Abstract
Socioeconomic gradients in health behavior are pervasive and well documented. Yet, there is little consensus on their causes. Behavioral ecological theory predicts that, if people of lower socioeconomic position (SEP) perceive greater personal extrinsic mortality risk than those of higher SEP, they should disinvest in their future health. We surveyed North American adults for reported effort in looking after health, perceived extrinsic and intrinsic mortality risks, and measures of SEP. We examined the relationships between these variables and found that lower subjective SEP predicted lower reported health effort. Lower subjective SEP was also associated with higher perceived extrinsic mortality risk, which in turn predicted lower reported health effort. The effect of subjective SEP on reported health effort was completely mediated by perceived extrinsic mortality risk. Our findings indicate that perceived extrinsic mortality risk may be a key factor underlying SEP gradients in motivation to invest in future health.
Similar content being viewed by others
Socioeconomic gradients in health outcomes are pervasive and well documented (Adler and Ostrove 1999; Melchior et al. 2011); people of lower SEP have shorter life expectancies and shorter healthy life expectancies than those of higher SEP (Crimmins and Saito 2001; Liao et al. 1999; Phelan et al. 2010; Wilkinson 1992). Evidence suggests that socioeconomic differences in health behavior account for up to half of the socioeconomic health gradient (Mokdad et al. 2004; Stringhini et al. 2010). People of lower SEP are more likely to smoke or to drink excessively than those of higher SEP (Harrell et al. 1998; Pridemore et al. 2010), and are less likely to take part in regular physical activity (McLaren 2007; Wardle et al. 2002). They are also less likely to adhere to treatment programs, even when there is no financial cost to doing so (Barr et al. 2002; Goldman and Smith 2002). The reasons for this SEP gradient in health behaviors have become an enduring point of debate across a range of disciplines including epidemiology, public health, health psychology, sociology and behavioral economics (Pampel et al. 2010).
Many nuanced explanations for SEP gradients in health behavior have been put forward, but there is currently little consensus across disciplines regarding their causes (Cutler and Lleras-Muney 2010; Pampel et al. 2010; Pepper and Nettle 2014). Some explanations are based on the idea that people of lower SEP face constraints which people of higher SEP do not. These explanations posit that a lack of resources (a fundamental component of SEP) or a lack of specific health knowledge (potentially related to the education component of SEP) constrains people’s ability to protect their health. The first constraint-based explanation, that people of lower SEP lack the resources to “purchase” health (Darmon and Drewnowski 2008), cannot be a considered a complete one because it does not apply to some of the most common health-damaging behaviors. Smoking, poor diet, physical inactivity, and alcohol consumption are major behavioral causes of mortality. Indeed, they were reported to have been the leading causes of death in the United States in the year 2000 (Mokdad et al. 2004). For at least two out of these four behaviors (smoking and alcohol consumption), the unhealthy option (consumption) is more financially costly than the healthy one (abstinence). Thus, the people who can least afford to spend money are spending money on behaviors that damage their health.
The second constraint-based explanation is that the socioeconomic gradient in health behavior is the result of socioeconomic differences in specific health knowledge (e.g., Siahpush et al. 2006). However, providing specific health information does not change behavior equally among high and low SEP individuals. For example, in the UK between 2003 and 2008 there was extensive government investment in public health information campaigns. Buck and Frosini (2012) examined how four behaviors (smoking, excessive alcohol use, poor diet, and low levels of physical activity) changed during this time. They found that high SEP individuals dramatically reduced their levels of unhealthy behavior during the public health campaign period, whereas low SEP individuals did not. Receiving specific health information may have improved behavior in individuals already motivated to invest in health, while failing to change behavior in others. Other studies have found that knowledge of the harms of smoking or the importance of exercise, for example, is widespread and differs minimally by SEP (Layte and Whelan 2009; Pampel et al. 2010). This raises the possibility that there is greater incentive for higher SEP individuals to invest in protecting their health than there is for individuals of lower SEP. In support of this, evidence suggests that desire to quit smoking and use of cessation tools do not differ across social class, whereas quitting success does (Kotz and West 2009). This implies that there is an SEP gradient in motivation to quit, rather than in knowledge that smoking is bad for health. We have given just a few examples here, but there is a wide range of evidence demonstrating SEP differences in response to health interventions (see White et al. 2009).
If constraint-based explanations are incomplete, then we must turn to alternatives. We have argued elsewhere that most of the explanations put forward in the non-evolutionary literature are proximate ones that are potentially consilient with a single ultimate explanation, which we will now discuss (Pepper and Nettle 2014). This ultimate explanation does not necessarily conflict with other explanations invoking proximate mechanisms such as stress, social networks, or efficacy and agency. It is simply a different level of explanation.
In previous work, we presented a theoretical model to explain SEP gradients in health behavior using an adaptive framework from behavioral ecology (Nettle 2010). Following a long tradition in evolutionary biology (Medawar 1952; Williams 1957), the model divided the risk of mortality into two components: an extrinsic component, which remains the same regardless of the behavioral decisions that the individual makes, and an intrinsic component, which reflects how much effort the individual invests in preventing the health risks that can be mitigated. The model assumed that health-protecting investments are costly, in the sense that the time and energy devoted to them must be taken away from other activities that individuals value. (There is a trade-off between investing in health behavior and investing in other adaptively relevant activities.) The results of the model showed that as the extrinsic component of mortality risk increases, the optimal investment in protective health behavior decreases. Under conditions of high extrinsic mortality, the value of health-protecting investments is reduced, since even if one makes them, one may well be killed by something extrinsic anyway. Thus, people facing higher extrinsic mortality risks should reduce their investment in preventative health behavior and reallocate their investment toward other things. If people of lower SEP perceive that they face increased extrinsic mortality risk relative to people of higher SEP, then reduced investment of energy in long-term health could be an adaptively patterned response to the perceived environment, rather than a result of constraints or mistakes.
The model we have just described, though specific to health behaviors, is derived from life history theory. Models of the evolution of life histories predict that adaptively relevant behaviors such as reproductive scheduling and parental investment should be sensitive to mortality rates (see Stearns 1992), and this prediction is borne out by comparative evidence (e.g., Harvey and Zammuto 1985). An extension of this concept within human behavioral ecology is the idea that humans have evolved the capacity to ontogenetically calibrate their reproductive strategies in response to local mortality risk (e.g., Chisholm et al. 1993; Lawson and Mace 2011; Nettle 2011; Wilson and Daly 1997). Indeed, empirical work has demonstrated associations between mortality rates and indicators of life history strategy (Low et al. 2008; Nettle et al. 2011; Quinlan 2010). However, nothing has been done specifically to investigate the associations between perceived extrinsic mortality risk and motivation to invest in health. Here we will focus on perceived extrinsic mortality risk. We do so because, although evidence suggests that people of lower SEP are generally exposed to greater risk of extrinsic mortality (e.g., Bolte et al. 2010; Soskolne and Mano 2010), we do not know that they perceive this to be the case. We look for SEP differences in reported effort in looking after health and safety in general because, as discussed above, SEP differences in health behavior may reflect SEP differences in motivation to look after health, rather than constraints in their ability to protect their health.
In this paper, we report our findings from a survey of North American adults which included questions designed to test our hypothesis—that perceived extrinsic mortality risk would mediate the relationship between SEP and effort in looking after health. We collected measures of income, subjective SEP, effort made in looking after health, and perceived risk of mortality. Perceived risk of mortality, or its inverse, subjective life expectancy, has been widely studied (Dunkel et al. 2010; Krupp 2012), but we introduced a novel method to discriminate the extrinsic component of perceived mortality from the intrinsic component. Based on the evolutionary model described above (Nettle 2010), we made the following predictions:
-
1.
Lower SEP will be associated with greater perceived extrinsic mortality risk, rather than perceived intrinsic mortality risk.
-
2.
Greater perceived extrinsic mortality risk will be associated with lower reported effort in looking after health.
-
3.
The relationship between SEP and reported effort in looking after health will be mediated by perceived extrinsic mortality risk.
Methods
Data Collection
The study was approved by the Newcastle University Faculty of Medical Sciences Ethics Committee. 600 North American volunteers were surveyed anonymously online using the SocialSci survey platform [www.socialsci.com]. Respondents had previously signed up to take part in surveys via this platform. SocialSci recruits using a distributed online advertising network, print media, and live recruitment. They award Amazon (www.amazon.com) credit to respondents for taking part in their surveys. Respondents completed an electronic consent form before proceeding. They were then asked for basic demographic information: age, gender, and gross annual income. Following this, we collected measures of reported effort spent looking after health, perceived risk of mortality, and subjective SEP.
Measures of SEP
We measured SEP in two different ways. First, we asked respondents to enter their gross annual income in US$ into a free-text box. This measure was captured at the beginning of the survey along with age and gender. A free-text box was used to avoid unintentional priming effects that could be elicited by using income brackets (Haisley et al. 2008). Income was square-root transformed for analysis. Respondents were also asked to complete a subjective measure of SEP taken from prior studies (Griskevicius et al. 2011). This was done at the end of the survey, to avoid priming effects. They were asked to rate their agreement on a scale from 1 (strongly disagree) to 7 (strongly agree) with the statements: (a) “I don’t worry too much about paying my bills”; (b) “I have enough money to buy things I want,” and (c) “I don’t think I’ll have to worry about money too much in the future.” The three responses correlated well with one another (r = 0.56–0.68, p < 0.01) and hence we summed them to give an overall subjective SEP score. The income and subjective SEP measures were correlated with one another (r = 0.30, p < 0.01), but not so highly as to treat them as equivalent. Income and subjective SEP were therefore entered separately into all our analyses.
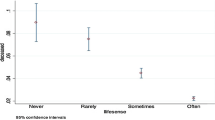
Reported Effort in Looking after Health
As a measure of motivation to invest in health, respondents were asked, “How much effort do you make to look after your health and ensure your safety these days? 0 is ‘no effort at all’ and 100 is ‘the maximum effort you could make.’” This question was asked before the questions used to determine perceived risk of mortality. Questions about general motivation to protect health have been found to be predictive of a range of health behaviors (e.g., Becker et al. 1972; Mirotznik et al. 1998). We used a single general question about motivation because responses to multiple questions about individual health behaviors often need to be summed to show the same effect as a single, more general motivation question in relation to actual behavior (e.g., Becker et al. 1977; Mirotznik et al. 1995, 1998).
Perceived Risk of Extrinsic and Intrinsic Mortality
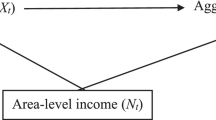
We created two novel survey items to separate out the extrinsic and intrinsic components of perceived mortality risk. We asked, “If you made the maximum effort you could make to look after your health and ensure your safety, what do you think the chances would be that you would live to be 75 or more? 0 is ‘no chance’ and 100 is ‘definitely.’” The extrinsic component of subjective mortality risk (henceforth perceived extrinsic mortality risk) is 100 minus this response. It is the portion of perceived mortality risk that the individual believes they cannot reduce via health effort. We then asked respondents, “If you made no effort at all to look after your health and ensure your safety, what do you think the chances would be that you would live to be 75 or more? Again, 0 is ‘no chance’ and 100 is ‘definitely.’” Our perceived intrinsic mortality risk variable was the difference between the preceding question and this one. That is, it is the portion of overall perceived mortality risk which the respondent believes they are able to reduce via health effort. The relationship between our original measures and these variables is illustrated in Fig. 1. We have also illustrated the predicted relationship between perceived mortality risks and subjective SEP in Fig. 2a.
Schematic of our measures of perceived extrinsic and intrinsic mortality risk. The perceived extrinsic risk is the difference between 100% and the perceived chances of surviving to age 75 with maximum effort in looking after health. It is the portion of perceived mortality risk that the individual believes they cannot reduce via health effort. The perceived intrinsic risk is the difference between the perceived chances of living to 75 with maximum effort in looking after health, and with minimum effort in looking after health. It is the portion of perceived mortality risk which the individual believes they can reduce via health effort
A: Predicted relationship between SEP and perceived mortality risk (arbitrary units). We predicted that it would be the perceived extrinsic mortality risk rather than the perceived intrinsic mortality risk that would show a social gradient. B: A plot of the observed relationship between our subjective SEP measure and perceived mortality with subjective SEP split into quartiles
Analysis
We excluded 138 respondents who were under the age of 21 since measures of income and subjective SEP are likely to be unstable in participants younger than this age. We also excluded 22 individuals who spent less than 2 min completing the survey, the minimum possible time to engage with the questions established by piloting; 1 individual whose reported income was more than 10 standard deviations above the mean; and 1 individual whose sex was missing. This left a final sample of 438 respondents. We give details of the effect of these exclusions in the results section. We tested our three predictions using General Linear Models (GLM) in SPSS version 19.0, with age and sex as control variables in all cases. For prediction 3, we tested the statistical significance of mediation with a Sobel test (Preacher and Hayes 2004).
Results
The raw data are downloadable as an online supplement to this paper. Of the 438 respondents included in the analysis, 184 were male and 254 were female. Ages ranged from 21 to 72 years (mean = 30.11 years, SD = 9.65). Reported personal annual incomes ranged from $0 to $250,000 (untransformed mean = $39,307, SD = $38,888). Subjective SEP ranged from the minimum possible score of 3 to the maximum possible score of 21 (mean = 11.11, SD = 4.90).
Prediction 1
Lower SEP will be associated with greater perceived extrinsic mortality risk, rather than perceived intrinsic mortality risk.
We ran a multivariate GLM with perceived extrinsic and intrinsic mortality risk as the outcome variables, and income, subjective SEP, age, and sex as the predictors. Subjective SEP was negatively associated with perceived extrinsic mortality (F 1,433 = 6.97, p < 0.01). That is, higher subjective SEP was associated with lower perceived extrinsic mortality (B = −0.83, s.e.[B] = 0.31). Income was not associated with perceived extrinsic mortality risk (F 1,433 = 1.34, p = 0.25). Neither subjective SEP (F 1,433 = 0.86, p = 0.36) nor income (F 1,433 = 0.18, p = 0.67) were significantly associated with perceived intrinsic mortality risk. (See Table 1 for full model results). Thus, for subjective SEP but not for income, our results conformed to the pattern we predicted (Fig. 2b).
Prediction 2
Greater perceived extrinsic mortality risk will be associated with lower reported effort in looking after health.
In a GLM with reported effort looking after health as the outcome variable and perceived extrinsic and intrinsic mortality risk along with age and sex as the predictors, both perceived extrinsic (F 1,433 = 244.13, p < 0.01) and perceived intrinsic (F 1, 433 = 5.42, p = 0.20) mortality risk were significantly associated with reported effort looking after health. Both associations were negative, with higher perceived mortality risk associated with lower reported effort (extrinsic: B = −0.64, s.e.[B] = 0.04; intrinsic: B = −0.10, s.e.[B] = 0.04). However, the association of reported health effort with perceived extrinsic mortality risk was much stronger than that with perceived intrinsic mortality risk. Perceived extrinsic mortality risk explained a substantial fraction of the variation not accounted for by other variables (ηp 2 = 0.362), and perceived intrinsic mortality risk explained very little of the variation not accounted for by other variables (ηp 2 = 0.012). (See Table 2 for full model results.)
Prediction 3
The relationship between SEP and reported effort in looking after health will be mediated by perceived extrinsic mortality risk.
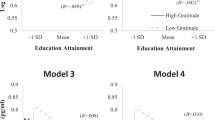
To test prediction 3, we followed the steps laid out by Baron and Kenny (1986) for detecting mediation effects. We could not test for mediation of the association between income and reported health effort because the former was not a predictor of the latter. However, subjective SEP was a significant predictor of reported effort in looking after health, with age, sex, and income controlled (F 1,433 = 3.94, p = 0.048, B = 0.56, s.e.[B] = 0.28; see Table 3 for full model results). We had already established that subjective SEP was a predictor of extrinsic mortality perception (see prediction 1). To test for mediation, we added perceived extrinsic mortality to the GLM predicting reported effort in looking after health from age, sex, subjective SEP, and income (this is the model in Table 2). We found that the relationship between subjective SEP and health behavior was no longer significant (F 1,433 = 0.06, p = 0.803) because perceived extrinsic mortality (F 1,433 = 244.13, p < 0.01) explained the variation that was explained by SEP in Model 1 (Table 4). This suggests complete mediation (Baron and Kenny 1986), a conclusion supported by a significant Sobel test (z = 2.65, p < 0.01).
Effects on our Results of Including Participants Under the Age of 21
In the analyses reported above, we excluded 138 respondents who were under the age of 21 because we felt that personal income would not be an accurate reflection of their actual SEP, and parental income measures are often inaccurately reported (Boyce et al. 2006). Indeed, the correlation of income with subjective SEP increased from r = 0.20 (p < 0.01) to r = 0.30 (p < 0.01) after these younger participants were excluded. Nonetheless, for completeness, we also present the results of the analyses without any data excluded. They are as follows: The association between subjective SEP and reported health effort (controlling for age, sex, and income) was no longer significant when participants under 21 were included (F 1,559 = 2.51, p = 0.114, ηp 2 = 0.004). This means that we were unable to test for mediation. Nevertheless, with the younger participants included, perceived extrinsic mortality (controlling for age, sex, income, subjective SEP, and perceived intrinsic mortality) remained a significant predictor of reported health effort, with a large effect size (F 1,559 = 318.20, p < 0.01, ηp 2 = 0.364). Despite the fact that we were unable to formally test for mediation, this result supports our hypothesis that perceived extrinsic mortality risk, which is often associated with SEP, is potentially a better predictor of health effort than SEP per se.
Discussion
Our previously presented theoretical model (Nettle 2010) led us to predict that perceptions of high extrinsic mortality risk would trigger psychological mechanisms that cause disinvestment in preventative health measures. We argued that this might explain the socioeconomic gradient in health behavior, if people of lower SEP are, or perceive themselves to be, at greater risk of extrinsic mortality (Nettle 2010; Pepper and Nettle 2014). Here, we collected survey data to test this hypothesis. We found a socioeconomic gradient in perceived mortality risk, with greater perceived risk among those of lower subjective SEP. Separating out the extrinsic and intrinsic components of this risk showed that it was the extrinsic component of perceived risk that increased as subjective SEP decreased, with no gradient in the intrinsic component (Fig. 2b). Perceived extrinsic mortality risk was strongly negatively associated with reported effort in looking after health, whereas perceived intrinsic mortality risk was only weakly associated with it (Table 2). We found that our subjective measure of SEP, but not gross annual income, was positively associated with reported effort in looking after health. However, this association was completely mediated by perceived extrinsic mortality risk. This suggests that people of lower subjective SEP may be less motivated to look after their health, but only because they perceive themselves to be subject to mortality risks that are beyond their control.
These results are consistent with previous empirical findings that people of lower SEP tend to be more fatalistic about their health outcomes and have a greater belief in the influence of chance on their health than those of higher SEP (Wardle and Steptoe 2003). However, they also demonstrate the benefits of taking an adaptively informed approach to understand variation in human behavior in the sphere of health. Our a priori theoretical model (Nettle 2010), based on the behavioral ecological literature, suggested the potential importance of distinguishing extrinsic from intrinsic mortality, and it also predicted that extrinsic mortality motivated people to reduce their effort in looking after their health.
There are a number of limitations to the current study. We used an opportunity sample recruited through an existing online participant pool. It would be desirable to investigate whether the same patterns are found in population-representative samples. Our main SEP measures were income and a self-report scale. Income reporting in surveys is often inaccurate; disposable income, though more complex to assess, may be a better predictor of behavior (Moore et al. 2000; Winkler et al. 2006). The subjective SEP measure we used did capture more fine-grained aspects of resource availability, such as disposable income and financial stability, that would not be captured simply by asking people for their gross annual income. However, this was a self-report measure of SEP: Although it was simple to administer, its relationship to more objective factors such as education and occupational status has not been explored here. To address this it would be ideal for a measure of perceived extrinsic mortality risk to be included in large health surveys in which respondents’ SEPs are well characterized. The socioeconomic gradient in reported health effort was only detectable in our sample with the participants under the age of 21 excluded from analysis. However, the existence of socioeconomic gradients in health behavior is extremely well documented in previous literature, and the null association in our sample without exclusions may simply reflect the instability of self-reported income and subjective SEP in participants who are not yet financially independent. Even with large samples, studies on the relationship between SEP and health behaviors often find small effects, especially when they use individual health behaviors rather than composite measures (e.g., Friestad and Klepp 2006; Halleröd and Gustafsson 2011; Hanson and Chen 2007). So, though associations between SEP and health behavior are reliably uncovered in a variety of studies, effect sizes in individual studies tend to be small. Our findings suggest that this may be because a third variable—extrinsic mortality risk—accounts for much of the relationship between SEP and health behavior. In our data, the effect size for the relationship between perceived extrinsic mortality risk and reported health effort (ηp 2 = 0.362) was substantially greater than for the association between our subjective SEP measure and reported health effort (ηp 2 = 0.009). Indeed, the relationship between subjective SEP and reported health effort was entirely extinguished when perceived extrinsic mortality risk was added to the model (Table 4). This may be because our measures of SEP were not comprehensive. However, it may also be because SEP-related differences in perceived extrinsic mortality risk have greater power to explain differences in health effort than SEP per se. This possibility should be investigated further.
Our findings have potential implications in applied settings. They suggest that people of lower SEP may not make less effort to look after their health whimsically or through ignorance. Rather, they perceive that whatever they do, there is a relatively high chance that they will be killed by something that they can do nothing about, so they follow a behavioral strategy of investing more of their energy in other things. Improving our understanding of what shapes perceived extrinsic mortality risk, and how to alter it, could therefore increase the efficacy of public health interventions.
As discussed in the introduction, our predictions about SEP gradients in health effort were derived from life history theory. Models of the evolution of life histories predict that behaviors such as health effort, reproductive scheduling, and parental investment should be sensitive to mortality risk. However, they also predict that if extrinsic mortality risk is high, we might expect a more general shift in time horizons (Hill et al. 2008; Kruger et al. 2008; Wilson and Daly 1997). That is, we might predict an increased tendency to prioritize immediate rewards and costs above delayed ones because, when risk of death is higher, the odds of being alive to receive future rewards are lower. There is some evidence that changes in time horizons occur in response to perceived mortality risk. When experimentally exposed to mortality primes, people who reported having low childhood SEP have been found to discount the future more steeply than those who were exposed to control primes (Griskevicius et al. 2011). People who reported suffering a greater number of recent close bereavements have been found to discount the future more steeply than those who had suffered fewer (Pepper and Nettle 2013). Exposure to violence has been found to be associated with future discounting (Ramos et al. 2013), and earthquake survivors have been found to discount future rewards more steeply than controls (Li et al. 2012). Given the large body of literature linking time perspective and related concepts, such as delay discounting and impulsivity, to health behavior (Adams 2009; Adams and Nettle 2009; Beenstock et al. 2011; White et al. 2009), it is plausible that perceived extrinsic mortality risk affects both time horizons and motivation towards health effort, thus accounting for the associations found between them. However, to our knowledge, there have been no direct tests of the impact of extrinsic mortality cues on health behaviors. It is important that such tests be developed.
The research presented here focused on perceived extrinsic mortality risk. However, relatively little is known about the environmental cues that produce these perceptions. Cues might include exposure to violent crime or knowing people who have died from circumstances beyond their control. Indeed, evidence suggests that fear of crime and experiences of bereavement are associated with poor health (Chandola 2001; Stafford et al. 2007; Stroebe et al. 2007). It would be useful to understand to what extent such cues contribute to a person’s perceived extrinsic mortality risk and whether qualitative differences between cues are important. It would also be useful to know how accurate people’s perceptions of mortality risk are. Some epidemiological evidence suggests that actual as well as perceived extrinsic mortality risk is higher in low-SEP communities (Bolte et al. 2010; Soskolne and Mano 2010). Although there may be a veridical basis to these perceptions, they may be inflated by media scare stories or by exaggerated accounts from peers. If this is the case, then something as simple as correcting people’s perceptions may be enough to improve their health behaviors. However, this is not to understate the fundamental importance of public action to tackle the sources of extrinsic mortality that differentially affect those of lower SEP. Not only would making low-SEP neighborhoods and workplaces safer have the primary benefit of reducing extrinsic mortality, it could also produce a secondary benefit of improved health behaviors. This would have the overall effect of reducing socioeconomic inequalities in health.
References
Adams, J. (2009). Time for a change of perspective on behaviour change interventions? Addiction, 104, 1025–1026.
Adams, J., & Nettle, D. (2009). Time perspective, personality and smoking, body mass, and physical activity: an empirical study. British Journal of Health Psychology, 14(1), 83–105.
Adler, N. E., & Ostrove, J. M. (1999). Socioeconomic status and health: what we know and what we don’t. Annals of the New York Academy of Sciences, 896, 3–15.
Baron, R. M., & Kenny, D. A. (1986). The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology, 51(6), 1173–1182.
Barr, R. G., Somers, S. C., Speizer, F. E., & Camargo, C. A. (2002). Patient factors and medication guideline adherence among older women with asthma. Archives of Internal Medicine, 162(15), 1761–1768.
Becker, M. H., Drachman, R. H., & Kirscht, J. P. (1972). Motivations as predictors of health behavior. Health Services Reports, 87(9), 852–862.
Becker, M., Maiman, L., Kirscht, J., Haefner, D. P., & Drachman, R. H. (1977). The Health Belief Model and prediction of dietary compliance: a field experiment. Journal of Health and Social Behavior, 18(4), 348–366.
Beenstock, J., Adams, J., & White, M. (2011). The association between time perspective and alcohol consumption in university students: cross-sectional study. European Journal of Public Health, 21(4), 438–443.
Bolte, G., Tamburlini, G., & Kohlhuber, M. (2010). Environmental inequalities among children in Europe: evaluation of scientific evidence and policy implications. European Journal of Public Health, 20(1), 14–20.
Boyce, W., Torsheim, T., Currie, C., & Zambon, A. (2006). The family affluence scale as a measure of national wealth: validation of an adolescent self-report measure. Social Indicators Research, 78(3), 473–487.
Buck, D., & Frosini, F. (2012). Clustering of unhealthy behaviours over time: Implications for policy and practice. The King’s Fund. Available online at http://www.kingsfund.org.uk/sites/files/kf/field/field_publication_file/clustering-of-unhealthy-behaviours-over-time-aug-2012.pdf
Chandola, T. (2001). The fear of crime and area differences in health. Health & Place, 7(2), 105–116.
Chisholm, J. S., Ellison, P. T., Evans, J., Lee, P. C. C., Lieberman, L. S., Pavlik, Z., & Worthman, C. M. (1993). Death, hope, and sex: life-history theory and the development of reproductive strategies. Current Anthropology, 34(1), 1–24.
Crimmins, E. M., & Saito, Y. (2001). Trends in healthy life expectancy in the United States, 1970–1990: gender, racial, and educational differences. Social Science & Medicine, 52(11), 1629–1641.
Cutler, D. M., & Lleras-Muney, A. (2010). Understanding differences in health behaviors by education. Journal of Health Economics, 29(1), 1–28.
Darmon, N., & Drewnowski, A. (2008). Does social class predict diet quality? American Journal of Clinical Nutrition, 87, 1107–1117.
Dunkel, C., Mathes, E., & Decker, M. (2010). Behavioral flexibility in life history strategies: The role of life expectancy. Journal of Social, Evolutionary and Cultural Psychology, 4(2), 51–61.
Friestad, C., & Klepp, K.-I. (2006). Socioeconomic status and health behaviour patterns through adolescence: results from a prospective cohort study in Norway. European Journal of Public Health, 16(1), 41–47.
Goldman, D. P., & Smith, J. P. (2002). Can patient self-management help explain the SES health gradient? Proceedings of the National Academy of Sciences USA, 99(16), 10929–10934.
Griskevicius, V., Tybur, J. M., Delton, A. W., & Robertson, T. E. (2011). The influence of mortality and socioeconomic status on risk and delayed rewards: A life history theory approach. Journal of Personality and Social Psychology, 100(6), 1015–1026.
Haisley, E., Mostafa, R., & Loewenstein, G. (2008). Subjective relative income and lottery ticket purchases. Journal of Behavioral Decision Making, 21, 283–295.
Halleröd, B., & Gustafsson, J.-E. (2011). A longitudinal analysis of the relationship between changes in socio-economic status and changes in health. Social Science & Medicine (1982), 72(1), 116–123.
Hanson, M. D., & Chen, E. (2007). Socioeconomic status and health behaviors in adolescence: a review of the literature. Journal of Behavioral Medicine, 30(3), 263–285.
Harrell, J., Bangdiwala, S., Deng, S., Webb, J., & Bradley, C. (1998). Smoking initiation in youth: the roles of gender, race, socioeconomics, and developmental status. Journal of Adolescent Health, 23, 271–279.
Harvey, P. H., & Zammuto, R. M. (1985). Patterns of mortality and age at first reproduction in natural populations of mammals. Nature, 315, 319–320.
Hill, E., Jenkins, J., & Farmer, L. (2008). Family unpredictability, future discounting, and risk taking. Journal of Socio-Economics, 37, 1381–1396.
Kotz, D., & West, R. (2009). Explaining the social gradient in smoking cessation: it’s not in the trying, but in the succeeding. Tobacco Control, 18(1), 43–46.
Kruger, D. J., Reischl, T., & Zimmerman, M. A. (2008). Time perspective as a mechanism for functional developmental adaptation. Journal of Social, Evolutionary and Cultural Psychology, 2(1), 1–22.
Krupp, D. B. (2012). Marital, reproductive, and educational behaviors covary with life expectancy. Archives of Sexual Behavior, 41(6), 1409–1414.
Lawson, D. W., & Mace, R. (2011). Parental investment and the optimization of human family size. Philosophical Transactions of the Royal Society, B: Biological Sciences, 366(1563), 333–343.
Layte, R., & Whelan, C. T. (2009). Explaining social class inequalities in smoking: the role of education, self-efficacy, and deprivation. European Sociological Review, 25(4), 399–410.
Li, J.-Z., Gui, D.-Y., Feng, C.-L., Wang, W.-Z., Du, B.-Q., Gan, T., & Luo, Y.-J. (2012). Victims’ time discounting 2.5 years after the Wenchuan earthquake: An ERP study. PloS One, 7(7), e40316.
Liao, Y., McGee, D. L., Kaufman, J. S., Cao, G., & Cooper, R. S. (1999). Socioeconomic status and morbidity in the last years of life. American Journal of Public Health, 89(4), 569–572.
Low, B. S., Hazel, A., Parker, N., & Welch, K. B. (2008). Influences on women’s reproductive lives: unexpected ecological underpinnings. Cross-Cultural Research, 42(3), 201–219.
McLaren, L. (2007). Socioeconomic status and obesity. Epidemiologic Reviews, 29, 29–48.
Medawar, P. B. (1952). An unsolved problem of biology. London: Lewis.
Melchior, M., Choquet, M., Le Strat, Y., Hassler, C., & Gorwood, P. (2011). Parental alcohol dependence, socioeconomic disadvantage and alcohol and cannabis dependence among young adults in the community. European Psychiatry, 26(1), 13–17.
Mirotznik, J., Feldman, L., & Stein, R. (1995). The health belief model and adherence with a community center-based, supervised coronary heart disease exercise program. Journal of Community Health, 20(3), 233–247.
Mirotznik, J., Ginzler, E., Zagon, G., & Baptiste, A. (1998). Using the health belief model to explain clinic appointment-keeping for the management of a chronic disease condition. Journal of Community Health, 23(3), 195–210.
Mokdad, A. H., Marks, J. S., Stroup, D. F., & Gerberding, J. L. (2004). Actual causes of death in the United States. Journal of the American Medical Association, 291(10), 1238–1245.
Moore, J., Stinson, L. L., & Welniak, E. J. (2000). Income measurement error in surveys: A review. Journal of Official Statistics, (June), 1–34
Nettle, D. (2010). Why are there social gradients in preventative health behavior? A perspective from behavioral ecology. PloS One, 5(10), 6.
Nettle, D. (2011). Flexibility in reproductive timing in human females: integrating ultimate and proximate explanations. Philosophical Transactions of the Royal Society of London, B: Biological Sciences, 366(1563), 357–365.
Nettle, D., Coall, D. A., & Dickins, T. E. (2011). Early-life conditions and age at first pregnancy in British women. Proceedings of the Royal Society B: Biological Sciences, 278, 1721–1727.
Pampel, F. C., Krueger, P., & Denney, J. (2010). Socioeconomic disparities in health behaviors. Annual Review of Sociology, 36, 349–370.
Pepper, G. V., & Nettle, D. (2013). Death and the time of your life: experiences of close bereavement are associated with steeper financial future discounting and earlier reproduction. Evolution and Human Behavior, 34(6), 434–439.
Pepper, G. V., & Nettle, D. (2014). Socioeconomic disparities in health behaviour: An evolutionary perspective. In D. W. Lawson & M. Gibson (Eds.), Applied evolutionary anthropology: Darwinian approaches to contemporary world issues (pp. 225–244). New York: Springer.
Phelan, J. C., Link, B. G., & Tehranifar, P. (2010). Social conditions as fundamental causes of health inequalities: theory, evidence, and policy implications. Journal of Health and Social Behavior, 51(suppl), S28–S40.
Preacher, K. J., & Hayes, A. F. (2004). SPSS and SAS procedures for estimating indirect effects in simple mediation models. Behavior Research Methods, Instruments, & Computers, 36(4), 717–731.
Pridemore, W. A., Tomkins, S., Eckhardt, K., Kiryanov, N., & Saburova, L. (2010). A case–control analysis of socio-economic and marital status differentials in alcohol- and non-alcohol-related mortality among working-age Russian males. European Journal of Public Health, 20(5), 569–575.
Quinlan, R. J. (2010). Extrinsic mortality effects on reproductive strategies in a Caribbean community. Human Nature, 21(2), 124–139.
Ramos, D., Victor, T., Seidl-de-Moura, M. L., & Daly, M. (2013). Future discounting by slum-dwelling youth versus university students in Rio de Janeiro. Journal of Research on Adolescence, 23(1), 95–102.
Siahpush, M., McNeill, A., Hammond, D., & Fong, G. T. (2006). Socioeconomic and country variations in knowledge of health risks of tobacco smoking and toxic constituents of smoke: results from the 2002 International Tobacco Control (ITC) Four Country Survey. Tobacco Control, 15(Suppl. 3), 65–70.
Soskolne, V., & Mano, O. (2010). Health inequalities in Israel: Explanatory factors of socio-economic inequalities in self-rated health and limiting longstanding illness. Health & Place, 16(2), 242–251.
Stafford, M., Chandola, T., & Marmot, M. (2007). Association between fear of crime and mental health and physical functioning. American Journal of Public Health, 97(11), 2076–2081.
Stearns, S. C. (1992). The evolution of life histories. Oxford: Oxford University Press.
Stringhini, S., Sabia, S., Shipley, M., Brunner, E., Nabi, H., Kivimaki, M., & Singh-Manoux, A. (2010). Association of socioeconomic position with health behaviors and mortality. Journal of the American Medical Association, 303(12), 1159–1166.
Stroebe, M., Schut, H., & Stroebe, W. (2007). Health outcomes of bereavement. Lancet, 370(9603), 1960–1973.
Wardle, J., & Steptoe, A. (2003). Socioeconomic differences in attitudes and beliefs about healthy lifestyles. Journal of Epidemiology and Community Health, 57(6), 440–443.
Wardle, J., Waller, J., & Jarvis, M. J. (2002). Sex differences in the association of socioeconomic status with obesity. American Journal of Public Health, 92(8), 1299–1304.
White, M., Adams, J., & Heywood, P. (2009). How and why do interventions that increase health overall widen inequalities within populations? In S. J. Babones (Ed.), Social inequality and public health (pp. 65–81). Bristol: The Policy Press.
Wilkinson, R. G. (1992). Income distribution and life expectancy. British Medical Journal, 304, 165–168.
Williams, G. C. (1957). Pleiotropy, natural selection, and the evolution of senescence. Evolution, 11(December), 398–411.
Wilson, M., & Daly, M. (1997). Life expectancy, economic inequality, homicide, and reproductive timing in Chicago neighbourhoods. British Medical Journal, 314(7089), 1271–1274.
Winkler, E., Turrell, G., & Patterson, C. (2006). Does living in a disadvantaged area mean fewer opportunities to purchase fresh fruit and vegetables in the area? Findings from the Brisbane food study. Health & Place, 12(3), 306–319.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(XLS 100 kb)
Rights and permissions
About this article
Cite this article
Pepper, G.V., Nettle, D. Perceived Extrinsic Mortality Risk and Reported Effort in Looking after Health. Hum Nat 25, 378–392 (2014). https://doi.org/10.1007/s12110-014-9204-5
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12110-014-9204-5