini CL, Noris P. Megakaryocytes derived from patients with the classical form of Bernard–Soulier syndrome show no ability to extend proplatelets in vitro. Platelets. 2011;22:308–11.
Noris P, Perrotta S, Bottega R, Pecci A, Melazzini F, Civaschi E, et al. Clinical and laboratory features of 103 patients from 42 Italian families with inherited thrombocytopenia derived from the monoallelic Ala156Val mutation of GPIbα (Bolzano mutation). Haematologica. 2012;97:82–8.
Balduini A, Malara A, Pecci A, Badalucco S, Bozzi V, Pallotta I, et al. Proplatelet formation in heterozygous Bernard–Soulier syndrome type Bolzano. J Thromb Haemost. 2009;7:478–84.
Kanaji T, Russell S, Ware J. Amelioration of the macrothrombocytopenia associated with the murine Bernard–Soulier syndrome. Blood. 2002;100:2102–7.
Ghevaert C, Salsmann A, Watkins NA, Schaffner-Reckinger E, Rankin A, Garner SF, et al. A nonsynonymous SNP in the ITGB3 gene disrupts the conserved membrane-proximal cytoplasmic salt bridge in the alphaIIbbeta3 integrin and cosegregates dominantly with abnormal proplatelet formation and macrothrombocytopenia. Blood. 2008;111:3407–14.
Kunishima S, Kashiwagi H, Otsu M, Takayama N, Eto K, Onodera M, et al. Heterozygous ITGA2B R995W mutation inducing constitutive activation of the αIIbβ3 receptor affects proplatelet formation and causes congenital macrothrombocytopenia. Blood. 2011;117:5479–84.
Schaffner-Reckinger E, Salsmann A, Debili N, Bellis J, De Mey J, Vainchenker W, et al. Overexpression of the partially activated alpha(IIb)beta3D723H integrin salt bridge mutant downregulates RhoA activity and induces microtubule-dependent proplatelet-like extensions in Chinese hamster ovary cells. J Thromb Haemost. 2009;7:1207–17.
Massaad MJ, Ramesh N, Geha RS. Wiskott-Aldrich syndrome: a comprehensive review. Ann N Y Acad Sci. 2013; Mar 25 [Epub ahead of print].
Prislovsky A, Marathe B, Hosni A, Bolen AL, Nimmerjahn F, Jackson CW, et al. Rapid platelet turnover in WASP(−) mice correlates with increased ex vivo phagocytosis of opsonized WASP(−) platelets. Exp Hematol. 2008;36:609–23.
Baldini MG. Nature of the platelet defect in the Wiskott–Aldrich syndrome. Ann N Y Acad Sci. 1972;201:437–44.
Prislovsky A, Zeng X, Sokolic RA, Garabedian EN, Anur P, Candotti F, et al. Platelets from WAS patients show an increased susceptibility to ex vivo phagocytosis. Platelets. 2012;24:288–96.
Marathe BM, Prislovsky A, Astrakhan A, Rawlings DJ, Wan JY, Strom TS. Antiplatelet antibodies in WASP(−) mice correlate with evidence of increased in vivo platelet consumption. Exp Hematol. 2009;37:1353–63.
Sabri S, Foudi A, Boukour S, Franc B, Charrier S, Jandrot-Perrus M, et al. Deficiency in the Wiskott–Aldrich protein induces premature proplatelet formation and platelet production in the bone marrow compartment. Blood. 2006;108:134–40.
Rees DC, Iolascon A, Carella M, O’marcaigh AS, Kendra JR, Jowitt SN, et al. Stomatocytic haemolysis and macrothrombocytopenia (Mediterranean stomatocytosis/macrothrombocytopenia) is the haematological presentation of phytosterolaemia. Br J Haematol. 2005;130:297–309.
Kidambi S, Patel SB. Sitosterolaemia: pathophysiology, clinical presentation and laboratory diagnosis. J Clin Pathol. 2008;61:588–94.
Kruit JK, Drayer AL, Bloks VW, Blom N, Olthof SG, Sauer PJ, et al. Plant sterols cause macrothrombocytopenia in a mouse model of sitosterolemia. J Biol Chem. 2008;283:6281–7.
Fei Z, Bera TK, Liu X, Xiang L, Pastan I. Ankrd26 gene disruption enhances adipogenesis of mouse embryonic fibroblasts. J Biol Chem. 2011;286:27761–8.
Noris P, Perrotta S, Seri M, Pecci A, Gnan C, Loffredo G, et al. Mutations in ANKRD26 are responsible for a frequent form of inherited thrombocytopenia: analysis of 78 patients from 21 families. Blood. 2011;117:6673–80.
Necchi V, Balduini A, Noris P, Barozzi S, Sommi P, di Buduo C, et al. Ubiquitin/proteasome-rich particulate cytoplasmic structures (PaCSs) in the platelets and megakaryocytes of ANKRD26-related thrombo-cytopenia. Thromb Haemost. 2013;109:263–71.
Köhler M, Hellstern P, Morgenstern E, Mueller-Eckhardt C, Berberich R, Meiser RJ, et al. Gray platelet syndrome: selective alpha-granule deficiency and thrombocytopenia due to increased platelet turnover. Blut. 1985;50:331–40.
Gunay-Aygun M, Zivony-Elboum Y, Gumruk F, Geiger D, Cetin M, Khayat M, et al. Gray platelet syndrome: natural history of a large patient cohort and locus assignment to chromosome 3p. Blood. 2010;116:4990–5001.
George JN, Shattil SJ. The clinical importance of acquired abnormalities of platelet function. N Engl J Med. 1991;324:27–39.
Peaceman AM, Katz AR, Laville M. Bernard–Soulier syndrome complicating pregnancy: a case report. Obstet Gynecol. 1989;73:457–9.
Moratto D, Giliani S, Bonfim C, Mazzolari E, Fischer A, Ochs HD, et al. Long-term outcome and lineage-specific chimerism in 194 patients with Wiskott–Aldrich syndrome treated by hematopoietic cell transplantation in the period 1980–2009: an international collaborative study. Blood. 2011;118:1675–84.
Locatelli F, Rossi G, Balduini C. Hematopoietic stem-cell transplantation for the Bernard–Soulier syndrome. Ann Intern Med. 2003;138:79.
Rieger C, Rank A, Fiegl M, Tischer J, Schiel X, Ostermann H, et al. Allogeneic stem cell transplantation as a new treatment option for patients with severe Bernard–Soulier Syndrome. Thromb Haemost. 2006;95:190–1.
Albert MH, Bittner TC, Nonoyama S, Notarangelo LD, Burns S, Imai K, et al. X-linked thrombocytopenia (XLT) due to WAS mutations: clinical characteristics, long-term outcome, and treatment options. Blood. 2010;115:3231–8.
Balduini CL, Noris P, Belletti S, Spedini P, Gamba G. In vitro and in vivo effects of desmopressin on platelet function. Haematologica. 1999;84:891–6.
Tosetto A, Balduini CL, Cattaneo M, De Candia E, Mariani G, Molinari AC, et al. Management of bleeding and of invasive procedures in patients with platelet disorders and/or thrombocytopenia: guidelines of the Italian Society for Haemostasis and Thrombosis (SISET). Thromb Res. 2009;124:13–8.
Pecci A, Barozzi S, d’Amico S, Balduini CL. Short-term eltrombopag for surgical preparation of a patient with inherited thrombocytopenia deriving from MYH9 mutation. Thromb Haemost. 2012;107:1188–9.
Gröpper S, Althaus K, Najm J, Haase S, Aul C, Greinacher A, et al. A patient with Fechtner syndrome successfully treated with romiplostim. Thromb Haemost. 2012;107:590–1.
Bussel JB, Frelinger AL III, Mitchell WB, Pinheiro MP, Barnard MR, Lampa M, et al. Platelet function and response to thrombopoietin mimetics in Wiskott–Aldrich syndrome/X-linked thrombocytopenia. Blood (ASH annual meeting abstracts). 2010;116:1429.
Tijssen MR, di Summa F, van den Oudenrijn S, Zwaginga JJ, van der Schoot CE, Voermans C, et al. Functional analysis of single amino-acid mutations in the thrombopoietin-receptor Mpl underlying congenital amegakaryocytic thrombocytopenia. Br J Haematol. 2008;141:808–13.
Freson K, Devriendt K, Matthijs G, Van Hoof A, De Vos R, Thys C, et al. Platelet characteristics in patients with X-linked macrothrombocytopenia because of a novel GATA1 mutation. Blood. 2001;98:85–92.
Basciano PA, Bussel JB. Thrombopoietin-receptor agonists. Curr Opin Hematol. 2012;19:392–8.
Girolami A, Vettore S, Bonamigo E, Fabris F. Thrombotic events in MYH9 gene-related autosomal macrothrombocytopenias (old May–Hegglin, Sebastian, Fechtner and Epstein syndromes). J Thromb Thrombolysis. 2011;32:474–7.
Heller PG, Pecci A, Glembotsky AC, Savoia A, Negro FD, Balduini CL, et al. Unexplained recurrent venous thrombosis in a patient with MYH9-related disease. Platelets. 2006;17:274–5.
McDunn S, Hartz W Jr, Ts’Ao C, Green D. Coronary thrombosis in a patient with May–Hegglin anomaly. Am J Clin Pathol. 1991;95:715–8.
Althaus K, Greinacher A. MYH-9 related platelet disorders: strategies for management and diagnosis. Transfus Med Hemother. 2010;37:260–7.
Kantarjian H, Fenaux P, Sekeres MA, Becker PS, Boruchov A, Bowen D, et al. Safety and efficacy of romiplostim in patients with lower-risk myelodysplastic syndrome and thrombocytopenia. J Clin Oncol. 2010;28:437–44.
Sekeres MA, Kantarjian H, Fenaux P, Becker P, Boruchov A, Guerci-Bresler A, et al. Subcutaneous or intravenous administration of romiplostim in thrombocytopenic patients with lower risk myelodysplastic. syndromes. Cancer. 2011;117:992–1000.
Léon C, Evert K, Dombrowski F, Pertuy F, Eckly A, Laeuffer P, et al. Romiplostim administration shows reduced megakaryocyte response-capacity and increased myelofibrosis in a mouse model of MYH9-RD. Blood. 2012;119:3333–41.
Acknowledgments
The author thanks Prof. Carlo Balduini for helpful discussion and Dr. Serena Barozzi for assistance in manuscript preparation.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Pecci, A. Pathogenesis and management of inherited thrombocytopenias: rationale for the use of thrombopoietin-receptor agonists. Int J Hematol 98, 34–47 (2013). https://doi.org/10.1007/s12185-013-1351-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12185-013-1351-7