Abstract
Purpose
For the rational design of nanovaccines against respiratory pathogens, careful selection of optimal particle size and chemistry is paramount. This work investigates the impact of these properties on the deposition, biodistribution, and cellular interactions of nanoparticles within the lungs.
Method
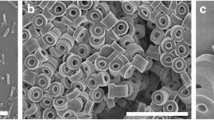
In this work, biodegradable poly(sebacic anhydride) (poly(SA)) nanoparticles of multiple sizes were synthesized with narrow particle size distributions. The lung deposition and retention as well as the internalization by phagocytic cells of these particles were compared to that of non-degradable monodisperse polystyrene nanoparticles of similar sizes.
Results
The initial deposition of intranasally administered particles in the lungs was dependent on primary particle size, with maximal deposition occurring for the 360–470 nm particles, regardless of chemistry. Over time, both particle size and chemistry affected the frequency of particle-positive cells and the specific cell types taking up particles. The biodegradable poly(SA) particles associated more closely with phagocytic cells and the dynamics of this association impacted the clearance of these particles from the lung.
Conclusions
The findings reported herein indicate that both size and chemistry control the fate of intranasally administered particles and that the dynamics of particle association with phagocytic cells in the lungs provide important insights for the rational design of pulmonary vaccine delivery vehicles.







Similar content being viewed by others
Abbreviations
- APC:
-
Antigen presenting cell
- DC:
-
Dendritic cell
- H&E:
-
Hematoxylin and eosin
- MFI:
-
Mean fluorescence intensity
- MΦ:
-
Macrophage
- PMN:
-
Polymorphonuclear leukocyte
- poly(SA):
-
Poly(sebacic anhydride)
- PS:
-
Polystyrene
References
Buxton DB. Nanotechnology in the diagnosis and management of heart, lung and blood diseases. Expert Rev Mol Diagn. 2007;7:149–60.
Kumari A, Yadav SK, Yadav SC. Biodegradable polymeric nanoparticles based drug delivery systems. Colloids Surf B. 2010;75(1):1–18.
McNeela EA, Lavelle EC. Recent advances in microparticle and nanoparticle delivery vehicles for mucosal vaccination. Curr Top Microbiol Immunol. 2012;354:75–99.
Park E-S, Maniar M, Shah JC. Biodegradable polyanhydride devices of cefazolin sodium, bupivacaine, and taxol for local drug delivery: preparation, and kinetics and mechanism of in vitro release. J Control Release. 1998;52(1–2):179–89.
Storm PB, Moriarity JL, Tyler B, Burger PC, Brem H, Weingart J. Polymer delivery of camptothecin against 9L gliosarcoma: release, distribution, and efficacy. J Neuro-Oncol. 2002;56:209–17.
Masters DB, Berde CB, Dutta S, Turek T, Langer R. Sustained local anesthetic release from bioerodible polymer matrices: a potential method for prolonged regional anesthesia. Pharm Res. 1993;10(10):1527–32.
Carino GP, Jacob JS, Mathiowitz E. Nanosphere based oral insulin delivery. J Control Release. 2000;65(1–2):261–9.
Erdmann L, Uhrich KE. Synthesis and degradation characteristics of salicylic acid-derived poly(anhydride-esters). Biomaterials. 2000;21:1941–6.
Deng J-S, Meisters M, Li L, Setesak J, Claycomb L, Tian Y, et al. The development of an injection-molding process for a polyanhydride implant containing gentamicin sulfate. PDA J Pharm Sci Technol. 2002;56(2):65–77.
Weiner AA, Bock EA, Gipson ME, Shastri VP. Photocrosslinked anhydride systems for long-term protein release. Biomaterials. 2008;29(15):2400–7.
Fv B, Schedl L, Göpferich A. Why degradable polymers undergo surface erosion or bulk erosion. Biomaterials. 2002;23(21):4221–31.
Balasse E, Odot J, Gatouillat G, Andry M-C, Madoulet C. Enhanced Immune response induced by bsa loaded in hydroxyethylstarch microparticles. Int J Pharm. 2008;353(1–2):131–8.
Huntimer L, Ramer-Tait AE, Petersen LK, Ross KA, Walz KA, Wang C, et al. Evaluation of biocompatiblity and administration site reactogenicity of polyanhydride-particle-based platform for vaccine delivery. Adv Healthc Mater. 2013;2:369–78.
Kuehl PJ, Anderson TL, Candelaria G, Gershman B, Harlin K, Hesterman JY, et al. Regional particle size dependent deposition of inhaled aerosols in rats and mice. Inhal Toxicol. 2012;24(1):27–35.
Champion JA, Walker A, Mitragotri S. Role of particle size in phagocytosis of polymeric microspheres. Pharm Res. 2008;25(8):1815–21.
Chiang P-C, Alsup J, Lai Y, Hu Y, Heyde B, Tung D. Evaluation of aerosol delivery of nanosuspension for Pre-clinical pulmonary drug delivery. Nanoscale Res Lett. 2009;4(3):254–61.
Wang SH, Thompson AL, Hickey AJ, Staats HF. Dry powder vaccines for mucosal administration: critical factors in manufacture and delivery. Curr Top Microbiol Immunol. 2012;354:121–56.
Wilson-Welder JH, Torres MP, Kipper MJ, Mallapragada SK, Wannemuehler MJ, Narasimhan B. Vaccine adjuvants: current challenges and future approaches. J Pharm Sci. 2009;98(4):1278–316.
Ulery BD, Phanse Y, Sinha A, Wannemuehler MJ, Narasimhan B, Bellaire BH. Polymer chemistry influences monocytic uptake of polyanhydride nanospheres. Pharm Res. 2009;26(3):683–90.
Champion JA, Mitragotri S. Shape induced inhibition of phagocytosis of polymer particles. Pharm Res. 2009;26(1):244–9.
Petersen LK, Xue L, Wannemuehler MJ, Rajan K, Narasimhan B. The simultaneous effect of polymer chemistry and device geometry on the in vitro activation of murine dendritic cells. Biomaterials. 2009;30(28):5131–42.
Ulery BD, Petersen LK, Phanse Y, Kong CS, Broderick SR, Kumar D, et al. Rational design of pathogen-mimicking amphiphilic materials as nanoadjuvants. Sci Rep. 2011;1:1–9.
Ulery BD, Kumar D, Ramer-Tait AE, Metzger DW, Wannemuehler MJ, Narasimhan B. Design of a protective single-dose intranasal nanoparticle-based vaccine platform for respiratory infectious diseases. PLoS One. 2011;6(3):e17642.
Jani PU, Florence AT, McCarthy DE. Further histological evidence of the gastrointestinal absorption of polystyrene nanospheres in the Rat. Int J Pharm. 1992;84:245–52.
Brooking J, Davis SS, Illum L. Transport of nanoparticles across the rat nasal mucosa. J Drug Target. 2001;9:267–79.
Kipper MJ, Shen E, Determan A, Narasimhan B. Design of an injectable system based on bioerodible polyanhydride microspheres for sustained drug delivery. Biomaterials. 2002;23(22):4405–12.
Shen E, Kipper MJ, Dziadul B, Lim M-K, Narasimhan B. Mechanistic relationships between polymer microstructure and drug release kinetics in bioerodible polyanhydrides. J Control Release. 2002;82(1):115–25.
Roberts JR, Antonini JM, Porter DW, Chapman RS, Scabilloni JF, Young S-H, et al. Lung toxicity and biodistribution of Cd/Se-ZnS quantum dots with different surface functional groups after pulmonary exposure in rats. Part Fibre Toxicol. 2013;10(5).
Determan AS, Trewyn BG, Lin VSY, Nilsen-Hamilton M, Narasimhan B. Encapsulation, stabilization, and release of BSA-FITC from polyanhydride microspheres. J Control Release. 2004;100(1):97–109.
Determan AS, Wilson JH, Kipper MJ, Wannemuehler MJ, Narasimhan B. Protein stability in the presence of polymer degradation products: consequences for controlled release formulations. Biomaterials. 2006;27(17):3312–20.
Determan AS, Graham JR, Pfeiffer KA, Narasimhan B. The role of microsphere fabrication methods on the stability and release kinetics of ovalbumin encapsulated in polyanhydride microspheres. J Microencapsul. 2006;23(8):832–43.
Torres MP, Vogel BM, Narasimhan B, Mallapragada SK. Synthesis and characterization of novel polyanhydrides with tailored erosion mechanisms. J Biomed Mater Res Part A. 2006;76A(1):102–10.
Ross KA, Haughney SL, Petersen LK, Boggiatto P, Wannemuehler MJ, Narasimhan B. Lung deposition and cellular uptake behavior of pathogen-mimicking nanovaccines in the first 48 hours. Adv Health Mater. 2014;3(7):1071–7.
Springer T, Galfré G, Secher DS, Milstein C. Mac-1: a macrophage differentiation antigen identified by monoclonal antibody. Eur J Immunol. 1979;9(4):301–6.
Springer TA, Dav:Gnon D, Ho M-K, Kurzinger K, Martz E, Sanchez-Madrid F. LFA-1 and Lyt-2,3, molecules associated with T lymphocyte-mediated killing; and Mac-1, an LFA-1 homologue associated with complement receptor Function1. Immunol Rev. 1982;68(1):171–96.
Metlay JP, Witmer-Pack MD, Agger R, Crowley MT, Lawless D, Steinman RM. The distinct leukocyte integrins of mouse spleen dendritic cells as identified with New hamster monoclonal antibodies. J Exp Med. 1990;171(5):1753–71.
Hirsch S, Gordon S. The Use and limitation of monoclonal antibodies against mononuclear phagocytes. Immunobiology. 1982;161:298–307.
Vermaelen K, Pauwels R. Accurate and simple discrimination of mouse pulmonary dendritic cell and macrophage populations by flow cytometry: methodology and new: insights. Cytom Part A. 2004;61A:170–7.
Matthews KE, Karabeg A, Roberts JM, Saeland S, Dekan G, Epstein MM, et al. Long-term deposition of inhaled antigen in lung resident CD11b-CD11c+ cells. Am J Respir Cell Mol Biol. 2007;36:435–41.
Marsh LM, Cakarova L, Kwapiszewska G, von Wulffen W, Herold S, Seeger W, et al. Surface expression of CD74 by type II alveolar epithelial cells: a potential mechanism for macrophage migration inhibitory factor-induced epithelial repair. Am J Physiol Lung Cell Mol Physiol. 2009;296(3):L442–52.
Patton JS, Brain JD, Davies LA, Fiegel J, Gumbleton M, Kim K-J, et al. The particle has landed - characterizing the fate of inhaled pharmaceuticals. J Aerosol Med Pulm Drug Deliv. 2010;23(S2):S-71–87.
Kirch J, Guenther M, Doshi N, Schaefer UF, Schneider M, Mitragotri S, et al. Mucociliary clearance of micro- and nanoparticles is independent of size, shape and charge—an ex vivo and in silico approach. J Control Release. 2012;159(1):128–34.
Blank F, Stumbles P, von Garnier C. Opportunities and challenges of the pulmonary route for vaccination. Expert Opin Drug Deliv. 2011;8(5):547–63.
Geiser M, Kreyling WG. Deposition and biokinetics of inhaled nanoparticles. Part Fibre Toxicol. 2010;7(2).
Blank F, Stumbles PA, Seydoux E, Holt PG, Fink A, Rothen-Rutishauser B, et al. Size-dependent uptake of particles by pulmonary APC populations and trafficking to regional lymph nodes. Am J Respir Cell Mol Biol. 2013;49(1):67–77.
von Garnier C, Filgueira L, Wikstrom M, Smith M, Thomas JA, Strickland DH, et al. Anatomical location determines the distribution and function of dendritic cells and other APCs in the respiratory tract. J Immunol. 2005;175(3):1609–18.
Misharin AV, Morales-Nebreda L, Mutlu GM, Budinger GRS, Perlman H. Flow cytometric analysis of the macrophages and dendritic cell subsets in the mouse lung. Am J Respir Cell Mol Biol. 2013;49:503–10.
Gonzalez-Juarrero M, Shim TS, Kipnis A, Junqueira-Kipnis AP, Orme IM. Dynamics of macrophage cell populations during murine pulmonary tuberculosis. J Immunol. 2003;171:3128–35.
Perrone LA, Plowden JK, García-Sastre A, Katz JM, Tumpey TM. H5N1 and 1918 pandemic influenza virus infection results in early and excessive infiltration of macrophages and neutrophils in the lungs of mice. PLoS Pathog. 2008;4(8):e1000115.
Nakano H, Yanagita M, Gunn MD. Cd11c+B220+Gr-1+ cells in mouse lymph nodes and spleen display characteristics of plasmacytoid dendritic cells. J Exp Med. 2001;194(8):1171–8.
Jakubzick C, Tacke F, Llodra J, van Rooijen N, Randolph GJ. Modulation of dendritic cell trafficking to and from the airways. J Immunol. 2006;176(6):3578–84.
Janssen WJ, Barthel L, Muldrow A, Oberley-Deegan RE, Kearns MT, Jakubzick C, et al. Fas determines differential fates of resident and recruited macrophages during resolution of acute lung injury. Am J Respir Crit Care Med. 2011;184:547–60.
Lambrecht BN, Hammad H. Lung dendritic cells in respiratory viral infection and asthma: from protection to immunopathology. Annu Rev Immunol. 2012;30:243–70.
Langlois RA, Legge KL. Plasmacytoid dendritic cells enhance mortality during lethal influenza infections by eliminating virus-specific CD8 T cells. J Immunol. 2010;184:4440–6.
Julia V, Hessel EM, Malherbe L, Glaichenhaus N, O’Garra A, Coffman RL. A restricted subset of dendritic cells captures airborne antigens and remains able to activate specific T cells long after antigen exposure. Immunity. 2002;16:271–83.
Rose CE, Lannigan JA, Kim P, Lee JJ, Fu SM, Sung SS. Murine lung eosinophil activation and chemokine production in allergic airway inflammation. Cell Mol Immunol. 2010;7(5):361–74.
Bosio CM, Goodyear AW, Dow SW. Early interaction of Yersinia pestis with APCs in the lung. J Immunol. 2005;175:6750–6.
Sackett CK, Narasimhan B. Mathematical modeling of polymer erosion: consequences for drug delivery. Int J Pharm. 2011;418:104–14.
Chavez-Santoscoy AV, Roychoudhury R, Pohl NLB, Wannemuehler MJ, Narasimhan B, Ramer-Tait AE. Tailoring the immune response by targeting C-type lectin receptors on alveolar macrophages using “pathogen-like” amphiphilic polyanhydride nanoparticles. Biomaterials. 2012;33:4762–72.
Acknowledgments
The authors wish to acknowledge funding from the ONR-MURI Award (NN00014-06-1-1176), the U.S. Army Medical Research and Materiel Command (Grant no. W81XWH-09-1-0386), and HRSA (Grant no. C76HF19578). The authors would also like to thank Shawn Rigby of the Iowa State Flow Cytometry Facility for his expertise in flow cytometry. BN acknowledges the Vlasta Klima Balloun Professorship in Chemical and Biological Engineering. The authors wish to thank Dr. Paola Boggiatto for useful discussions on the analysis of the flow cytometric data.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Supplemental Figure 1
Hemotoxilyn & eosin stained lung tissues were evaluated, blindly by a board-certified veterinary pathologist using a histopathological scoring system. Scores of 0–5 were assigned to five independent parameters: inflammatory infiltration, necrosis, edema, hemorrhage, and bronchus-associated lymphoid tissue hyperplasia. A score of zero indicated the parameter was absent and a score of five indicated that the parameter was diffuse and interrupted normal tissue architecture. The data are presented as the mean ± standard error of the mean of the combined scores of all five parameters. The asterisk (*) indicates statistical significance compared to lungs from mice that were administered saline (p < 0.05) at the same time point. Each treatment group at each time point consisted of slides sectioned from a total of four mice. (GIF 34 kb)
Supplemental Figure 2
Flow cytometry gating strategy utilized for identification of particle-positive cells. Gating sequence illustrated for mice intranasally administered either saline, 470 nm poly(SA), or 360 nm PS particles 12 h previously. After initial gating for viable cells in forward (FSC-A) and side (SSC-A) scatter plots (top plot), single cells were identified in dual forward scatter (FSC-A vs. FSC-H) plot (not shown). The viable single cells were determined as particle positive based on fluorescence intensity, demonstrated here in dot plots of particle fluorescence (y-axis) vs. forward scatter (FSC-A) (x-axis). From these dot plots, it is clear that the lungs of mice administered saline only had no particle-positive cells. In contrast, the lungs of mice administered the poly(SA) or polystyrene (PS) particles showed significant numbers of particle-positive cells which were further examined for cell type. (GIF 20 kb)
Rights and permissions
About this article
Cite this article
Brenza, T.M., Petersen, L.K., Zhang, Y. et al. Pulmonary Biodistribution and Cellular Uptake of Intranasally Administered Monodisperse Particles. Pharm Res 32, 1368–1382 (2015). https://doi.org/10.1007/s11095-014-1540-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-014-1540-y