Abstract
Purpose
In recent years, multiple studies have demonstrated the value of volumetric FDG-PET/CT parameters as independent prognostic factors in patients with non-small cell lung cancer (NSCLC). We aimed to determine the optimal cut-off points of pretreatment volumetric FDG-PET/CT parameters in predicting overall survival (OS) in patients with locally advanced NSCLC and to recommend imaging biomarkers appropriate for routine clinical applications.
Methods
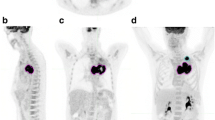
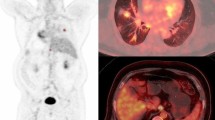
Patients with inoperable stage IIB/III NSCLC enrolled in ACRIN 6668/RTOG 0235 were included. Pretreatment FDG-PET scans were quantified using semiautomatic adaptive contrast-oriented thresholding and local-background partial-volume-effect-correction algorithms. For each patient, the following indices were measured: metabolic tumor volume (MTV), total lesion glycolysis (TLG), SUVmax, SUVmean, partial-volume-corrected TLG (pvcTLG), and pvcSUVmean for the whole-body, primary tumor, and regional lymph nodes. The association between each index and patient outcome was assessed using Cox proportional hazards regression. Optimal cut-off points were estimated using recursive binary partitioning in a conditional inference framework and used in Kaplan-Meier curves with log-rank testing. The discriminatory ability of each index was examined using time-dependent receiver operating characteristic (ROC) curves and corresponding area under the curve (AUC(t)).
Results
The study included 196 patients. Pretreatment whole-body and primary tumor MTV, TLG, and pvcTLG were independently prognostic of OS. Optimal cut-off points were 175.0, 270.9, and 35.5 cm3 for whole-body TLG, pvcTLG, and MTV, and were 168.2, 239.8, and 17.4 cm3 for primary tumor TLG, pvcTLG, and MTV, respectively. In time-dependent ROC analysis, AUC(t) for MTV and TLG were uniformly higher than that of SUV measures over all time points. Primary tumor and whole-body parameters demonstrated similar patterns of separation for those patients above versus below the optimal cut-off points in Kaplan-Meier curves and in time-dependent ROC analysis.
Conclusion
We demonstrated that pretreatment whole-body and primary tumor volumetric FDG-PET/CT parameters, including MTV, TLG, and pvcTLG, are strongly prognostic for OS in patients with locally advanced NSCLC, and have similar discriminatory ability. Therefore, we believe that, after validation in future trials, the derived optimal cut-off points for primary tumor volumetric FDG-PET/CT parameters, or their more refined versions, could be incorporated into routine clinical practice, and may provide more accurate prognostication and staging based on tumor metabolic features.



Similar content being viewed by others
References
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2016. CA Cancer J Clin. 2016;66(1):7–30.
Chen W, Zheng R, Baade PD, Zhang S, Zeng H, Bray F, et al. Cancer statistics in China, 2015. CA Cancer J Clin. 2016;66(2):115–32.
Network NCC. Non-Small Cell Lung Cancer (Version 4.2016). http://www.nccn.org/professionals/physician_gls/pdf/nscl.pdf. Accessed 3 Feb 2016.
Bradley J, Bae K, Choi N, Forster K, Siegel BA, Brunetti J, et al. A phase II comparative study of gross tumor volume definition with or without PET/CT fusion in dosimetric planning for non-small-cell lung cancer (NSCLC): primary analysis of radiation therapy oncology group (RTOG) 0515. Int J Radiat Oncol Biol Phys. 2012;82(1):435–41 e1.
Geiger GA, Kim MB, Xanthopoulos EP, Pryma DA, Grover S, Plastaras JP, et al. Stage migration in planning PET/CT scans in patients due to receive radiotherapy for non-small-cell lung cancer. Clin Lung Cancer. 2014;15(1):79–85.
Houshmand S, Boursi B, Salavati A, Simone CB 2nd, Alavi A. Applications of Fluorodeoxyglucose PET/computed tomography in the assessment and prediction of radiation therapy-related complications. PET Clin. 2015;10(4):555–71.
Simone CB 2nd, Houshmand S, Kalbasi A, Salavati A, Alavi A. PET-based thoracic radiation oncology. PET Clin. 2016;11(3):319–32.
Khiewvan B, Ziai P, Houshmand S, Salavati A, Ziai P, Alavi A. The role of PET/CT as a prognosticator and outcome predictor in lung cancer. Expert Rev Respir Med. 2016;10(3):317–30.
Chen HH, Chiu NT, Su WC, Guo HR, Lee BF. Prognostic value of whole-body total lesion glycolysis at pretreatment FDG PET/CT in non-small cell lung cancer. Radiology. 2012;264(2):559–66.
van Loon J, Offermann C, Ollers M, van Elmpt W, Vegt E, Rahmy A, et al. Early CT and FDG-metabolic tumour volume changes show a significant correlation with survival in stage I-III small cell lung cancer: a hypothesis generating study. Radiother Oncol. 2011;99(2):172–5.
Liao S, Penney BC, Wroblewski K, Zhang H, Simon CA, Kampalath R, et al. Prognostic value of metabolic tumor burden on 18F-FDG PET in nonsurgical patients with non-small cell lung cancer. Eur J Nucl Med Mol Imaging. 2012;39(1):27–38.
Burger IA, Casanova R, Steiger S, Husmann L, Stolzmann P, Huellner MW, et al. 18F-FDG PET/CT of non-small cell lung carcinoma under Neoadjuvant chemotherapy: background-based adaptive-volume metrics outperform TLG and MTV in predicting Histopathologic response. J Nucl Med. 2016;57(6):849–54.
Houshmand S, Salavati A, Basu S, Khiewvan B, Alavi A. The role of dual and multiple time point imaging of FDG uptake in both normal and disease states. Clin Transl Imaging. 2014;2(4):281–93.
Houshmand S, Salavati A, Hess S, Werner TJ, Alavi A, Zaidi H. An update on novel quantitative techniques in the context of evolving whole-body PET imaging. PET Clin. 2015;10(1):45–58.
Soret M, Bacharach SL, Buvat I. Partial-volume effect in PET tumor imaging. J Nucl Med. 2007;48(6):932–45.
Erlandsson K, Buvat I, Pretorius PH, Thomas BA, Hutton BF. A review of partial volume correction techniques for emission tomography and their applications in neurology, cardiology and oncology. Phys Med Biol. 2012;57(21):R119–59.
Hatt M, Le Pogam A, Visvikis D, Pradier O. Cheze le rest C. Impact of partial-volume effect correction on the predictive and prognostic value of baseline 18F-FDG PET images in esophageal cancer. J Nucl Med. 2012;53(1):12–20.
Machtay M, Duan F, Siegel BA, Snyder BS, Gorelick JJ, Reddin JS, et al. Prediction of survival by [18F]fluorodeoxyglucose positron emission tomography in patients with locally advanced non-small-cell lung cancer undergoing definitive chemoradiation therapy: results of the ACRIN 6668/RTOG 0235 trial. J Clin Oncol. 2013;31(30):3823–30.
Scheuermann JS, Saffer JR, Karp JS, Levering AM, Siegel BA. Qualification of PET scanners for use in multicenter cancer clinical trials: the American College of Radiology Imaging Network experience. J Nucl Med. 2009;50(7):1187–93.
Salavati A, Borofsky S, Boon-Keng TK, Houshmand S, Khiewvan B, Saboury B, et al. Application of partial volume effect correction and 4D PET in the quantification of FDG avid lung lesions. Mol Imaging Biol. 2015;17(1):140–8.
Hofheinz F, Langner J, Petr J, Beuthien-Baumann B, Oehme L, Steinbach J, et al. A method for model-free partial volume correction in oncological PET. EJNMMI Res. 2012;2(1):16.
Torigian DA, Lopez RF, Alapati S, Bodapati G, Hofheinz F, van den Hoff J, et al. Feasibility and performance of novel software to quantify metabolically active volumes and 3D partial volume corrected SUV and metabolic volumetric products of spinal bone marrow metastases on 18F-FDG-PET/CT. Hell J Nucl Med. 2011;14(1):8–14.
Schaefer A, Kim YJ, Kremp S, Mai S, Fleckenstein J, Bohnenberger H, et al. PET-based delineation of tumour volumes in lung cancer: comparison with pathological findings. Eur J Nucl Med Mol Imaging. 2013;40(8):1233–44.
Basaki K, Abe Y, Aoki M, Kondo H, Hatayama Y, Nakaji S. Prognostic factors for survival in stage III non-small-cell lung cancer treated with definitive radiation therapy: impact of tumor volume. Int J Radiat Oncol Biol Phys. 2006;64(2):449–54.
Dehing-Oberije C, De Ruysscher D, van der Weide H, Hochstenbag M, Bootsma G, Geraedts W, et al. Tumor volume combined with number of positive lymph node stations is a more important prognostic factor than TNM stage for survival of non-small-cell lung cancer patients treated with (chemo)radiotherapy. Int J Radiat Oncol Biol Phys. 2008;70(4):1039–44.
Koo TR, Moon SH, Lim YJ, Kim JY, Kim Y, Kim TH, et al. The effect of tumor volume and its change on survival in stage III non-small cell lung cancer treated with definitive concurrent chemoradiotherapy. Radiat Oncol. 2014;9:283.
Chiti A, Kirienko M, Gregoire V. Clinical use of PET-CT data for radiotherapy planning: what are we looking for? Radiother Oncol. 2010;96(3):277–9.
Ohri N, Duan F, Machtay M, Gorelick JJ, Snyder BS, Alavi A, et al. Pretreatment FDG-PET metrics in stage III non-small cell lung cancer: ACRIN 6668/RTOG 0235. J Natl Cancer Inst. 2015;107(4):djv004.
Bazan JG, Duan F, Snyder BS, Horng D, Graves EE, Siegel BA, et al. Metabolic tumor volume predicts overall survival and local control in patients with stage III non-small cell lung cancer treated in ACRIN 6668/RTOG 0235. Eur J Nucl Med Mol Imaging. 2017;44(1):17–24.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Funding
The ACRIN 6668/RTOG 0235 Trial receives funding from the National Cancer Institute through the grants U01 CA079778 and UO1 CA080098.
Conflict of interest
None.
Ethical approval
Patients consented to the original prospective study, which was approved by the local institutional review board of each participating institution.
Appendix
Appendix
Rights and permissions
About this article
Cite this article
Salavati, A., Duan, F., Snyder, B.S. et al. Optimal FDG PET/CT volumetric parameters for risk stratification in patients with locally advanced non-small cell lung cancer: results from the ACRIN 6668/RTOG 0235 trial. Eur J Nucl Med Mol Imaging 44, 1969–1983 (2017). https://doi.org/10.1007/s00259-017-3753-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00259-017-3753-x