Abstract
Background
Helicobacter pylori eradication is a challenge in penicillin allergy.
Aim
To assess the efficacy and safety of first-line and rescue treatments in patients allergic to penicillin.
Methods
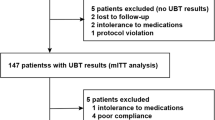
Prospective multicenter study. Patients allergic to penicillin were given a first-line treatment comprising (a) 7-day omeprazole–clarithromycin–metronidazole and (b) 10-day omeprazole–bismuth–tetracycline–metronidazole. Rescue treatments were as follows: (a) bismuth quadruple therapy; (b) 10-day PPI–clarithromycin–levofloxacin; and (c) 10-day PPI–clarithromycin–rifabutin. Eradication was confirmed by 13C-urea breath test. Compliance was determined through questioning and recovery of empty medication envelopes. Adverse effects were evaluated by questionnaires.
Results
In total, 267 consecutive treatments were included. (1) First-line treatment: Per-protocol and intention-to-treat eradication rates with omeprazole–clarithromycin–metronidazole were 59 % (62/105; 95 % CI 49–62 %) and 57 % (64/112; 95 % CI 47–67 %). Respective figures for PPI–bismuth–tetracycline–metronidazole were 75 % (37/49; 95 % CI 62–89 %) and 74 % (37/50; 95 % CI (61–87 %) (p < 0.05). Compliance with treatment was 94 and 98 %, respectively. Adverse events were reported in 14 % with both regimens (all mild). (2) Second-line treatment: Intention-to-treat eradication rate with omeprazole–clarithromycin–levofloxacin was 64 % both after triple and quadruple failure; compliance was 88–100 %, with 23–29 % adverse effects (all mild). (3) Third-/fourth-line treatment: Intention-to-treat eradication rate with PPI–clarithromycin–rifabutin was 22 %.
Conclusion
In allergic to penicillin patients, a first-line treatment with a bismuth-containing quadruple therapy (PPI–bismuth–tetracycline–metronidazole) seems to be a better option than the triple PPI–clarithromycin–metronidazole regimen. A levofloxacin-based regimen (together with a PPI and clarithromycin) represents a second-line rescue option in the presence of penicillin allergy.

Similar content being viewed by others
Abbreviations
- H. pylori :
-
Helicobacter pylori
- PPI:
-
Proton pump inhibitor
References
Malfertheiner P, Megraud F, O’Morain CA, et al. Management of Helicobacter pylori infection—the Maastricht IV/florence consensus report. Gut. 2012;61:646–664.
O’Connor A, Molina-Infante J, Gisbert JP, O’Morain C. Treatment of Helicobacter pylori infection 2013. Helicobacter. 2013;18:58–65.
Muranaka M, Okumura H, Takeda K, Koizumi K, Igarashi H. Population studies on drug hypersensitivities. Acta Allergol. 1973;28:50–61.
Gisbert JP, Calvet X, Bermejo F, et al. III Spanish consensus conference on Helicobacter pylori infection. Gastroenterol Hepatol. 2013;36:340–374.
Gisbert JP, Gisbert JL, Marcos S, Olivares D, Pajares JM. Helicobacter pylori first-line treatment and rescue options in patients allergic to penicillin. Aliment Pharmacol Ther. 2005;22:1041–1046.
Gisbert JP, Perez-Aisa A, Castro-Fernandez M, et al. Helicobacter pylori first-line treatment and rescue option containing levofloxacin in patients allergic to penicillin. Dig Liver Dis. 2010;42:287–290.
Gisbert JP, Badia X, Roset M, Pajares JM. The TETRA study: a prospective evaluation of Helicobacter pylori ‘test-and-treat’ strategy on 736 patients in clinical practice. Helicobacter. 2004;9:28–38.
Gisbert JP, Gonzalez L, Calvet X, et al. Proton pump inhibitor, clarithromycin and either amoxycillin or nitroimidazole: a meta-analysis of eradication of Helicobacter pylori. Aliment Pharmacol Ther. 2000;14:1319–1328.
Gisbert JP, Maria Pajares J. Helicobacter pylori resistance to metronidazole and to clarithromycin in Spain. A systematic review. Med Clin (Barc). 2001;116:111–116.
Megraud F, Coenen S, Versporten A, et al. Helicobacter pylori resistance to antibiotics in Europe and its relationship to antibiotic consumption. Gut. 2013;12:34–42.
Molina-Infante J, Gisbert JP. Update on the efficacy of triple therapy for Helicobacter pylori infection and clarithromycin resistance rates in Spain (2007–2012)]. Gastroenterol Hepatol. 2013;36:375–381.
Matsushima M, Suzuki T, Kurumada T, et al. Tetracycline, metronidazole and amoxicillin-metronidazole combinations in proton pump inhibitor-based triple therapies are equally effective as alternative therapies against Helicobacter pylori infection. J Gastroenterol Hepatol. 2006;21:232–236.
Rodriguez-Torres M, Salgado-Mercado R, Rios-Bedoya CF, et al. High eradication rates of Helicobacter pylori infection with first- and second-line combination of esomeprazole, tetracycline, and metronidazole in patients allergic to penicillin. Dig Dis Sci. 2005;50:634–639.
Fischbach L, Evans EL. Meta-analysis: the effect of antibiotic resistance status on the efficacy of triple and quadruple first-line therapies for Helicobacter pylori. Aliment Pharmacol Ther. 2007;26:343–357.
Malfertheiner P, Bazzoli F, Delchier JC, et al. Helicobacter pylori eradication with a capsule containing bismuth subcitrate potassium, metronidazole, and tetracycline given with omeprazole versus clarithromycin-based triple therapy: a randomised, open-label, non-inferiority, phase 3 trial. Lancet. 2011;377:905–913.
Gisbert JP. “Rescue” regimens after Helicobacter pylori treatment failure. World J Gastroenterol. 2008;14:5385–5402.
Gisbert JP, Pajares JM. Review article: Helicobacter pylori “rescue” regimen when proton pump inhibitor-based triple therapies fail. Aliment Pharmacol Ther. 2002;16:1047–1057.
Anderson VR, Perry CM. Levofloxacin : a review of its use as a high-dose, short-course treatment for bacterial infection. Drugs. 2008;68:535–565.
Sanchez JE, Saenz NG, Rincon MR, Martin IT, Sanchez EG, Martinez MJ. Susceptibility of Helicobacter pylori to mupirocin, oxazolidinones, quinupristin/dalfopristin and new quinolones. J Antimicrob Chemother. 2000;46:283–285.
Watanabe Y, Aoyama N, Shirasaka D, et al. Levofloxacin based triple therapy as a second-line treatment after failure of helicobacter pylori eradication with standard triple therapy. Dig Liver Dis. 2003;35:711–715.
Antos D, Schneider-Brachert W, Bastlein E, et al. 7-day triple therapy of Helicobacter pylori infection with levofloxacin, amoxicillin, and high-dose esomeprazole in patients with known antimicrobial sensitivity. Helicobacter. 2006;11:39–45.
Yahav J, Shmuely H, Niv Y, Bechor J, Samra Z. In vitro activity of levofloxacin against Helicobacter pylori isolates from patients after treatment failure. Diagn Microbiol Infect Dis. 2006;55:81–83.
Bilardi C, Dulbecco P, Zentilin P, et al. A 10-day levofloxacin-based therapy in patients with resistant Helicobacter pylori infection: a controlled trial. Clin Gastroenterol Hepatol. 2004;2:997–1002.
Gatta L, Zullo A, Perna F, et al. A 10-day levofloxacin-based triple therapy in patients who have failed two eradication courses. Aliment Pharmacol Ther. 2005;22:45–49.
Matsumoto Y, Miki I, Aoyama N, et al. Levofloxacin- versus metronidazole-based rescue therapy for H. pylori infection in Japan. Dig Liver Dis. 2005;37:821–825.
Saad RJ, Schoenfeld P, Kim HM, Chey WD. Levofloxacin-based triple therapy versus bismuth-based quadruple therapy for persistent Helicobacter pylori infection: a meta-analysis. Am J Gastroenterol. 2006;101:488–496.
Gisbert JP, Morena F. Systematic review and meta-analysis: levofloxacin-based rescue regimens after Helicobacter pylori treatment failure. Aliment Pharmacol Ther. 2006;23:35–44.
Li Y, Huang X, Yao L, Shi R, Zhang G. Advantages of Moxifloxacin and Levofloxacin-based triple therapy for second-line treatments of persistent Helicobacter pylori infection: a meta analysis. Wien Klin Wochenschr. 2010;122:413–422.
Marin AC, McNicholl AG, Gisbert JP. A review of rescue regimens after clarithromycin-containing triple therapy failure (for Helicobacter pylori eradication). Expert Opin Pharmacother. 2013;14:843–861.
Furuta T, Sugimoto M, Yamade M, et al. Eradication of H. pylori infection in patients allergic to penicillin using triple therapy with a PPI, metronidazole and sitafloxacin. Intern Med. 2014;53:571–575.
Murakami K, Okimoto T, Kodama M, et al. Sitafloxacin activity against Helicobacter pylori isolates, including those with gyrA mutations. Antimicrob Agents Chemother. 2009;53:3097–3099.
Croom KF, Goa KL. Levofloxacin: a review of its use in the treatment of bacterial infections in the United States. Drugs. 2003;63:2769–2802.
Gao W, Cheng H, Hu F, et al. The evolution of Helicobacter pylori antibiotics resistance over 10 years in Beijing, China. Helicobacter. 2010;15:460–466.
De Francesco V, Giorgio F, Hassan C, Manes G, Vannella L, Panella C et al. Worldwide H. pylori antibiotic resistance: a systematic review. J Gastrointestin Liver Dis. 2010;19:409–414.
Pérez-Trallero E, Ramírez-Lázaro MJ, Villar H, et al. Resistencia de Helicobacter pylori a diversos antibióticos: un estudio multicéntrico español. Gastroenterol Hepatol. 2011;34:236.
Gisbert JP, Calvet X. Review article: rifabutin in the treatment of refractory Helicobacter pylori infection. Aliment Pharmacol Ther. 2012;35:209–221.
Tay CY, Windsor HM, Thirriot F, et al. Helicobacter pylori eradication in Western Australia using novel quadruple therapy combinations. Aliment Pharmacol Ther. 2012;36:1076–1083.
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gisbert, J.P., Barrio, J., Modolell, I. et al. Helicobacter Pylori First-Line and Rescue Treatments in the Presence of Penicillin Allergy. Dig Dis Sci 60, 458–464 (2015). https://doi.org/10.1007/s10620-014-3365-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10620-014-3365-2