Abstract
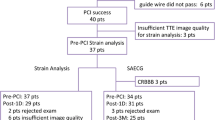
Surgical re-implantation of the left coronary artery (LCA) is the treatment of choice in anomalous origin of left coronary artery from pulmonary artery (ALCAPA). Despite normalization of left ventricular function after surgery, residual coronary lesions or myocardial fibrosis may be found. The aim of this study was to detect regional left ventricular dysfunction predictive of coronary lesions or residual myocardial fibrosis using speckle tracking. We enrolled ten patients treated with surgical re-implantation of LCA for ALCAPA. All patients were asymptomatic, and ejection fraction (EF) was normal. Using S-SR imaging, we studied longitudinal, radial, and circumferential function. A cardiac MRI was performed to assess myocardial fibrosis and the anatomy of the coronaries. In case of suspected coronary stenosis, a coronary angiography was performed. Finally, 20 normal subjects were enrolled as control group. Median age at surgery was 188 days, and mean follow-up was 8.7 ± 4.7 years. Longitudinal and circumferential functions were reduced in LCA territory compared to RCA territory and normal. MRI showed LCA stenosis in three of ten patients, confirmed by coronary angiography: these patients had the lowest longitudinal strain values in LCA territories (−11.7, −14.7 and −14.8%). Radial strain was preserved (Normal 45.6 ± 12.1, ALCAPA 43.5 ± 10.7%, p = ns), while circumferential strain was mildly depressed (−23.5 ± 3.8 vs. −20.3 ± 2.0%, p < 0.05). After LCA re-implantation, ALCAPA patients showed a residual sub-endocardial damage in LCA territories. Despite a normal systolic and diastolic function, the prevalence of residual coronary lesions was high. A mean longitudinal strain >−15% in LCA territories was able to identify those patients.

Similar content being viewed by others
Abbreviations
- ALCAPA:
-
Anomalous origin of left coronary artery from the pulmonary artery
- C-MRI:
-
Cardiac magnetic resonance imaging
- IVRT:
-
Isovolumetric relaxation time
- LCA:
-
Left coronary artery
- LGE:
-
Late gadolinium enhancement
- LV:
-
Left ventricle
- RCA:
-
Right coronary artery
- RV:
-
Right ventricle
- S:
-
Strain
- SR:
-
Strain rate
- TDI:
-
Tissue Doppler imaging
References
Cowies RA, Berdon WE (2007) Bland—White—Garland syndrome of anomalous left coronary artery arising from the pulmonary artery [ALPACA]: a historical review. Pediatr Radiol 37:890–895
Dodge-Khatami A, Mavroudis C, Backer CL (2002) Anomalous origin of the left coronary artery from the pulmonary artery: collective review of surgical therapy. Ann Thorac Surg 74:946–955
Wesselhoeft H, Fawcett JS, Johnson AL (1968) Anomalous origin of the left coronary artery from the pulmonary trunk: its clinical spectrum, pathology, and pathophysiology, based on a review of 140 cases with seven further cases. Circulation 38:403–425
Shivalkar B, Borgers M, Daemen W, Gewillig M, Flameng W (1994) ALCAPA syndrome: an example of chronic myocardial hypoperfusion? J Am Coll Cardiol 23:772–778
Smith A, Arnold R, Anderson RH, Qureshi SA, Gertis LM, Mckay R. (1989) Anomalous origin of the left coronary artery from the pulmonary trunk: anatomic findings in relation to pathophysiology and surgical repair. J Thorac Cardiovasc Surg 98:16–24.
Singh TP, Dicarli MF, Sullivan NM, Leonen MF, Morrow WR (1998) Myocardial flow reserve in long term survivors of repair of anomalous left coronary artery from pulmonary artery. J Am Coll Cardiol 31:437–443
Secinaro A, Ntsinjana H, Tann O et al (2001) Cardiovascular magnetic resonance findings in repaired anomalous left coronary artery to pulmonary artery connection (ALCAPA). J Cardiovasc Magn Reson 13:27
Latus H, Gummel K, Rupp S et al. (2014) Cardiovascular magnetic resonance assessment of ventricular function and myocardial scarring before and early after repair of anomalous left coronary artery from the pulmonary artery. J Carvasc Magn Reson 16:3
Di Salvo G, Pacileo G, Rea A et al (2005) Quantitative evaluation of regional myocardial function using strain and strain rate imaging: normal values in pediatric age. Ital Heart J 6:420–426
Di Salvo G, Pacileo G, Gala S et al (2006) Strain rate imaging: data acquisition and post processing. Minerva Cardioangiol 54:451–459
Langeland S, D’hooge J, Wouters PF et al (2005) Experimental validation of a new ultrasound method for the simultaneous assessment of radial and longitudinal myocardial deformation independent of insonation angle. Circulation 112:2157–2162
Castaldi B, Santoro G, Di Salvo G et al (2013) Impact of the Amplatzer atrial septal occlude device on left ventricular function in pediatric patients. Pediatr Cardiol 34(7):1645–1651
Cabrera AG, Chen DW, Pignatelli RH et al (2015) Outcomes of anomalous left coronary artery from pulmonary artery repair: beyond normal function. Ann Thorac Surg 99(4):1342–1347
Fratz S, Hager A, Schreiber C, Schwaiger M, Hess J, Stern HC (2011) Long-term myocardial scarring after operation for anomalous left coronary artery from the pulmonary artery. Ann Thorac Surg 92(5):1761–1765
Shivalkar B, Borgers M, Daenen W, Gewillig M, Flameng W. (2009) ALCAPA syndrome: an example of chronic myocardial hypoperfusion? J Am Coll Cardiol 23(3): 772–778
Bergmann O, Bhardwaj RD, Bernard S et al (2009) Evidence for cardiomyocyte renewal in humans. Science 324:98–102
Schmitt B, Bauer S, Kutty S, Nordmeyer S, Nasseri B, Berger F, Alexi-Meskishvili V (2014) Myocardial perfusion, scarring, and function in anomalous left coronary artery from the pulmonary artery syndrome: a long-term analysis using magnetic resonance imaging. Ann Thorac Surg 98(4):1425–1436
Di Salvo G, Eyskens B, Claus P et al (2004) Late post-repair ventricular function in patients with origin of the left main coronary artery from the pulmonary trunk. Am J Cardiol 93:506–508
Nordgaard H, Swillens A, Nordhaug D et al (2010) Impact of competitive flow on wall shear stress in coronary surgery: computational fluid dynamics of a LIMA-LAD model. Cardiovasc Res 88(3):512–519
Neglia D, Rovai D, Caselli C et al. (2015) Detection of significant coronary artery disease by noninvasive anatomical and functional imaging. Circ Cardiovasc Imaging 8(3):e002179
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Rights and permissions
About this article
Cite this article
Castaldi, B., Vida, V., Reffo, E. et al. Speckle Tracking in ALCAPA Patients After Surgical Repair as Predictor of Residual Coronary Disease. Pediatr Cardiol 38, 794–800 (2017). https://doi.org/10.1007/s00246-017-1583-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00246-017-1583-z