Abstract
Purpose
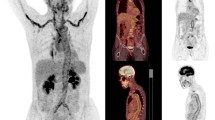
To estimate the diagnostic accuracy of conventional 18F-FDG PET/CT of cranial arteries in the diagnosis of giant cell arteritis (GCA).
Methods
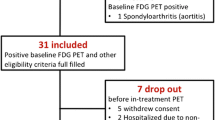
The study was a retrospective case-control study. The reference diagnosis was fulfillment of the 1990 ACR criteria for GCA. All patients had new-onset GCA. Conventional 18F-FDG PET/CT was performed before glucocorticoid treatment. Controls were age- and sex-matched patients with a previous history of malignant melanoma (MM) undergoing surveillance PET/CT >6 months after MM resection. PET images were evenly cropped to include only head and neck and were assessed in random order by four nuclear medicine physicians blinded to reference diagnosis. Temporal (TA), maxillary (MA) and vertebral (VA) arteries were visually rated for 18F-FDG uptake. Interreader agreement was evaluated by Fleiss kappa.
Results
A total of 44 patients and 44 controls were identified. In both groups, the mean age was 69 years (p = 0.45) and 25/44 were women. 35/41 GCA patients were temporal artery biopsy positive (TAB). Considering only FDG uptake in TA and/or MA, diagnostic sensitivity and specificity was 64 and 100%. Including VA, sensitivity increased to 82% and specificity remained 100%. Interreader agreement was 91% and Fleiss kappa 0.82 for the PET diagnosis based on the cranial arteries.
Conclusion
Conventional 18F-FDG PET/CT is an accurate and reliable tool to diagnose cranial arteritis in glucocorticoid-naïve GCA patients. The high diagnostic specificity suggests that TAB can be omitted in patients with 18F-FDG uptake in cranial arteries. 18F-FDG PET/CT performed in patients with suspected vasculitis should always include the head and neck.



Similar content being viewed by others
References
Ashton-Key MR, Gallagher PJ. False-negative temporal artery biopsy. Am J Surg Pathol. 1992;16:634.
Luqmani R, Lee E, Singh S, Gillett M, Schmidt WA, Bradburn M, et al. The role of ultrasound compared to biopsy of temporal arteries in the diagnosis and treatment of giant cell arteritis (TABUL): a diagnostic accuracy and cost-effectiveness study. Health Technol Assess (Rockv). 2016;20:1–270.
Mukhtyar C, Guillevin L, Cid MC, Dasgupta B, de Groot K, Gross W, et al. EULAR recommendations for the management of large vessel vasculitis. Ann Rheum Dis. 2009;68:318–23.
Bowling K, Rait J, Atkinson J, Srinivas G. Temporal artery biopsy in the diagnosis of giant cell arteritis: does the end justify the means? Ann Med Surg. 2017;20:1–5.
Dejaco C, Ramiro S, Duftner C, Besson FL, Bley TA, Blockmans D, et al. EULAR recommendations for the use of imaging in large vessel vasculitis in clinical practice. Ann Rheum Dis. 2018;77(5):636–43.
Treglia G, Mattoli MV, Leccisotti L, Ferraccioli G, Giordano A. Usefulness of whole-body fluorine-18-fluorodeoxyglucose positron emission tomography in patients with large-vessel vasculitis: a systematic review. Clin Rheumatol. 2011;30:1265–75.
Besson FL, Parienti J-J, Bienvenu B, Prior JO, Costo S, Bouvard G, et al. Diagnostic performance of 18F-fluorodeoxyglucose positron emission tomography in giant cell arteritis: a systematic review and meta-analysis. Eur J Nucl Med Mol Imaging. 2011;38:1764–72.
Soussan M, Nicolas P, Schramm C, Katsahian S, Pop G, Fain O, et al. Management of large-vessel vasculitis with FDG-PET. Medicine (Baltimore). 2015;94:e622.
Grayson PC, Alehashemi S, Bagheri AA, Civelek AC, Cupps TR, Kaplan MJ, et al. 18 F-Fluorodeoxyglucose-positron emission tomography as an imaging biomarker in a prospective, longitudinal cohort of patients with large vessel vasculitis. Arthritis Rheumatol. 2018;70:439–49.
Sammel AM, Hsiao E, Nguyen K, Schembri G, Laurent R. Maxillary artery 18F-FDG uptake as a new finding on PET/CT scan in a cohort of 41 patients suspected of having giant cell arteritis. Int J Rheum Dis. 2018;21:560–2.
Rehak Z, Szturz P, Kren L, Fojtik Z, Stanicek J. Upsampling from aorta and aortic branches: PET/CT hybrid imaging identified 18F-FDG hypermetabolism in inflamed temporal and occipital arteries. Clin Nucl Med. 2014;39:e84–6.
Maestri Brittain J, Gormsen L, von Benzon E, Andersen K. Concomitant polymyalgia rheumatica and large-vessel vasculitis visualized on 18F-FDG PET/CT. Diagnostics. 2018;8:27.
Hunder GG, Bloch DA, Michel BA, Stevens MB, Arend WP, Calabrese LH, et al. The American college of rheumatology 1990 criteria for the classification of giant cell arteritis. Arthritis Rheum. 1990;33:1122–8.
Nielsen BD, Gormsen LC, Hansen IT, Keller KK, Therkildsen P, Hauge E-M. Three days of high-dose glucocorticoid treatment attenuates large-vessel 18F-FDG uptake in large-vessel giant cell arteritis but with a limited impact on diagnostic accuracy. Eur J Nucl Med Mol Imaging. 2018;45:1119–28.
Boellaard R, Delgado-Bolton R, Oyen WJG, Giammarile F, Tatsch K, Eschner W, et al. FDG PET/CT: EANM procedure guidelines for tumour imaging: version 2.0. Eur J Nucl Med Mol Imaging. 2015;42:328–54.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42:377–81.
Sim J, Wright CC. The kappa statistic in reliability studies: use, interpretation, and sample size requirements. Phys Ther. 2005;85:257–68.
Brodmann M, Lipp RW, Passath A, Seinost G, Pabst E, Pilger E. The role of 2-18F-fluoro-2-deoxy-D-glucose positron emission tomography in the diagnosis of giant cell arteritis of the temporal arteries. Rheumatology. 2004;43:241–2.
Prieto-González S, Depetris M, García-Martínez A, Espígol-Frigolé G, Tavera-Bahillo I, Corbera-Bellata M, et al. Positron emission tomography assessment of large vessel inflammation in patients with newly diagnosed, biopsy-proven giant cell arteritis: a prospective, case–control study. Ann Rheum Dis. 2014;73:1388–92.
Förster S, Tato F, Weiss M, Czihal M, Rominger A, Bartenstein P, et al. Patterns of extracranial involvement in newly diagnosed giant cell arteritis assessed by physical examination, colour coded duplex sonography and FDG-PET. Vasa. 2011;40:219–27.
Lehmann P, Buchtala S, Achajew N, Haerle P, Ehrenstein B, Lighvani H, et al. 18F-FDG PET as a diagnostic procedure in large vessel vasculitis-a controlled, blinded re-examination of routine PET scans. Clin Rheumatol. 2011;30:37–42.
Henes JC, Müller M, Krieger J, Balletshofer B, Pfannenberg AC, Kanz L, et al. [18F] FDG-PET/CT as a new and sensitive imaging method for the diagnosis of large vessel vasculitis. Clin Exp Rheumatol. 2008;26:S47–52.
Pfadenhauer K, Weber H. Duplex sonography of the temporal and occipital artery in the diagnosis of temporal arteritis. A prospective study. J Rheumatol. 2003;30:2177–81.
Klink T, Geiger J, Both M, Ness T, Heinzelmann S, Reinhard M, et al. Giant cell arteritis: diagnostic accuracy of MR imaging of superficial cranial arteries in initial diagnosis—results from a multicenter trial. Radiology. 2014;273:844–52.
Rhéaume M, Rebello R, Pagnoux C, Carette S, Clements-Baker M, Cohen-Hallaleh V, et al. High-resolution magnetic resonance imaging of scalp arteries for the diagnosis of giant cell arteritis: results of a prospective cohort study. Arthritis Rheumatol. 2017;69:161–8.
Schmidt WA, Natusch A, Möller DE, Vorpahl K, Gromnica-Ihle E. Involvement of peripheral arteries in giant cell arteritis: a color Doppler sonography study. Clin Exp Rheumatol. 2002;20:309–18.
Ješe R, Rotar Ž, Tomšič M, Hočevar A. The role of colour doppler ultrasonography of facial and occipital arteries in patients with giant cell arteritis: a prospective study. Eur J Radiol. 2017;95:9–12.
Stone JH, Tuckwell K, Dimonaco S, Klearman M, Aringer M, Blockmans D, et al. Trial of tocilizumab in giant-cell arteritis. N Engl J Med. 2017;377:317–28.
Langford CA, Cuthbertson D, Ytterberg SR, Khalidi N, Monach PA, Carette S, et al. A randomized, double-blind trial of abatacept (CTLA-4Ig) for the treatment of giant cell arteritis. Arthritis Rheumatol. 2017;69:837–45.
Dejaco C, Brouwer E, Mason JC, Buttgereit F, Matteson EL, Dasgupta B. Giant cell arteritis and polymyalgia rheumatica: current challenges and opportunities. Nat Rev Rheumatol. 2017;13:1–15.
Meller J, Sahlmann CO, Gürocak O, Liersch T, Meller B. FDG-PET in patients with fever of unknown origin: the importance of diagnosing large vessel vasculitis. Q J Nucl Med Mol Imaging. 2009;53:51–63.
Muto G, Yamashita H, Takahashi Y, Miyata Y, Morooka M, Minamimoto R, et al. Large vessel vasculitis in elderly patients: early diagnosis and steroid-response evaluation with FDG-PET/CT and contrast-enhanced CT. Rheumatol Int. 2014;34:1545–54.
Fuchs M, Briel M, Daikeler T, Walker UA, Rasch H, Berg S, et al. The impact of 18F-FDG PET on the management of patients with suspected large vessel vasculitis. Eur J Nucl Med Mol Imaging. 2012;39:344–53.
Acknowledgements
This work was funded by The Danish Rheumatism Association, Aarhus University, Aarhus University Hospital, Brødrene Hartmann Fond, A.P. Moeller Foundation, and Aase & Ejnar Danielsen Foundation.
We would like to thank Irene Dalsgaard Nielsen, medical secretary, Department of Plastic and Breast surgery, Aarhus University Hospital for assisting the assessment of eligibility of the controls and Anne-Birgitte Blavnsfeldt, MD, Department of Rheumatology, Aarhus University Hospital for editing the manuscript.
Funding
This study was funded by The Danish Rheumatism Association, Aarhus University, Aarhus University Hospital, Brødrene Hartmann Foundation, A.P. Moeller Foundation, Aase & Ejnar Danielsen Foundation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethical approval
All procedures performed in the study were in accordance with the ethical standards of the National Committee on Health Research Ethics and with the 1964 Helsinki Declaration and its later amendments.
The Central Denmark Region Committees on Health Research Ethics (reference number 1–10–72-246-16 and 1–10–72-60-14) and The Danish Data Protection Agency (reference number 1–16–02-380-14 and 1–16–02-481-16) approved the study.
Informed consent
Ethical approval was given to assess 18F-FDG PET/CT of controls and to check prior and current diagnoses in their electronic medical record without informed consent from the patient. All GCA patients gave written, informed consent.
Conflicts of interests
Berit Dalsgaard Nielsen has received fees for speaking from Roche. Ellen-Margrethe Hauge has received fees for speaking from MSD, AbbVie, UCB and Sobi; and received research funding to Aarhus University Hospital from Roche and Novartis. Kresten Krarup Keller has received fees for speaking from Pfizer.
Disclaimers
The views expressed in the submitted article are the authors’ own and not an official position of the institution or funder.
Rights and permissions
About this article
Cite this article
Nielsen, B.D., Hansen, I.T., Kramer, S. et al. Simple dichotomous assessment of cranial artery inflammation by conventional 18F-FDG PET/CT shows high accuracy for the diagnosis of giant cell arteritis: a case-control study. Eur J Nucl Med Mol Imaging 46, 184–193 (2019). https://doi.org/10.1007/s00259-018-4106-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-018-4106-0