Abstract
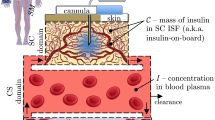
To shed light on how acute exercise affects blood glucose (BG) concentrations in nondiabetic subjects, we develop a physiological pharmacokinetic/pharmacodynamic model of postprandial glucose dynamics during exercise. We unify several concepts of exercise physiology to derive a multiscale model that includes three important effects of exercise on glucose dynamics: increased endogenous glucose production (EGP), increased glucose uptake in skeletal muscle (SM), and increased glucose delivery to SM by capillary recruitment (i.e. an increase in surface area and blood flow in capillary beds). We compare simulations to experimental observations taken in two cohorts of healthy nondiabetic subjects (resting subjects (n = 12) and exercising subjects (n = 12)) who were each given a mixed-meal tolerance test. Metabolic tracers were used to quantify the glucose flux. Simulations reasonably agree with postprandial measurements of BG concentration and EGP during exercise. Exercise-induced capillary recruitment is predicted to increase glucose transport to SM by 100%, causing hypoglycemia. When recruitment is blunted, as in those with capillary dysfunction, the opposite occurs and higher than expected BG levels are predicted. Model simulations show how three important exercise-induced phenomena interact, impacting BG concentrations. This model describes nondiabetic subjects, but it is a first step to a model that describes glucose dynamics during exercise in those with type 1 diabetes (T1D). Clinicians and engineers can use the insights gained from the model simulations to better understand the connection between exercise and glucose dynamics and ultimately help patients with T1D make more informed insulin dosing decisions around exercise.







Similar content being viewed by others
Change history
01 June 2021
A Correction to this paper has been published: https://doi.org/10.1007/s10928-021-09766-9
References
Wasserman DH (2009) Four grams of glucose. Am J Physiol Endocrinol Metab 296(1):E11–21. https://doi.org/10.1152/ajpendo.90563.2008
DeFronzo RA, Ferrannini E, Sato Y, Felig P, Wahren J (1981) Synergistic interaction between exercise and insulin on peripheral glucose uptake. J Clin Investig 68(6):1468–1474
Aarnio P, Lauritsen T, Dela F (2001) Insulin secretion and glucose kinetics during exercise with and without pharmacological \(a\)1- and \(a\)2-receptor blockade. Diabetes 50(8):1834–1843. https://doi.org/10.2337/diabetes.50.8.1834
Marliss EB, Vranic M (2002) Intense exercise has unique effects on both insulin release and its roles in glucoregulation: implications for diabetes. Diabetes 51(suppl 1):S271–S283. https://doi.org/10.2337/diabetes.51.2007.S271
Bergman RN (1989) Toward physiological understanding of glucose tolerance. Minimal-model approach. Diabetes 38(12):1512–1527
Schaller S, Willman S, Lippert J, Schaupp L, Pieber T, Schuppert A, Eissing T (2013) A generic integrated physiologically based whole-body model of the glucose-insulin-glucagon regulatory system. CPT 2(8):40. https://doi.org/10.1038/psp.2013.40
Sorensen J (1985) A Physiologic Model of Glucose Metabolism in Man and Its use to Design and Assess Improved Insulin Therapies for Diabetes. PhD thesis, Massachusetts Institute of Technology
Dalla Man C, Rizza RA, Cobelli C (2007) Meal simulation model of the glucose-insulin system. IEEE Trans Bio-medical Eng 54(10):1740–1749. https://doi.org/10.1109/TBME.2007.893506
Dalla Man C, Caumo A, Cobelli C (2002) The oral glucose minimal model: estimation of insulin sensitivity from a meal test. IEEE Trans Bio-medical Eng 49(5):419–429. https://doi.org/10.1109/10.995680
Dalla Man C, Raimondo DM, Rizza RA, Cobelli C (2007) GIM, simulation software of meal glucose-insulin model. J Diabetes Sci Technol 1(3):323–330
Roy A, Parker RS (2007) Dynamic modeling of exercise effects on plasma glucose and insulin levels. J Diabetes Sci Technol 1(3):338–347
Breton MD (2008) Physical activity-the major unaccounted impediment to closed loop control. J Diabetes Sci Technol 2(1):169–174
Man CD, Breton MD, Cobelli C (2009) Physical activity into the meal glucose-insulin model of type 1 diabetes: In silico studies. J Diabetes Sci Technol 3(1):56–67
Lenart PJ, Parker RS (2002) Modeling exercise effects in type 1 diabetic patients. IFAC Proc Vol 35(1):247–252. https://doi.org/10.3182/20020721-6-ES-1901.01350
Kovatchev BP, Breton M, Man CD, Cobelli C (2009) In silico preclinical trials: a proof of concept in closed-loop control of type 1 diabetes. J Diabetes Sci Technol 3(1):44–55
Ahlborg G, Felig P (1982) Lactate and glucose exchange across the forearm, legs, and splanchnic bed during and after prolonged leg exercise. J Clin Investig 69(1):45–54
Ahlborg G, Felig P, Hagenfeldt L, Hendler R, Wahren J (1974) Substrate turnover during prolonged exercise in man. Splanchnic and leg metabolism of glucose, free fatty acids, and amino acids. J Clin Investig 53(4):1080–1090. https://doi.org/10.1172/JCI107645
Renkin EM, Hudlicka O, Sheehan RM (1966) Influence of metabolic vasodilatation on blood-tissue diffusion in skeletal muscle. Am J Physiol 211(1):87–98
Womack L, Peters D, Barrett EJ, Kaul S, Price W, Lindner JR (2009) Abnormal skeletal muscle capillary recruitment during exercise in patients with type 2 diabetes mellitus and microvascular complications. J Am Coll Cardiol 53(23):2175–2183. https://doi.org/10.1016/j.jacc.2009.02.042
Schiavon M, Hinshaw L, Mallad A, Dalla Man C, Sparacino G, Johnson M, Carter R, Basu R, Kudva Y, Cobelli C, Basu A (2013) Postprandial glucose fluxes and insulin sensitivity during exercise: a study in healthy individuals. Am J Physiol Endocrinol Metab 305(4):E557–566. https://doi.org/10.1152/ajpendo.00182.2013
Hinshaw L, Schiavon M, Mallad A, Man CD, Basu R, Bharucha AE, Cobelli C, Carter RE, Basu A, Kudva YC (2014) Effects of delayed gastric emptying on postprandial glucose kinetics, insulin sensitivity, and beta-cell function. Am J Physiol Endocrinol Metab 307(6):494. https://doi.org/10.1152/ajpendo.00199.2014
Richter EA, Hargreaves M (2013) Exercise, GLUT4, and skeletal muscle glucose uptake. Physiol Rev 93(3):993–1017. https://doi.org/10.1152/physrev.00038.2012
Ren JM, Semenkovich CF, Gulve EA, Gao J, Holloszy JO (1994) Exercise induces rapid increases in GLUT4 expression, glucose transport capacity, and insulin-stimulated glycogen storage in muscle. J Biol Chem 269(20):14396–14401
Rose AJ, Richter EA (2005) Skeletal muscle glucose uptake during exercise: how is it regulated? Physiology (Bethesda, Md) 20:260–270. https://doi.org/10.1152/physiol.00012.2005
Yki-Järvinen H, Young AA, Lamkin C, Foley JE (1987) Kinetics of glucose disposal in whole body and across the forearm in man. J Clin Investiga 79(6):1713–1719
Renkin EM (1977) Multiple pathways of capillary permeability. Circ Res 41(6):735–743. https://doi.org/10.1161/01.RES.41.6.735
Renkin EM (1985) B. W. Zweifach Award lecture. Regulation of the microcirculation. Microvasc Res 30(3):251–263
Renkin EM (1959) Transport of potassium-42 from blood to tissue in isolated mammalian skeletal muscles. Am J Physiol 197:1205–1210
Frank S, Jbaily A, Hinshaw L, Basu R, Basu A, Szeri AJ (2018) Modeling the acute effects of exercise on insulin kinetics in type 1 diabetes. J Pharmacokinet Pharmacodyn 45(6):829–845. https://doi.org/10.1007/s10928-018-9611-z
Basu R, Di Camillo B, Toffolo G, Basu A, Shah P, Vella A, Rizza R, Cobelli C (2003) Use of a novel triple-tracer approach to assess postprandial glucose metabolism. Am J Physiol Endocrinol Metab 284(1):55. https://doi.org/10.1152/ajpendo.00190.2001
Radziuk J, McDonald TJ, Rubenstein D, Dupre J (1978) Initial splanchnic extraction of ingested glucose in normal man. Metabolism 27(6):657–669. https://doi.org/10.1016/0026-0495(78)90003-3
DeFronzo RA, Ferrannini E, Alberti KGMM, Zimmet P, Alberti G (2015) International textbook of diabetes mellitus. Wiley, Hoboken
Ferrannini E, Wahren J, Felig P, DeFronzo RA (1980) The role of fractional glucose extraction in the regulation of splanchnic glucose metabolism in normal and diabetic man. Metabolism 29(1):28–35. https://doi.org/10.1016/0026-0495(80)90094-3
Castillo C, Bogardus C, Bergman R, Thuillez P, Lillioja S (1994) Interstitial insulin concentrations determine glucose uptake rates but not insulin resistance in lean and obese men. J Clin Investig 93(1):10–16
Nielsen B, Savard G, Richter E, Hargreaves M, Saltin B (1990) Muscle blood flow and muscle metabolism during exercise and heat stress. J Appl Physiol 69(3):1040–1046
Katz A, Broberg S, Sahlin K, Wahren J (1986) Leg glucose uptake during maximal dynamic exercise in humans. Am J Physiol Endocrinol Metab 251(1):E65–E70
Saltin B (1988) Capacity of blood flow delivery to exercising skeletal muscle in humans. The American journal of cardiology 62(8):30E–35E
Fournier RL (2011) Basic transport phenomena in biomedical engineering. CRC Press, Boca Raton
Gudbjörnsdóttir S, Sjöstrand M, Strindberg L, Wahren J, Lönnroth P (2003) Direct measurements of the permeability surface area for insulin and glucose in human skeletal muscle. J Clin Endocrinol Metab 88(10):4559–4564. https://doi.org/10.1210/jc.2003-030434
Gudbjornsdottir S, Sjostrand M, Strindberg L, Lonnroth P (2005) Decreased muscle capillary permeability surface area in type 2 diabetic subjects. J Clin Endocrinol Metab 90(2):1078–1082. https://doi.org/10.1210/jc.2004-0947
Williams LR, Leggett RW (1989) Reference values for resting blood flow to organs of man. Clin Phys Physiol Meas 10(3):187
Bergman RN, Yang YJ, Hope ID, Ader M (1990) The role of the transcapillary insulin transport in the efficiency of insulin action: studies with glucose clamps and the minimal model. Hormone Metab Res Suppl Series 24:49–56
Guyton A, Hall J (2006) Textbook of medical physiology, 11th edn. Elsevier Saunders, Amsterdam
Vincent MA, Clerk LH, Lindner JR, Price WJ, Jahn LA, Leong-Poi H, Barrett EJ (2006) Mixed meal and light exercise each recruit muscle capillaries in healthy humans. Am J Physiol Endocrinol Metab 290(6):E1191–1197. https://doi.org/10.1152/ajpendo.00497.2005
Richter EA (2010) Glucose utilization. Comprehensive physiology. Wiley, Hoboken
Felig P, Wahren J, Hendler R (1975) Influence of oral glucose ingestion on splanchnic glucose and gluconeogenic substrate metabolism in man. Diabetes 24(5):468–475. https://doi.org/10.2337/diab.24.5.468
Bergman RN, Ider YZ, Bowden CR, Cobelli C (1979) Quantitative estimation of insulin sensitivity. Am J Physiol 236(6):E667–677
Cobelli C, Dalla Man C, Toffolo G, Basu R, Vella A, Rizza R (2014) The oral minimal model method. Diabetes 63(4):1203–1213. https://doi.org/10.2337/db13-1198
Dalla Man C, Caumo A, Basu R, Rizza R, Toffolo G, Cobelli C (2004) Minimal model estimation of glucose absorption and insulin sensitivity from oral test: validation with a tracer method. Am J Physiol Endocrinol Metab 287(4):E637–643. https://doi.org/10.1152/ajpendo.00319.2003
Baron AD, Brechtel G, Wallace P, Edelman SV (1988) Rates and tissue sites of non-insulin- and insulin-mediated glucose uptake in humans. Am J Physiol 255(6 Pt 1):E769–774
Holmäng A, Mimura K, Lönnroth P (2002) Involuntary leg movements affect interstitial nutrient gradients and blood flow in rat skeletal muscle. J Appl Physiol 92(3):982–988. https://doi.org/10.1152/japplphysiol.01194.2000
Sjöstrand M, Holmäng A, Lönnroth P (1999) Measurement of interstitial insulin in human muscle. Am J Physiol Endocrinol Metab 276(1):E151–E154
Jansson PAE, Fowelin JP, Von Schenck HP, Smith UP, Lönnroth PN (1993) Measurement by microdialysis of the insulin concentration in subcutaneous interstitial fluid: importance of the endothelial barrier for insulin. Diabetes 42(10):1469–1473. https://doi.org/10.2337/diab.42.10.1469
Hasgall P, Di Gebbari F, Baumgartner C, Neufeld E, Gosselin M, Payne D, Klingenböck A, Kuster N (2015) IT’IS Database for thermal and electromagnetic parameters of biological tissues 3.0, https://doi.org/10.13099/VIP21000-03-0
Clark MG, Rattigan S, Barrett EJ, Vincent MA (2008) Point:Counterpoint: there is/is not capillary recruitment in active skeletal muscle during exercise. J Appl Physiol 104(3):889–891. https://doi.org/10.1152/japplphysiol.00779.2007
Dawson D, Vincent MA, Barrett EJ, Kaul S, Clark A, Leong-Poi H, Lindner JR (2002) Vascular recruitment in skeletal muscle during exercise and hyperinsulinemia assessed by contrast ultrasound. Am J Physiol Endocrinol Metab 282(3):E714–720. https://doi.org/10.1152/ajpendo.00373.2001
Coggins M, Lindner J, Rattigan S, Jahn L, Fasy E, Kaul S, Barrett E (2001) Physiologic hyperinsulinemia enhances human skeletal muscle perfusion by capillary recruitment. Diabetes 50(12):2682–2690
De Feo P, Perriello G, Ventura MM, Calcinaro F, Basta G, Lolli C, Cruciani C, Dell’Olio A, Santeusanio F, Brunetti P (1986) Studies on overnight insulin requirements and metabolic clearance rate of insulin in normal and diabetic man: relevance to the pathogenesis of the dawn phenomenon. Diabetologia 29(8):475–480
Thorsteinsson B, Fugleberg S, Binder C (1988) Insulin clearance from plasma in type i (insulin-dependent) diabetic patients: influence of glycaemic level. Pharmacol Toxicol 62(4):206–209. https://doi.org/10.1111/j.1600-0773.1988.tb01873.x
Thorsteinsson B, Fugleberg S, Feldt-Rasmussen B, Ellemann K, Andersen OO, Binder C (1987) Kinetic Models for insulin disappearance from plasma in type I diabetic patients. Pharmacol Toxicol 60(2):90–95. https://doi.org/10.1111/j.1600-0773.1987.tb01502.x
Acknowledgements
We thank C. Funke and J. Gomez for their help and insight into this work.
Author information
Authors and Affiliations
Corresponding author
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This work was supported by the National Science Foundation Graduate Research Fellowship Program (S.F.). Studies supported by NIH Grant Nos. DK 085516, DK 094331, and UL1-R000135 from the National Center for Advancing Translational Sciences.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Frank, S., Jbaily, A., Hinshaw, L. et al. Modeling the acute effects of exercise on glucose dynamics in healthy nondiabetic subjects. J Pharmacokinet Pharmacodyn 48, 225–239 (2021). https://doi.org/10.1007/s10928-020-09726-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10928-020-09726-9