Abstract
Aim
To assess the clinical utility of FDG-PET as a diagnostic aid for differentiating Alzheimer’s disease (AD; both typical and atypical forms), dementia with Lewy bodies (DLB), frontotemporal lobar degeneration (FTLD), vascular dementia (VaD) and non-degenerative pseudodementia.
Methods
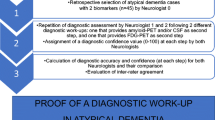
A comprehensive literature search was conducted using the PICO model to extract evidence from relevant studies. An expert panel then voted on six different diagnostic scenarios using the Delphi method.
Results
The level of empirical study evidence for the use of FDG-PET was considered good for the discrimination of DLB and AD; fair for discriminating FTLD from AD; poor for atypical AD; and lacking for discriminating DLB from FTLD, AD from VaD, and for pseudodementia. Delphi voting led to consensus in all scenarios within two iterations. Panellists supported the use of FDG-PET for all PICOs—including those where study evidence was poor or lacking—based on its negative predictive value and on the assistance it provides when typical patterns of hypometabolism for a given diagnosis are observed.
Conclusion
Although there is an overall lack of evidence on which to base strong recommendations, it was generally concluded that FDG-PET has a diagnostic role in all scenarios. Prospective studies targeting diagnostically uncertain patients for assessing the added value of FDG-PET would be highly desirable.


Similar content being viewed by others
References
Nobili F, Arbizu J, Bouwman F, Drzezga A, Filippi M, Nestor P, et al. EAN-EANM recommendations for the use of brain 18F-Fluorodeoxyglucose Positron Emission Tomography (FDG-PET) in neurodegenerative cognitive impairment and dementia: Delphi consensus. Eur J Neurol Eur J. 2018; being submitted.
Boccardi M, Festari C, Altomare D, Gandolfo F, Orini S, Nobili F, et al. Assessing accuracy diagnostic FDG-PET studies to define clinical use for dementia diagnosis. J Nucl Med Mol Imaging. 2018; In this Issue.
Leone MA, Brainin M, Boon P, Pugliatti M, Keindl M, Bassetti CL, et al. Guidance for the preparation of neurological management guidelines by EFNS scientific task forces - revised recommendations 2012. Eur J Neurol. 2013;20:410–9. https://doi.org/10.1111/ene.12043.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62:1006–12. https://doi.org/10.1016/j.jclinepi.2009.06.005.
Dubois B, Feldman HH, Jacova C, Cummings JL, Dekosky ST, Barberger-Gateau P, et al. Revising the definition of Alzheimer’s disease: a new lexicon. Lancet Neurol. 2010;9:1118–27. https://doi.org/10.1016/S1474-4422(10)70223-4.
McKhann GM, Knopman DS, Chertkow H, Hyman BT, Jack CR, Kawas CH, et al. The diagnosis of dementia due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7:263–9. https://doi.org/10.1016/j.jalz.2011.03.005.
Rascovsky K, Hodges JR, Knopman D, Mendez MF, Kramer JH, Neuhaus J, et al. Sensitivity of revised diagnostic criteria for the behavioural variant of frontotemporal dementia. Brain. 2011;134:2456–77. https://doi.org/10.1093/brain/awr179.
Neary D, Snowden JS, Gustafson L, Passant U, Stuss D, Black S, et al. Frontotemporal lobar degeneration: a consensus on clinical diagnostic criteria. Neurology. 1998;51:1546–54.
Albert MS, DeKosky ST, Dickson D, Dubois B, Feldman HH, Fox NC, et al. The diagnosis of mild cognitive impairment due to Alzheimer’s disease: recommendations from the National Institute on Aging-Alzheimer’s Association workgroups on diagnostic guidelines for Alzheimer’s disease. Alzheimers Dement. 2011;7:270–9. https://doi.org/10.1016/j.jalz.2011.03.008.
Dubois B, Feldman HH, Jacova C, Hampel H, Molinuevo JL, Blennow K, et al. Advancing research diagnostic criteria for Alzheimer’s disease: the IWG-2 criteria. Lancet Neurol. 2014;13:614–29. https://doi.org/10.1016/S1474-4422(14)70090-0.
Gorno-Tempini ML, Hillis AE, Weintraub S, Kertesz A, Mendez M, Cappa SF, et al. Classification of primary progressive aphasia and its variants. Neurology. 2011;76:1006–14. https://doi.org/10.1212/WNL.0b013e31821103e6.
Höglinger GU, Respondek G, Stamelou M, Kurz C, Josephs KA, Lang AE, et al. Clinical diagnosis of progressive supranuclear palsy: the movement disorder society criteria. Mov Disord. 2017;32:853–64. https://doi.org/10.1002/mds.26987.
McKeith IG, Boeve BF, Dickson DW, Halliday G, Taylor J-P, Weintraub D, et al. Diagnosis and management of dementia with Lewy bodies: fourth consensus report of the DLB consortium. Neurology. 2017;89:88–100. https://doi.org/10.1212/WNL.0000000000004058.
Dubois B, Feldman HH, Jacova C, DeKosky ST, Barberger-Gateau P, Cummings J, et al. Research criteria for the diagnosis of Alzheimer’s disease: revising the NINCDS–ADRDA criteria. Lancet Neurol. 2007;6:734–46. https://doi.org/10.1016/S1474-4422(07)70178-3.
Filippi M, Agosta F, Barkhof F, Dubois B, Fox NC, Frisoni GB, et al. EFNS task force: the use of neuroimaging in the diagnosis of dementia. Eur J Neurol. 2012;19:1487–501. https://doi.org/10.1111/j.1468-1331.2012.03859.x.
Bouwman F, Orini S, Gandolfo F, Altomare D, Festari C, Agosta F, et al. Diagnostic utility of FDG-PET in the differential diagnosis between different forms of primary progressive aphasia. J Nucl Med Mol Imaging. 2018. https://doi.org/10.1007/s00259-018-4034-z.
Drzezga A, Altomare D, Festari C, Arbizu J, Orini S, Herholz K, et al. Diagnostic utility of FDG-PET in conditions of increased risk for Alzheimer’s disease. Eur J Nucl Med Molec Imaging. 2018. https://doi.org/10.1007/s00259-018-4032-1.
Walker Z, Gandolfo F, Orini S, Garibotto V, Agosta F, Arbizu J, et al. Clinical utility of FDG-PET in Parkinson’s disease and atypical Parkinsonisms associated to dementia. Eur J Nucl Med Mol Imaging. 2018. https://doi.org/10.1007/s00259-018-4031-2.
Arbizu J, Festari C, Altomare D, Walker Z, Bouwman F, Rivolta J, et al. Clinical utility of FDG-PET for the differential diagnosis in MCI. Eur J Nucl Med Mol Imaging. 2018. 2018. https://doi.org/10.1007/s00259-018-4039-7.
Agosta F, Altomare D, Festari C, Orini S, Gandolfo F, Boccardi M, et al. Clinical utility of FDG-PET in amyotrophic lateral sclerosis and Huntington’s disease. Eur J Nucl Med Molec Imaging. 2018. https://doi.org/10.1007/s00259-018-4033-0.
Matias-Guiu JA, Cabrera-Martin MN, Moreno-Ramos T, Valles-Salgado M, Fernandez-Matarrubia M, Carreras JL, et al. Amyloid and FDG-PET study of logopenic primary progressive aphasia: evidence for the existence of two subtypes. J Neurol. 2015;262:1463–72. https://doi.org/10.1007/s00415-015-7738-z.
Schmidtke K, Hull M, Talazko J. Posterior cortical atrophy: variant of Alzheimer’s disease? A case series with PET findings. J Neurol. 2005;252:27–35. https://doi.org/10.1007/s00415-005-0594-5.
Whitwell JL, Lowe VJ, Duffy JR, Strand EA, Machulda MM, Kantarci K, et al. Elevated occipital beta-amyloid deposition is associated with widespread cognitive impairment in logopenic progressive aphasia. J Neurol Neurosurg Psychiatry. 2013;84:1357–64. https://doi.org/10.1136/jnnp-2013-305628.
Singh TD, Josephs KA, Machulda MM, Drubach DA, Apostolova LG, Lowe VJ, et al. Clinical, FDG and amyloid PET imaging in posterior cortical atrophy. J Neurol. 2015;262:1483–92. https://doi.org/10.1007/s00415-015-7732-5.
Cerami C, Della Rosa PA, Magnani G, Santangelo R, Marcone A, Cappa SF, et al. Brain metabolic maps in mild cognitive impairment predict heterogeneity of progression to dementia. NeuroImage Clin. 2015;7:187–94. https://doi.org/10.1016/j.nicl.2014.12.004.
Laforce R, Buteau JP, Paquet N, Verret L, Houde M, Bouchard RW. The value of PET in mild cognitive impairment, typical and atypical/unclear dementias: a retrospective memory clinic study. Am J Alzheimer’s Dis Other Demen. 2010;25:324–32. https://doi.org/10.1177/1533317510363468.
Laforce RJ, Tosun D, Ghosh P, Lehmann M, Madison CM, Weiner MW, et al. Parallel ICA of FDG-PET and PiB-PET in three conditions with underlying Alzheimer’s pathology. NeuroImage Clin. 2014;4:508–16. https://doi.org/10.1016/j.nicl.2014.03.005.
Madhavan A, Whitwell JL, Weigand SD, Duffy JR, Strand EA, Machulda MM, et al. FDG PET and MRI in logopenic primary progressive aphasia versus dementia of the Alzheimer’s type. PLoS One. 2013;8:e62471. https://doi.org/10.1371/journal.pone.0062471.
Spehl TS, Hellwig S, Amtage F, Weiller C, Bormann T, Weber WA, et al. Syndrome-specific patterns of regional cerebral glucose metabolism in posterior cortical atrophy in comparison to dementia with Lewy bodies and Alzheimer’s disease--a [F-18]-FDG pet study. J Neuroimaging. 2015;25:281–8. https://doi.org/10.1111/jon.12104.
Albin RL, Minoshima S, D’Amato CJ, Frey KA, Kuhl DA, Sima AA. Fluoro-deoxyglucose positron emission tomography in diffuse Lewy body disease. Neurology. 1996;47:462–6.
Garibotto V, Montandon ML, Viaud CT, Allaoua M, Assal F, Burkhard PR, et al. Regions of interest-based discriminant analysis of DaTSCAN SPECT and FDG-PET for the classification of dementia. Clin Nucl Med. 2013;38:e112–7. https://doi.org/10.1097/RLU.0b013e318279b991.
Imamura T, Ishii K, Hirono N, Hashimoto M, Tanimukai S, Kazuai H, et al. Visual hallucinations and regional cerebral metabolism in dementia with Lewy bodies (DLB). Neuroreport. 1999;10:1903–7.
Imamura T, Ishii K, Hirono N, Hashimoto M, Tanimukai S, Kazui H, et al. Occipital glucose metabolism in dementia with lewy bodies with and without parkinsonism: a study using positron emission tomography. Dement Geriatr Cogn Disord. 2001;12:194–7. https://doi.org/10.1159/000051257.
Teune LK, Bartels AL, de Jong BM, Willemsen ATM, Eshuis SA, de Vries JJ, et al. Typical cerebral metabolic patterns in neurodegenerative brain diseases. Mov Disord. 2010;25:2395–404. https://doi.org/10.1002/mds.23291.
Tripathi M, Dhawan V, Peng S, Kushwaha S, Batla A, Jaimini A, et al. Differential diagnosis of parkinsonian syndromes using F-18 fluorodeoxyglucose positron emission tomography. Neuroradiology. 2013;55:483–92. https://doi.org/10.1007/s00234-012-1132-7.
Perani D, Della Rosa PA, Cerami C, Gallivanone F, Fallanca F, Vanoli EG, et al. Validation of an optimized SPM procedure for FDG-PET in dementia diagnosis in a clinical setting. NeuroImage Clin. 2014;6:445–54. https://doi.org/10.1016/j.nicl.2014.10.009.
Ishii K, Hosokawa C, Hyodo T, Sakaguchi K, Usami K, Shimamoto K, et al. Regional glucose metabolic reduction in dementia with Lewy bodies is independent of amyloid deposition. Ann Nucl Med. 2015;29:78–83. https://doi.org/10.1007/s12149-014-0911-0.
Granert O, Drzezga AE, Boecker H, Perneczky R, Kurz A, Gotz J, et al. Metabolic topology of neurodegenerative disorders: influence of cognitive and motor deficits. J Nucl Med. 2015;56:1916–21. https://doi.org/10.2967/jnumed.115.156067.
Sharma R, Tripathi M, D’Souza MM, Jaimini A, Varshney R, Panwar P, et al. Spectrum of neurocognitive dysfunction in Indian population on FDG PET/CT imaging. Indian J Nucl Med. 2011;26:67–77. https://doi.org/10.4103/0972-3919.90255.
Kasanuki K, Iseki E, Fujishiro H, Yamamoto R, Higashi S, Minegishi M, et al. Neuropathological investigation of the hypometabolic regions on positron emission tomography with [18F] fluorodeoxyglucose in patients with dementia with Lewy bodies. J Neurol Sci. 2012;314:111–9. https://doi.org/10.1016/j.jns.2011.10.010.
Della Rosa PA, Cerami C, Gallivanone F, Prestia A, Caroli A, Castiglioni I, et al. A standardized [18F]-FDG-PET template for spatial normalization in statistical parametric mapping of dementia. Neuroinformatics. 2014;12:575–93. https://doi.org/10.1007/s12021-014-9235-4.
Chiba Y, Fujishiro H, Ota K, Kasanuki K, Arai H, Hirayasu Y, et al. Clinical profiles of dementia with Lewy bodies with and without Alzheimer’s disease-like hypometabolism. Int J Geriatr Psychiatry. 2015;30:316–23. https://doi.org/10.1002/gps.4144.
Imamura T, Ishii K, Sasaki M, Kitagaki H, Yamaji S, Hirono N, et al. Regional cerebral glucose metabolism in dementia with Lewy bodies and Alzheimer’s disease: a comparative study using positron emission tomography. Neurosci Lett. 1997;235:49–52.
Okamura N, Arai H, Higuchi M, Tashiro M, Matsui T, Hu XS, et al. [18F]FDG-PET study in dementia with Lewy bodies and Alzheimer’s disease. Prog Neuro-Psychopharmacol Biol Psychiatry. 2001;25:447–56.
Gilman S, Koeppe RA, Little R, An H, Junck L, Giordani B, et al. Differentiation of Alzheimer’s disease from dementia with Lewy bodies utilizing positron emission tomography with [18F]fluorodeoxyglucose and neuropsychological testing. Exp Neurol. 2005;191(Suppl):S95–103. https://doi.org/10.1016/j.expneurol.2004.06.017.
Firbank MJ, Lloyd J, Williams D, Barber R, Colloby SJ, Barnett N, et al. An evidence-based algorithm for the utility of FDG-PET for diagnosing Alzheimer’s disease according to presence of medial temporal lobe atrophy. Br J Psychiatry. 2016;208:491–6. https://doi.org/10.1192/bjp.bp.114.160804.
Higuchi M, Tashiro M, Arai H, Okamura N, Hara S, Higuchi S, et al. Glucose hypometabolism and neuropathological correlates in brains of dementia with Lewy bodies. Exp Neurol. 2000;162:247–56. https://doi.org/10.1006/exnr.2000.7342.
Ishii K, Soma T, Kono AK, Sofue K, Miyamoto N, Yoshikawa T, et al. Comparison of regional brain volume and glucose metabolism between patients with mild dementia with lewy bodies and those with mild Alzheimer’s disease. J Nucl Med. 2007;48:704–11. https://doi.org/10.2967/jnumed.106.035691.
Koeppe RA, Gilman S, Joshi A, Liu S, Little R, Junck L, et al. 11C-DTBZ and 18F-FDG PET measures in differentiating dementias. J Nucl Med. 2005;46:936–44.
Lim SM, Katsifis A, Villemagne VL, Best R, Jones G, Saling M, et al. The 18F-FDG PET cingulate island sign and comparison to 123I-beta-CIT SPECT for diagnosis of dementia with Lewy bodies. J Nucl Med. 2009;50:1638–45. https://doi.org/10.2967/jnumed.109.065870.
Minoshima S, Foster NL, Sima AA, Frey KA, Albin RL, Kuhl DE. Alzheimer’s disease versus dementia with Lewy bodies: cerebral metabolic distinction with autopsy confirmation. Ann Neurol. 2001;50:358–65.
Mosconi L, Tsui WH, Herholz K, Pupi A, Drzezga A, Lucignani G, et al. Multicenter standardized 18F-FDG PET diagnosis of mild cognitive impairment, Alzheimer’s disease, and other dementias. J Nucl Med. 2008;49:390–8. https://doi.org/10.2967/jnumed.107.045385.
O’Brien JT, Firbank MJ, Davison C, Barnett N, Bamford C, Donaldson C, et al. 18F-FDG PET and perfusion SPECT in the diagnosis of Alzheimer and Lewy body dementias. J Nucl Med. 2014;55:1959–65. https://doi.org/10.2967/jnumed.114.143347.
Kono AK, Ishii K, Sofue K, Miyamoto N, Sakamoto S, Mori E. Fully automatic differential diagnosis system for dementia with Lewy bodies and Alzheimer’s disease using FDG-PET and 3D-SSP. Eur J Nucl Med Mol Imaging. 2007;34:1490–7. https://doi.org/10.1007/s00259-007-0380-y.
Santens P, De Bleecker J, Goethals P, Strijckmans K, Lemahieu I, Slegers G, et al. Differential regional cerebral uptake of (18)F-fluoro-2-deoxy-D-glucose in Alzheimer’s disease and frontotemporal dementia at initial diagnosis. Eur Neurol. 2001;45:19–27. https://doi.org/10.1159/000052084.
Tripathi M, Tripathi M, Damle N, Kushwaha S, Jaimini A, D’Souza MM, et al. Differential diagnosis of neurodegenerative dementias using metabolic phenotypes on F-18 FDG PET/CT. Neuroradiol J. 2014;27:13–21. https://doi.org/10.15274/NRJ-2014-10002.
Panegyres PK, Rogers JM, McCarthy M, Campbell A, Wu JS. Fluorodeoxyglucose-positron emission tomography in the differential diagnosis of early-onset dementia: a prospective, community-based study. BMC Neurol. 2009;9:41. https://doi.org/10.1186/1471-2377-9-41.
Bergeron D, Beauregard J-M, Guimond J, Fortin M-P, Houde M, Poulin S, et al. Clinical impact of a second FDG-PET in atypical/unclear dementia syndromes. J Alzheimers Dis. 2016;49:695–705. https://doi.org/10.3233/JAD-150302.
Krudop WA, Dols A, Kerssens CJ, Prins ND, Moller C, Schouws S, et al. Impact of imaging and cerebrospinal fluid biomarkers on behavioral variant frontotemporal dementia diagnosis within a late-onset frontal lobe syndrome cohort. Dement Geriatr Cogn Disord. 2016;41:16–26. https://doi.org/10.1159/000441023.
Kerklaan BJ, van Berckel BNM, Herholz K, Dols A, van der Flier WM, Scheltens P, et al. The added value of 18-fluorodeoxyglucose-positron emission tomography in the diagnosis of the behavioral variant of frontotemporal dementia. Am J Alzheimers Dis Other Demen. 2014;29:607–13. https://doi.org/10.1177/1533317514524811.
Foster NL, Heidebrink JL, Clark CM, Jagust WJ, Arnold SE, Barbas NR, et al. FDG-PET improves accuracy in distinguishing frontotemporal dementia and Alzheimer’s disease. Brain. 2007;130:2616–35. https://doi.org/10.1093/brain/awm177.
Poljansky S, Ibach B, Hirschberger B, Männer P, Klünemann H, Hajak G, et al. A visual [18F]FDG-PET rating scale for the differential diagnosis of frontotemporal lobar degeneration. Eur Arch Psychiatry Clin Neurosci. 2011;261:433–46. https://doi.org/10.1007/s00406-010-0184-0.
Rabinovici GD, Rosen HJ, Alkalay A, Kornak J, Furst AJ, Agarwal N, et al. Amyloid vs FDG-PET in the differential diagnosis of AD and FTLD. Neurology. 2011;77:2034–42. https://doi.org/10.1212/WNL.0b013e31823b9c5e.
Perani D, Cerami C, Caminiti SP, Santangelo R, Coppi E, Ferrari L, et al. Cross-validation of biomarkers for the early differential diagnosis and prognosis of dementia in a clinical setting. Eur J Nucl Med Mol Imaging. 2016;43:499–508. https://doi.org/10.1007/s00259-015-3170-y.
Rostomian AH, Madison C, Rabinovici GD, Jagust WJ. Early 11C-PIB frames and 18F-FDG PET measures are comparable: a study validated in a cohort of AD and FTLD patients. J Nucl Med. 2011;52:173–9. https://doi.org/10.2967/jnumed.110.082057.
Ishii K, Sakamoto S, Sasaki M, Kitagaki H, Yamaji S, Hashimoto M, et al. Cerebral glucose metabolism in patients with frontotemporal dementia. J Nucl Med. 1998;39:1875–8.
Iaccarino L, Crespi C, Della Rosa PA, Catricala E, Guidi L, Marcone A, et al. The semantic variant of primary progressive aphasia: clinical and neuroimaging evidence in single subjects. PLoS One. 2015;10:e0120197. https://doi.org/10.1371/journal.pone.0120197.
De Reuck J, Decoo D, Marchau M, Santens P, Lemahieu I, Strijckmans K. Positron emission tomography in vascular dementia. J Neurol Sci. 1998;154:55–61.
Sabri O, Hellwig D, Schreckenberger M, Cremerius U, Schneider R, Kaiser HJ, et al. Correlation of neuropsychological, morphological and functional (regional cerebral blood flow and glucose utilization) findings in cerebral microangiopathy. J Nucl Med. 1998;39:147–54.
Mendez MF, Ottowitz W, Brown CV, Cummings JL, Perryman KM, Mandelkern MA. Dementia with leukoaraiosis: clinical differentiation by temporoparietal hypometabolism on (18)FDG-PET imaging. Dement Geriatr Cogn Disord. 1999;10:518–25. https://doi.org/10.1159/000017199.
Sultzer DL, Mahler ME, Cummings JL, Van Gorp WG, Hinkin CH, Brown C. Cortical abnormalities associated with subcortical lesions in vascular dementia. Clinical and position emission tomographic findings. Arch Neurol. 1995;52:773–80.
Nagata K, Maruya H, Yuya H, Terashi H, Mito Y, Kato H, et al. Can PET data differentiate Alzheimer’s disease from vascular dementia? Ann N Y Acad Sci. 2000;903:252–61.
Hoffmann M. Frontal network syndrome testing: clinical tests and positron emission tomography brain imaging help distinguish the 3 most common dementia subtypes. Am J Alzheimers Dis Other Demen. 2013;28:477–84. https://doi.org/10.1177/1533317513488920.
Reed BR, Eberling JL, Mungas D, Weiner M, Kramer JH, Jagust WJ. Effects of white matter lesions and lacunes on cortical function. Arch Neurol. 2004;61:1545–50. https://doi.org/10.1001/archneur.61.10.1545.
Kuczynski B, Reed B, Mungas D, Weiner M, Chui HC, Jagust W. Cognitive and anatomic contributions of metabolic decline in Alzheimer disease and cerebrovascular disease. Arch Neurol. 2008;65:650–5. https://doi.org/10.1001/archneur.65.5.650.
Kerrouche N, Herholz K, Mielke R, Holthoff V, Baron J-C. 18FDG PET in vascular dementia: differentiation from Alzheimer’s disease using voxel-based multivariate analysis. J Cereb Blood Flow Metab. 2006;26:1213–21. https://doi.org/10.1038/sj.jcbfm.9600296.
Mielke R, Pietrzyk U, Jacobs A, Fink GR, Ichimiya A, Kessler J, et al. HMPAO SPET and FDG PET in Alzheimer’s disease and vascular dementia: comparison of perfusion and metabolic pattern. Eur J Nucl Med. 1994;21:1052–60.
Seo SW, Cho SS, Park A, Chin J, Na DL. Subcortical vascular versus amnestic mild cognitive impairment: comparison of cerebral glucose metabolism. J Neuroimaging. 2009;19:213–9. https://doi.org/10.1111/j.1552-6569.2008.00292.x.
Duara R, Barker W, Loewenstein D, Pascal S, Bowen B. Sensitivity and specificity of positron emission tomography and magnetic resonance imaging studies in Alzheimer’s disease and multi-infarct dementia. Eur Neurol. 1989;29(Suppl 3):9–15.
Szelies B, Mielke R, Herholz K, Heiss WD. Quantitative topographical EEG compared to FDG PET for classification of vascular and degenerative dementia. Electroencephalogr Clin Neurophysiol. 1994;91:131–9.
Kipps CM, Hodges JR, Fryer TD, Nestor PJ. Combined magnetic resonance imaging and positron emission tomography brain imaging in behavioural variant frontotemporal degeneration: refining the clinical phenotype. Brain. 2009;132:2566–78. https://doi.org/10.1093/brain/awp077.
Varrone A, Asenbaum S, Vander Borght T, Booij J, Nobili F, Någren K, et al. EANM procedure guidelines for PET brain imaging using [18F]FDG, version 2. Eur J Nucl Med Mol Imaging. 2009;36:2103–10. https://doi.org/10.1007/s00259-009-1264-0.
Caso F, Gesierich B, Henry M, Sidhu M, LaMarre A, Babiak M, et al. Nonfluent/agrammatic PPA with in-vivo cortical amyloidosis and Pick’s disease pathology. Behav Neurol. 2013;26:95–106. https://doi.org/10.3233/BEN-2012-120255.
Ossenkoppele R, Jansen WJ, Rabinovici GD, Knol DL, van der Flier WM, van Berckel BNM, et al. Prevalence of amyloid PET positivity in dementia syndromes. JAMA. 2015;313:1939. https://doi.org/10.1001/jama.2015.4669.
Walker Z, Jaros E, Walker RWH, Lee L, Costa DC, Livingston G, et al. Dementia with Lewy bodies: a comparison of clinical diagnosis, FP-CIT single photon emission computed tomography imaging and autopsy. J Neurol Neurosurg Psychiatry. 2007;78:1176–81. https://doi.org/10.1136/jnnp.2006.110122.
Morgan S, Kemp P, Booij J, Costa DC, Padayachee S, Lee L, et al. Differentiation of frontotemporal dementia from dementia with Lewy bodies using FP-CIT SPECT. J Neurol Neurosurg Psychiatry. 2012;83:1063–70. https://doi.org/10.1136/jnnp-2012-302577.
Claassen DO, Parisi JE, Giannini C, Boeve BF, Dickson DW, Josephs KA. Frontotemporal dementia mimicking dementia with Lewy bodies. Cogn Behav Neurol. 2008;21:157–63. https://doi.org/10.1097/WNN.0b013e3181864a09.
Gorelick PB, Scuteri A, Black SE, Decarli C, Greenberg SM, Iadecola C, et al. Vascular contributions to cognitive impairment and dementia: a statement for healthcare professionals from the American heart association/American stroke association. Stroke. 2011;42:2672–713. https://doi.org/10.1161/STR.0b013e3182299496.
Acknowledgements
The procedure for assessing scientific evidence and defining consensual recommendations was funded by the European Association of Nuclear Medicine (EANM) and by the European Academy of Neurology (EAN). We thank the guidelines working group of EAN, particularly Simona Arcuti and Maurizio Leone, for methodological advice.
Funding
This project was funded in part by the European Association of Nuclear Medicine (EANM) and the European Academy of Neurology (EAN).
Author information
Authors and Affiliations
Consortia
Corresponding authors
Ethics declarations
Conflict of interest
Peter Nestor received discounted radiotracer from Piramal for a research study.
Flavio Nobili received personal fees and non-financial support from GE Healthcare, non-financial support from Eli Lilly and grants from Chiesi Farmaceutici.
Cristina Festari declares that she has no conflict of interest.
Daniele Altomare was the recipient of a grant allocated by the European Academy of Neurology (EAN) for data extraction and evidence assessment for the present project.
Jasmine Gandolfo declares that she has no conflict of interest.
Federica Agosta is Section Editor of NeuroImage: Clinical; has received speaker fees from Biogen Idec, Novartis, and Excellence in Medical Education; and receives or has received research support from the Italian Ministry of Health, AriSLA (Fondazione Italiana di Ricerca per la SLA), and the European Research Council. She received personal fees from Elsevier Inc.
Stefania Orini declares that she has no conflict of interest.
Javier Arbizu received grants from Eli Lilly & Company, Piramal and GE Healthcare.
Femke Bouwman declares that she has no conflict of interest.
Alexander Drzezga received grants and non-financial support from Eli Lilly & Company, Siemens and GE Healthcare; he also received non-financial support from Piramal.
Zuzana Walker received grants and tracers, personal fees for consultancy and speaker fees from GE Healthcare.
Ian Law declares that he has no conflict of interest.
Marina Boccardi has received funds from the European Association of Nuclear Medicine (EANM) to perform the evidence assessment and the global coordination of the present project. She has also received research grants from Piramal and served as a paid member of advisory boards for Eli Lilly.
Giovanni B Frisoni is principal investigator of industry-sponsored trials funded by AbbVie, Acadia, Altoida, Amoneta, Araclon, Biogen, Janssen, Novartis and Piramal; has received funding for investigator-initiated trials from GE, Piramal, and Avid–Lilly; and has received speaker fees from a number of pharma and imaging companies.
Ethical approval
This is a review article that does not contain any original study with human participants performed by any of the authors. Ethical approval is shown in each of the quoted original papers.
Informed consent
Not applicable; this is a review article. Informed consent statement is declared in each of the reviewed papers.
Rights and permissions
About this article
Cite this article
Nestor, P.J., Altomare, D., Festari, C. et al. Clinical utility of FDG-PET for the differential diagnosis among the main forms of dementia. Eur J Nucl Med Mol Imaging 45, 1509–1525 (2018). https://doi.org/10.1007/s00259-018-4035-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-018-4035-y