Abstract
Purpose
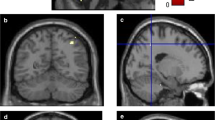
Cognitive impairment (CI) in Parkinson’s disease (PD) is associated with a widespread reduction in cortical glucose metabolism and relative increases in the cerebellum and brainstem as measured using 18F-fluorodesoxyglucose (FDG) PET. We separately analysed CI-related hypermetabolism and hypometabolism in comparison with neuropsychological test performance and investigated whether increased FDG uptake is a true feature of the disease or a normalization effect.
Methods
The study included 29 subjects (12 patients with PD, 10 patients with PD dementia and 7 healthy controls") who underwent FDG PET and comprehensive neuropsychological testing. Test performance across various cognitive domains was summarized in a cognitive staging score. Metabolic indices reflecting associated changes in regional cerebral glucose metabolism (rCGM) were calculated: index(−) for CI-related hypometabolism, and index(+) for CI-related hypermetabolism. We tested whether index(+) offered additional value in predicting the severity of CI in multiple regression analysis.
Results
At higher stages of CI, increased rCGM was found in the posterior cerebellar vermis and pons, associated with impaired attention, executive function and memory. Reduced rCGM was found in various cortical regions in agreement with the literature. In multiple regression analysis, both indices independently predicted the severity of CI with a whole-model R2 of 0.68 (index(−), p = 0.0006; index(+), p = 0.013), confirmed by alternative analyses combining different reference tissues in the multiple regression.
Conclusion
We found CI-related hypermetabolism in cerebellar regions that are known to be involved in several cognitive functions and in the pons. These alterations may represent compensatory activation of cognitive networks including cerebropontocerebellar tracts.


Similar content being viewed by others
References
Fereshtehnejad SM, Romenets SR, Anang JB, Latreille V, Gagnon JF, Postuma RB. New clinical subtypes of Parkinson disease and their longitudinal progression: a prospective cohort comparison with other phenotypes. JAMA Neurol. 2015;72(8):863–73. https://doi.org/10.1001/jamaneurol.2015.0703.
Kehagia AA, Barker RA, Robbins TW. Neuropsychological and clinical heterogeneity of cognitive impairment and dementia in patients with Parkinson’s disease. Lancet Neurol. 2010;9(12):1200–13. https://doi.org/10.1016/s1474-4422(10)70212-x.
Biundo R, Weis L, Antonini A. Cognitive decline in Parkinson’s disease: the complex picture. NPJ Parkinsons Dis. 2016;2:16018. https://doi.org/10.1038/npjparkd.2016.18.
Garcia-Garcia D, Clavero P, Gasca Salas C, Lamet I, Arbizu J, Gonzalez-Redondo R, et al. Posterior parietooccipital hypometabolism may differentiate mild cognitive impairment from dementia in Parkinson’s disease. Eur J Nucl Med Mol Imaging. 2012;39(11):1767–77. https://doi.org/10.1007/s00259-012-2198-5.
González-Redondo R, García-García D, Clavero P, Gasca-Salas C, García-Eulate R, Zubieta JL, et al. Grey matter hypometabolism and atrophy in Parkinson’s disease with cognitive impairment: a two-step process. Brain J Neurol. 2014;137(8):2356–67. https://doi.org/10.1093/brain/awu159.
Huang C, Mattis P, Perrine K, Brown N, Dhawan V, Eidelberg D. Metabolic abnormalities associated with mild cognitive impairment in Parkinson disease. Neurology. 2008;70(16 Pt 2):1470–7. https://doi.org/10.1212/01.wnl.0000304050.05332.9c.
Jokinen P, Scheinin N, Aalto S, Nagren K, Savisto N, Parkkola R, et al. [(11)C]PIB-, [(18)F]FDG-PET and MRI imaging in patients with Parkinson’s disease with and without dementia. Parkinsonism Relat Disord. 2010;16(10):666–70. https://doi.org/10.1016/j.parkreldis.2010.08.021.
Liepelt I, Reimold M, Maetzler W, Godau J, Reischl G, Gaenslen A, et al. Cortical hypometabolism assessed by a metabolic ratio in Parkinson’s disease primarily reflects cognitive deterioration-[18F]FDG-PET. Mov Disord. 2009;24(10):1504–11. https://doi.org/10.1002/mds.22662.
Meles SK, Tang CC, Teune LK, Dierckx RA, Dhawan V, Mattis PJ, et al. Abnormal metabolic pattern associated with cognitive impairment in Parkinson’s disease: a validation study. J Cereb Blood Flow Metab. 2015;35(9):1478–84. https://doi.org/10.1038/jcbfm.2015.112.
Bohnen NI, Koeppe RA, Minoshima S, Giordani B, Albin RL, Frey KA, et al. Cerebral glucose metabolic features of Parkinson disease and incident dementia: longitudinal study. J Nucl Med. 2011;52(6):848–55. https://doi.org/10.2967/jnumed.111.089946.
Eckert T, Tang C, Eidelberg D. Assessment of the progression of Parkinson’s disease: a metabolic network approach. Lancet Neurol. 2007;6(10):926–32. https://doi.org/10.1016/s1474-4422(07)70245-4.
Poston KL, Eidelberg D. Network biomarkers for the diagnosis and treatment of movement disorders. Neurobiol Dis. 2009;35(2):141–7. https://doi.org/10.1016/j.nbd.2008.09.026.
Borghammer P, Hansen SB, Eggers C, Chakravarty M, Vang K, Aanerud J, et al. Glucose metabolism in small subcortical structures in Parkinson’s disease. Acta Neurol Scand. 2012;125(5):303–10. https://doi.org/10.1111/j.1600-0404.2011.01556.x.
Ma Y, Tang C, Moeller JR, Eidelberg D. Abnormal regional brain function in Parkinson’s disease: truth or fiction? Neuroimage. 2009;45(2):260–6. https://doi.org/10.1016/j.neuroimage.2008.09.052.
Edison P, Ahmed I, Fan Z, Hinz R, Gelosa G, Ray Chaudhuri K, et al. Microglia, amyloid, and glucose metabolism in Parkinson’s disease with and without dementia. Neuropsychopharmacology. 2013;38(6):938–49. https://doi.org/10.1038/npp.2012.255.
Dubois B, Burn D, Goetz C, Aarsland D, Brown RG, Broe GA, et al. Diagnostic procedures for Parkinson’s disease dementia: recommendations from the Movement Disorder Society Task Force. Mov Disord. 2007;22(16):2314–24. https://doi.org/10.1002/mds.21844.
American Psychiatric Association. Diagnostic and statistical manual of mental disorders: DSM-IV. Washington DC: American Psychiatric Association; 1994.
Folstein MF, Folstein SE, McHugh PR. "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–98.
Cummings JL. The Neuropsychiatric Inventory: assessing psychopathology in dementia patients. Neurology. 1997;48(5 Suppl 6):S10–6.
Buckner RL, Krienen FM, Castellanos A, Diaz JC, Yeo BT. The organization of the human cerebellum estimated by intrinsic functional connectivity. J Neurophysiol. 2011;106(5):2322–45. https://doi.org/10.1152/jn.00339.2011.
Trošt M, Brezovar S, Tang CC, Eidelberg D, Zupančič Križnar N,Gregorič Kramberger M, et al. Metabolic brain changes related to specific cognitive impairment in non-demented Parkinson’s disease patients. Mov Disord. 2016;31(Suppl 2):S428.
Huang C, Mattis P, Tang C, Perrine K, Carbon M, Eidelberg D. Metabolic brain networks associated with cognitive function in Parkinson’s disease. Neuroimage. 2007;34(2):714–23. https://doi.org/10.1016/j.neuroimage.2006.09.003.
Keren-Happuch E, Chen S-HA, Ho M-HR, Desmond JE. A meta-analysis of cerebellar contributions to higher cognition from PET and fMRI studies. Hum Brain Mapp. 2014;35(2):593–615. https://doi.org/10.1002/hbm.22194.
Tang Y, Ge J, Liu F, Wu P, Guo S, Liu Z, et al. Cerebral metabolic differences associated with cognitive impairment in Parkinson’s disease. PLoS One. 2016;11(4):e0152716. https://doi.org/10.1371/journal.pone.0152716.
Tard C, Demailly F, Delval A, Semah F, Defebvre L, Dujardin K, et al. Hypometabolism in posterior and temporal areas of the brain is associated with cognitive decline in Parkinson’s disease. J Parkinsons Dis. 2015;5(3):569–74. https://doi.org/10.3233/JPD-150583.
Samson M, Claassen DO. Neurodegeneration and the cerebellum. Neurodegener Dis. 2017;17(4-5):155–65. https://doi.org/10.1159/000460818.
Wu T, Hallett M. The cerebellum in Parkinson’s disease. Brain. 2013;136(Pt 3):696–709. https://doi.org/10.1093/brain/aws360.
Mink JW. The basal ganglia: focused selection and inhibition of competing motor programs. Prog Neurobiol. 1996;50(4):381–425.
Salmi J, Pallesen KJ, Neuvonen T, Brattico E, Korvenoja A, Salonen O, et al. Cognitive and motor loops of the human cerebro-cerebellar system. J Cogn Neurosci. 2010;22(11):2663–76. https://doi.org/10.1162/jocn.2009.21382.
Caligiore D, Pezzulo G, Baldassarre G, Bostan AC, Strick PL, Doya K, et al. Consensus paper: towards a systems-level view of cerebellar function: the interplay between cerebellum, basal ganglia, and cortex. Cerebellum. 2017;16(1):203–29. https://doi.org/10.1007/s12311-016-0763-3.
Habas C, Kamdar N, Nguyen D, Prater K, Beckmann CF, Menon V, et al. Distinct cerebellar contributions to intrinsic connectivity networks. J Neurosci. 2009;29(26):8586–94. https://doi.org/10.1523/jneurosci.1868-09.2009.
van Eimeren T, Monchi O, Ballanger B, Strafella AP. Dysfunction of the default mode network in Parkinson disease: a functional magnetic resonance imaging study. Arch Neurol. 2009;66(7):877–83. https://doi.org/10.1001/archneurol.2009.97.
Disbrow EA, Carmichael O, He J, Lanni KE, Dressler EM, Zhang L, et al. Resting state functional connectivity is associated with cognitive dysfunction in non-demented people with Parkinson’s disease. J Parkinsons Dis. 2014;4(3):453–65. https://doi.org/10.3233/jpd-130341.
Simioni AC, Dagher A, Fellows LK. Compensatory striatal–cerebellar connectivity in mild–moderate Parkinson’s disease. Neuroimage Clin. 2016;10:54–62. https://doi.org/10.1016/j.nicl.2015.11.005.
Vo A, Sako W, Fujita K, Peng S, Mattis PJ, Skidmore FM, et al. Parkinson’s disease-related network topographies characterized with resting state functional MRI. Hum Brain Mapp. 2017;38(2):617–30. https://doi.org/10.1002/hbm.23260.
Wong K, Sidransky E, Verma A, Mixon T, Sandberg GD, Wakefield LK, et al. Neuropathology provides clues to the pathophysiology of Gaucher disease. Mol Genet Metab. 2004;82(3):192–207. https://doi.org/10.1016/j.ymgme.2004.04.011.
Yu H, Sternad D, Corcos DM, Vaillancourt DE. Role of hyperactive cerebellum and motor cortex in Parkinson’s disease. Neuroimage. 2007;35(1):222–33. https://doi.org/10.1016/j.neuroimage.2006.11.047.
Goerendt IK, Lawrence AD, Brooks DJ. Reward processing in health and Parkinson’s disease: neural organization and reorganization. Cereb Cortex. 2004;14(1):73–80.
Acknowledgments
We acknowledge the funding received from the European Community’s Seventh Framework Programme.
Funding
The research leading to these results received funding from the European Community’s Seventh Framework Programme (FP7/2007–2013) under grant agreement no. 603646 (MultISyn).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
None.
Ethical approval
All procedures performed in this study were in accordance with the principles of the 1964 Declaration of Helsinki and its later amendments and were approved by the local ethics committee.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Electronic supplementary material
ESM 1
Neuropsychological test battery: descriptive statistics for the four cognitive staging groups and results from correlation analysis (voxelwise multiple regression with two independent variables, i.e. the respective neuropsychological score and, as nuisance variable, UPDRSIII). CI = cognitive impairment (DOCX 25 kb)
Rights and permissions
About this article
Cite this article
Blum, D., la Fougère, C., Pilotto, A. et al. Hypermetabolism in the cerebellum and brainstem and cortical hypometabolism are independently associated with cognitive impairment in Parkinson’s disease. Eur J Nucl Med Mol Imaging 45, 2387–2395 (2018). https://doi.org/10.1007/s00259-018-4085-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-018-4085-1