Abstract
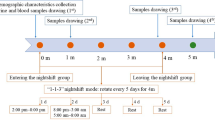
Epidemiologic studies indicate on an increased risk of cardiovascular disease and cancer in shift workers, although the underling mechanism is obscure. Heparanase directly enhances tissue factor (TF) activity leading to increased factor Xa production and subsequent activation of the coagulation system. In the present study, a comparison of coagulation markers among healthy shift working (SW) vs. healthy daytime working (DW) female nurses was performed. Thirty SW and 30 DW female nurses were enrolled. For each of the 60 participants, blood was drawn between 7:00 and 8:00 a.m. and at least 8 h after the last work shift. Plasma was studied for coagulation marker that included TF/heparanase procoagulant activity, TF activity, heparanase procoagulant activity, heparanase level, factor Xa level, plasminogen activator inhibitor 1 (PAI-1), plasminogen, α2-antiplasmin, fibrinogen, global protein C, von Willebrand factor, and D-dimer by chromogenic assays and enzyme-linked immunosorbent assays (ELISAs). Sleep quality was assessed by self-report according to the Pittsburgh Sleep Quality Index. The heparanase procoagulant activity increased by 2-fold and the TF/heparanase procoagulant activity increased by 1.5-fold in SW nurses compared to DW nurses (P < 0.05). Factor Xa levels and PAI-1 levels were significantly higher among SW nurses compared to the DW group (22 vs. 18 ng/ml, P < 0.05, and 32 vs. 22 ng/ml, P < 0.005, respectively). No significant differences were found in the other tested coagulation markers between the study groups. Heparanase procoagulant activity, factor Xa level, and PAI-1 level were significantly higher in SW nurses compared to the DW group. These alterations of blood coagulation activation may potentially contribute to cardiovascular and cancer morbidity.


Similar content being viewed by others
References
Wang XS, Armstrong ME, Cairns BJ, Key TJ, Travis RC (2011) Shift work and chronic disease: the epidemiological evidence. Occup Med (Lond) 61:78–89
Vyas MV, Garg AX, Iansavichus AV, Costella J, Donner A, Laugsand LE et al (2012) Shift work and vascular events: systematic review and meta-analysis. BMJ 345:e4800
Stevens RG, Brainard GC, Blask DE, Lockley SW, Motta ME (2014) Breast cancer and circadian disruption from electric lighting in the modern world. CA Cancer J Clin 64:207–218
Mazzoccoli G, Vinciguerra M, Papa G, Piepoli A (2014) Circadian clock circuitry in colorectal cancer. World J Gastroenterol 20:4197–4207
Knutsson A, Alfredsson L, Karlsson B, Akerstedt T, Fransson EI, Westerholm P et al (2013) Breast cancer among shift workers: results of the WOLF longitudinal cohort study. Scand J Work Environ Health 39:170–177
Varki A (2007) Trousseau’s syndrome: multiple definitions and multiple mechanisms. Blood 110:1723–1729
Rickles FR, Patierno S, Fernandez PM (2003) Tissue factor, thrombin, and cancer. Chest 124:58S–68S
Oishi K, Ohkura N (2013) Chronic circadian clock disruption induces expression of the cardiovascular risk factor plasminogen activator inhibitor-1 in mice. Blood Coagul Fibrinolysis 24:106–108
Meade TW, Chakrabarti R, North WR (1977) Associations between fibrinolytic activity and other variables in an industrial population. Adv Exp Med Biol 82:219–221
Freeman C, Parish CR (1998) Human platelet heparanase: purification, characterization and catalytic activity. Biochem J 330(Pt 3):1341–1350
Pikas DS, Li JP, Vlodavsky I, Lindahl U (1998) Substrate specificity of heparanases from human hepatoma and platelets. J Biol Chem 273:18770–18777
Parish CR, Freeman C, Hulett MD (2001) Heparanase: a key enzyme involved in cell invasion. Biochim Biophys Acta 1471:M99–M108
Vlodavsky I, Friedmann Y (2001) Molecular properties and involvement of heparanase in cancer metastasis and angiogenesis. J Clin Invest 108:341–347
Nadir Y, Brenner B, Zetser A, Ilan N, Shafat I, Zcharia E et al (2006) Heparanase induces tissue factor expression in vascular endothelial and cancer cells. J Thromb Haemost 4:2443–2451
Nadir Y, Brenner B, Gingis-Velitski S, Levy-Adam F, Ilan N, Zcharia E et al (2008) Heparanase induces tissue factor pathway inhibitor expression and extracellular accumulation in endothelial and tumor cells. Thromb Haemost 99:133–141
Nadir Y, Brenner B, Fux L, Shafat I, Attias J, Vlodavsky I (2010) Heparanase enhances the generation of activated factor X in the presence of tissue factor and activated factor VII. Haematologica 95:1927–1934
Nadir Y, Kenig Y, Drugan A, Shafat I, Brenner B (2011) An assay to evaluate heparanase procoagulant activity. Thromb Res 128:e3–e8
Peled E, Rovitsky A, Axelman E, Norman D, Brenner B, Nadir Y (2012) Increased heparanase level and procoagulant activity in orthopedic surgery patients receiving prophylactic dose of enoxaparin. Thromb Res 130:129–134
Matan M, Axelman E, Brenner B, Nadir Y (2013) Heparanase procoagulant activity is elevated in women using oral contraceptives. Hum Reprod 28:2372–2380
Nadir Y, Sarig G, Axelman E, Meir A, Wollner M, Shafat I et al (2014) Heparanase procoagulant activity is elevated and predicts survival in non-small cell lung cancer patients. Thromb Res 134:639–642
Zetser A, Levy-Adam F, Kaplan V, Gingis-Velitski S, Bashenko Y, Schubert S et al (2004) Processing and activation of latent heparanase occurs in lysosomes. J Cell Sci 117:2249–2258
Shafat I, Zcharia E, Nisman B, Nadir Y, Nakhoul F, Vlodavsky I et al (2006) An ELISA method for the detection and quantification of human heparanase. Biochem Biophys Res Commun 341:958–963
Andreotti F, Kluft C (1991) Circadian variation of fibrinolytic activity in blood. Chronobiol Int 8:336–351
Maemura K, de la Monte SM, Chin MT, Layne MD, Hsieh CM, Yet SF et al (2000) CLIF, a novel cycle-like factor, regulates the circadian oscillation of plasminogen activator inhibitor-1 gene expression. J Biol Chem 275:36847–36851
Mutch NJ, Wilson HM, Booth NA (2001) Plasminogen activator inhibitor-1 and haemostasis in obesity. Proc Nutr Soc 60:341–347
Eren M, Painter CA, Gleaves LA, Schoenhard JA, Atkinson JB, Brown NJ et al (2003) Tissue- and agonist-specific regulation of human and murine plasminogen activator inhibitor-1 promoters in transgenic mice. J Thromb Haemost 1:2389–2396
Skurk T, Hauner H (2004) Obesity and impaired fibrinolysis: role of adipose production of plasminogen activator inhibitor-1. Int J Obes Relat Metab Disord 28:1357–1364
Mertens I, Van der Planken M, Corthouts B, Wauters M, Peiffer F, De Leeuw I et al (2001) Visceral fat is a determinant of PAI-1 activity in diabetic and non-diabetic overweight and obese women. Horm Metab Res 33:602–607
Esterson YB, Kishore P, Koppaka S, Li W, Zhang K, Tonelli J et al (2012) Fatty acid-induced production of plasminogen activator inhibitor-1 by adipose macrophages is greater in middle-aged versus younger adult participants. J Gerontol A Biol Sci Med Sci 67:1321–1328
Buysse DJ, Reynolds CF 3rd, Monk TH, Berman SR, Kupfer DJ (1989) The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res 28:193–213
Shochat T, Tzischinsky O, Oksenberg A, Peled R (2007) Validation of the Pittsburgh Sleep Quality Index Hebrew translation (PSQI-H) in a sleep clinic sample. Isr Med Assoc J 9:853–856
Strike PC, Magid K, Whitehead DL, Brydon L, Bhattacharyya MR, Steptoe A (2006) Pathophysiological processes underlying emotional triggering of acute cardiac events. Proc Natl Acad Sci U S A 103:4322–4327
Jiang Q, Gingles NA, Olivier MA, Miles LA, Parmer RJ (2011) The anti-fibrinolytic SERPIN, plasminogen activator inhibitor 1 (PAI-1), is targeted to and released from catecholamine storage vesicles. Blood 117:7155–7163
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Additional information
Informed consent was obtained from all the patients for being included in the study.
Rights and permissions
About this article
Cite this article
Nadir, Y., Saharov, G., Hoffman, R. et al. Heparanase procoagulant activity, factor Xa, and plasminogen activator inhibitor 1 are increased in shift work female nurses. Ann Hematol 94, 1213–1219 (2015). https://doi.org/10.1007/s00277-015-2345-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00277-015-2345-8