Abstract
Purpose
Gabapentin exhibits saturable absorption kinetics, however, it remains unclear which transporters that are involved in the intestinal transport of gabapentin. Thus, the aim of the current study was to explore the mechanistic influence of transporters on the intestinal absorption of gabapentin by both in vivo and in vitro investigations
Methods
Pharmacokinetic parameters were determined following a range of intravenous (5–100 mg/kg) and oral doses (10–200 mg/kg) in rats. Transepithelial transport (50 μM–50 mM) and apical uptake of gabapentin (0.01–50 mM) were investigated in Caco-2 cells. The effect of co-application of the LAT-inhibitor, BCH, and the b0,+-substrate, L-lysine, on intestinal transport of gabapentin was evaluated in vivo and in vitro.
Results
Gabapentin showed dose-dependent oral absorption kinetics and dose-independent disposition kinetics. Co-application of BCH inhibited intestinal absorption in vivo and apical uptake in vitro, whereas no effect was observed following co-application of L-lysine.
Conclusions
The present study shows for the first time that BCH was capable of inhibiting intestinal absorption of gabapentin in vivo. Furthermore, in Caco-2 cell experiments BCH inhibited apical uptake of gabapentin. These findings may imply that a BCH-sensitive transport-system was involved in the apical and possibly the basolateral transport of gabapentin across the intestinal wall.






Similar content being viewed by others
Abbreviations
- GBP:
-
Gabapentin
- BBB:
-
Blood–brain barrier
- Leu:
-
L-Leucine
- Phe:
-
L-Phenylalanine
- Lys:
-
L-Lysine
- Arg:
-
L-Arginine
- CssC:
-
L-Cystine
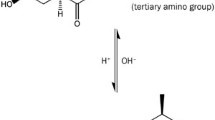
- BCH:
-
2-amino-2-norbornanecarboxylic acid
- (A-B):
-
Apical to basolateral
- (B-A):
-
Basolateral to apical
References
Bryans JS, Wustrow DJ. 3-Substituted GABA analogs with central nervous system activity: a review. Med Res Rev. 1999;19:149–77.
Taylor CP, Gee NS, Su TZ, Kocsis JD, Welty DF, Brown JP, et al. A summary of mechanistic hypotheses of gabapentin pharmacology. Epilepsy Res. 1998;29:233–49.
Farach FJ, Pruitt LD, Jun JJ, Jerud AB, Zoellner LA, Roy-Byrne PP. Pharmacological treatment of anxiety disorders: current treatments and future directions. J Anxiety Disord. 2012;26:833–43.
Kukkar A, Bali A, Singh N, Jaggi AS. Implications and mechanism of action of gabapentin in neuropathic pain. Arch Pharm Res. 2013;36:237–51.
Somerville ER, Michell AW. Gabapentin. In: Shorvon S, Perucca E, Engel J, editors. The treatment of epilepsy. Oxford: Wiley-Blackwell; 2009. p. 519–26.
Avdeef A. Absorption and drug development: solubility, permeability, and charge state. Hoboken: Wiley; 2003.
Stewart BH, Kugler AR, Thompson PR, Bockbrader HN. A saturable transport mechanism in the intestinal absorption of gabapentin is the underlying cause of the lack of proportionality between increasing dose and drug levels in plasma. Pharm Res. 1993;10:276–81.
Madan J, Chawla G, Arora V, Malik R, Bansal AK. Unbiased membrane permeability parameters for gabapentin using boundary layer approach. AAPS J. 2005;7:224–30.
Gidal BE, DeCerce J, Bockbrader HN, Gonzalez J, Kruger S, Pitterle ME, et al. Gabapentin bioavailability: effect of dose and frequency of administration in adult patients with epilepsy. Epilepsy Res. 1998;31:91–9.
Moore RA, Wiffen PJ, Derry S, McQuay HJ. Gabapentin for chronic neuropathic pain and fibromyalgia in adults. Cochrane Database Syst Rev. 2011:1–91.
Luer MS, Hamani C, Dujovny M, Gidal B, Cwik M, Deyo K, et al. Saturable transport of gabapentin at the blood–brain barrier. Neurol Res. 1999;21:559–62.
Radulovic LL, Türck D, von Hodenberg A, Vollmer KO, McNally WP, DeHart PD, et al. Disposition of gabapentin (neurontin) in mice, rats, dogs, and monkeys. Drug Metab Dispos. 1995;23:441–8.
Vollmer KO, von Hodenberg A, Kölle EU. Pharmacokinetics and metabolism of gabapentin in rat, dog and man. Arzneimittelforschung. 1986;36:830–9.
Cundy KC, Annamalai T, Bu L, De Vera J, Estrela J, Luo W, et al. XP13512 [(±)-1-([(α-Isobutanoyloxyethoxy)carbonyl] aminomethyl)-1-cyclohexane acetic acid], a novel gabapentin prodrug: II. Improved oral bioavailability, dose proportionality, and colonic absorption compared with gabapentin in rats and monkeys. J Pharmacol Exp Ther. 2004;311:324–33.
Urban TJ, Brown C, Castro RA, Shah N, Mercer R, Huang Y, et al. Effects of genetic variation in the novel organic cation transporter, OCTN1, on the renal clearance of gabapentin. Clin Pharmacol Ther. 2008;83:416–21.
Su TZ, Feng MR, Weber ML. Mediation of highly concentrative uptake of pregabalin by L-Type amino acid transport in chinese hamster ovary and Caco-2 cells. J Pharmacol Exp Ther. 2005;313:1406–15.
Naoki S, Nakanishi K, Wada M, Fujita T. Uptake and transport characteristics of gabapentin in human intestinal cell line caco-2. Drug Metab Rev. 2007;39:288–9.
Nguyen TV, Smith DE, Fleisher D. PEPT1 enhances the uptake of gabapentin via trans-stimulation of b0,+ exchange. Pharm Res. 2007;24:353–60.
Piyapolrungroj N, Li C, Bockbrader H, Liu G, Fleisher D. Mucosal uptake of gabapentin (neurontin) vs. pregabalin in the small intestine. Pharm Res. 2001;18:1126–30.
Fotiadis D, Kanai Y, Palacín M. The SLC3 and SLC7 families of amino acid transporters. Mol Aspects Med. 2013;34:139–58.
Rossier G, Meier C, Bauch C, Summa V, Sordat B, Verrey F, et al. LAT2, a new basolateral 4F2hc/CD98-associated amino acid transporter of kidney and intestine. J Biol Chem. 1999;274:34948–54.
Dave MH, Schulz N, Zecevic M, Wagner CA, Verrey F. Expression of heteromeric amino acid transporters along the murine intestine. J Physiol. 2004;558:597–610.
Larsen M, Larsen BB, Frølund B, Nielsen CU. Transport of amino acids and GABA analogues via the human proton-coupled amino acid transporter, hPAT1: Characterization of conditions for affinity and transport experiments in Caco-2 cells. Eur J Pharm Sci. 2008;35:86–95.
Frølund S, Langthaler L, Kall M, Holm R, Nielsen CU. Intestinal drug transport via the proton-coupled amino acid transporter, PAT1 (SLC36A1), is inhibited by Gly-Xaa dipeptides. Mol Pharm. 2012;9:2761–9.
Nielsen CU, Amstrup J, Steffansen B, Frokjaer S, Brodin B. Epidermal growth factor inhibits glycylsarcosine transport and hPepT1 expression in a human intestinal cell line. Am J Physiol Gastrointest Liver Physiol. 2001;281:G191–G9.
Frølund S, Marquez OC, Larsen M, Brodin B, Nielsen CU. delta-Aminolevulinic acid is a substrate for the amino acid transporter SLC36A1 (hPAT1). Br J Pharmacol. 2010;159:1339–53.
Park S, Kim JK, Kim IJ, Choi B, Jung KY, Lee S, et al. Reabsorption of neutral amino acids mediated by amino acid transporter LAT2 and TAT1 in the basolateral membrane of proximal tubule. Arch Pharm Res. 2005;28:421–32.
Bauch C, Forster N, Loffing-Cueni D, Summa V, Verrey F. Functional cooperation of epithelial heteromeric amino acid transporters expressed in Madin-Darby canine kidney cells. J Biol Chem. 2003;278:1316–22.
Mclean MJ. Gabapentin: chemistry, absorption, distribution, and elimination. In: Levy R, Mattson R, Meldrum B, editors. Antiepileptic drugs. New York: Raven; 1995. p. 843–9.
Jezyk N, Li C, Stewart BH, Wu X, Bockbrader HN, Fleisher D. Transport of pregabalin in rat intestine and Caco-2 monolayers. Pharm Res. 1999;16:519–26.
Cundy KC, Branch R, Chernov-Rogan T, Dias T, Estrada T, Hold K, et al. XP13512 [(±)-1-([(α-Isobutanoyloxyethoxy)carbonyl] aminomethyl)-1-cyclohexane acetic acid], a novel gabapentin prodrug: I. Design, synthesis, enzymatic conversion to gabapentin, and transport by intestinal solute transporters. J Pharmacol Exp Ther. 2004;311:315–23.
Mailliard ME, Stevens BR, Mann GE. Amino acid transport by small intestinal, hepatic, and pancreatic epithelia. Gastroenterology. 1995;108:888–910.
Kim CS, Cho S-H, Chun HS, Lee S-Y, Endou H, Kanai Y, et al. BCH, an Inhibitor of system L amino acid transporters, induces apoptosis in cancer cells. Biol Pharm Bull. 2008;31:1096–100.
Fraga S, Pinho MJ, Soares-da-Silva P. Expression of LAT1 and LAT2 amino acid transporters in human and rat intestinal epithelial cells. Amino Acids. 2005;29:229–33.
Fraga S, Serrão MP, Soares-da-Silva P. l-Type amino acid transporters in two intestinal epithelial cell lines function as exchangers with neutral amino acids. J Nutr. 2002;132:733–8.
Gidal BE, Radulovic LL, Kruger S, Rutecki P, Pitterle M, Bockbrader HN. Inter- and intra-subject variability in gabapentin absorption and absolute bioavailability. Epilepsy Res. 2000;40:123–7.
ACKNOWLEDGMENTS AND DISCLOSURES
The personnel at the animal facilities at H. Lundbeck A/S are acknowledged and appreciated for their skillful and flexible handling of the animal study. The cell culture facility at Department of Pharmacy is acknowledged for culturing cells.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(PDF 418 kb)
Rights and permissions
About this article
Cite this article
Larsen, M.S., Frølund, S., Nøhr, M.K. et al. In vivo and In vitro Evaluations of Intestinal Gabapentin Absorption: Effect of Dose and Inhibitors on Carrier-Mediated Transport. Pharm Res 32, 898–909 (2015). https://doi.org/10.1007/s11095-014-1505-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s11095-014-1505-1