Abstract
Purpose
Pharmacology and pharmacotherapy education is being increasingly integrated in medical curricula, which might lead to a specific loss of knowledge in these subjects. This, in turn, could lead to harmful prescribing errors, especially in vulnerable older patients.
Methods
Teachers who coordinated education in Dutch medical schools completed a structured interview on (geriatric) pharmacology and pharmacotherapy education. A list of core learning goals was developed. Pharmacology and pharmacotherapy education in general was compared to geriatric pharmacology and pharmacotherapy education.
Results
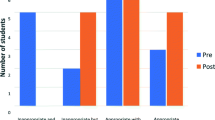
All Dutch medical schools participated. Contact hours for education in pharmacology and pharmacotherapy ranged from 39 to 107 h; ECTSs (representing 28 study hours) ranged from 0 to 3. The various curricula covered, on average, 79 % of all learning goals for these subjects: knowledge 85 %, skills 76 %, and attitudes 66 %; the curricula also covered specific geriatric goals: knowledge 87 % and skills 65 %. All geriatric learning goals were met if a geriatrician was among the coordinators. Half (4 of 8) of the medical schools lacked appropriate assessment procedures. Evaluation was mostly based on students’ opinions. Teachers rated students as being moderately well prepared for daily practice.
Conclusions
There are large differences in the quantity and quality of (geriatric) pharmacology and pharmacotherapy education in Dutch medical schools. In general, more time should be devoted to skills and attitude, and the assessment procedures should be optimized with high priority. Other curricula with a problem-based approach might benefit from the points of improvement described in this article.
Similar content being viewed by others
References
Neville AJ (2009) Problem-based learning and medical education forty years on. A review of its effects on knowledge and clinical performance. Med Princ Pract 18(1):1–9
Smits PB, Verbeek JH, de Buisonje CD (2002) Problem based learning in continuing medical education: a review of controlled evaluation studies. BMJ 324(7330):153–156
Keijsers CJ, Custers EJ, ten Cate OT (2009) A new, problem oriented medicine curriculum in Utrecht: less basic science knowledge. Ned Tijdschr Geneeskd 153:B400
Members of EMERGE,Erice Medication Errors Research Group, Agrawal A, Aronson JK, Britten N, Ferner RE, de Smet PA et al (2009) Medication errors: problems and recommendations from a consensus meeting. Br J Clin Pharmacol 67(6):592–598
Krahenbuhl-Melcher A, Schlienger R, Lampert M, Haschke M, Drewe J, Krahenbuhl S (2007) Drug-related problems in hospitals: a review of the recent literature. Drug Saf 30(5):379–407
Leendertse AJ, Egberts AC, Stoker LJ, van den Bemt PM, HARM Study Group (2008) Frequency of and risk factors for preventable medication-related hospital admissions in the Netherlands. Arch Intern Med 168(17):1890–1896
Lesar TS, Briceland L, Stein DS (1997) Factors related to errors in medication prescribing. JAMA 277(4):312–317
Tichelaar J, Richir MC, Avis HJ, Scholten HJ, Antonini NF, De Vries TP (2010) Do medical students copy the drug treatment choices of their teachers or do they think for themselves? Eur J Clin Pharmacol 66(4):407–412
Heaton A, Webb DJ, Maxwell SR (2008) Undergraduate preparation for prescribing: the views of 2413 UK medical students and recent graduates. Br J Clin Pharmacol 66(1):128–134
Keijsers CJ, van Hensbergen L, Jacobs L, Brouwers JR, de Wildt DJ, ten Cate OT et al (2012) Geriatric pharmacology and pharmacotherapy education for health professionals and students: a systematic review. Br J Clin Pharmacol 74(5):762–773
de Vries TP, Henning RH, Hogerzeil HV, Bapna JS, Bero L, Kafle KK et al (1995) Impact of a short course in pharmacotherapy for undergraduate medical students: an international randomised controlled study. Lancet 346(8988):1454–1457
Ross S, Loke YK (2009) Do educational interventions improve prescribing by medical students and junior doctors? A systematic review. Br J Clin Pharmacol 67(6):662–670
Keijsers CJ, Segers WS, de Wildt DJ, Brouwers JR, Keijsers L, Jansen PA (2014) Implementation of the WHO-6-step method in the medical curriculum to improve pharmacology knowledge and pharmacotherapy skills. Br J Clin Pharmacol. doi:10.1111/bcp.12575
Walley T, Bligh J, Orme M, Breckenridge A (1994) Clinical pharmacology and therapeutics in undergraduate medical education in the UK: current status. Br J Clin Pharmacol 37(2):129–135
O'Shaughnessy L (2010) Teaching of clinicalpharmacology and therapeutics in UK medical schools: current status in 2009. Br J Clin Pharmacol 70(1):143–148
Harden RM (2001) AMEE Guide No. 21: curriculum mapping: a tool for transparent and authentic teaching and learning. Med Teach 23(2):123–137
Nederlandse Federatie van Universitaire Centra (2009) Raamplan Artsopleiding. Available at: http://www.nfu.nl/img/pdf/Raamplan_Artsopleiding_2009.pdf. Accessed Aug 2014
Carter C (1985) A taxonomy of objectives for professional education. Stud High Educ 10(2):135–149
van Doorn A (2007) The value of a learning content management system (LCMS) for assessment of an internet application programme ‘Pscribe’ in problem-based pharmacotherapy teaching. Basic Clin Pharmacol Toxicol 101:51–102
Franson KL, Dubois EA, de Kam ML, Cohen AF (2008) Measuring learning from the TRC pharmacology E-Learning program. Br J Clin Pharmacol 66(1):135–141
Smee S (2003) Skill based assessment. BMJ 326(7391):703–706
Kongkaew C, Noyce PR, Ashcroft DM (2008) Hospital admissions associated with adverse drug reactions: a systematic review of prospective observational studies. Ann Pharmacother 42(7):1017–1025
Aronson JK, Henderson G, Webb DJ, Rawlins MD (2006) A prescription for better prescribing. BMJ 333(7566):459–460
Richir MC, Tichelaar J, Geijteman EC, de Vries TP (2008) Teaching clinical pharmacology and therapeutics with an emphasis on the therapeutic reasoning of undergraduate medical students. Eur J Clin Pharmacol 64(2):217–224
Raman M, McLaughlin K, Violato C, Rostom A, Allard JP, Coderre S (2010) Teaching in small portions dispersed over time enhances long-term knowledge retention. Med Teach 32(3):250–255
Wijnen-Meijer M, ten Cate OT, van der Schaaf M, Borleffs JC (2010) Vertical integration in medical school: effect on the transition to postgraduate training. Med Educ 44(3):272–279
Schwartz A, Weiner SJ, Harris IB, Binns-Calvey A (2010) An educational intervention for contextualizing patient care and medical students’ abilities to probe for contextual issues in simulated patients. JAMA 304(11):1191–1197
Wood T (2009) Assessment not only drives learning, it may also help learning. Med Educ 43(1):5–6
Nara N, Suzuki T, Tohda S (2011) The current medical education system in the world. J Med Dent Sci 58(2):79–83
Jippes M, Majoor GD (2008) Influence of national culture on the adoption of integrated and problem-based curricula in Europe. Med Educ 42(3):279–285
Maxwell SRJ, Webb DJ (2006) Clinical pharmacology - Too young to die? Lancet 367(9513):799–800
Hafler JP, Ownby AR, Thompson BM, Fasser CE, Grigsby K, Haidet P et al (2011) Decoding the learning environment of medical education: a hidden curriculum perspective for faculty development. Acad Med 86(4):440–444
Brinkman DJ, Tichelaar J, van Agtmael MA, de Vries TP, Richir MC (2015) Self-reported confidence in prescribing skills correlates poorly with assessed competence in fourth-year medical students. J Clin Pharmacol
Maxwell S, Walley T, Ferner RE (2002) Using drugs safely. Br Med J 324(7343):930–931
Acknowledgments
The authors would like to thank all curriculum coordinators who participated in this study and approved the use of the data in the manuscript: Prof. Dr. Sophia EJA de Rooij (University of Amsterdam), Dr. WMC (Mieke) Mulder (University of Amsterdam), Prof. Dr. Arnold G Vulto (Erasmus University), Dr. Nicole GM Hunfeld (Erasmus University), Dr. JeroenHassink (Erasmus University), Dr. Robert Rissmann (Leiden University), Dr. Marleen HM Hessel (Leiden University), Dr. Ben Janssen (University Maastricht), Adriaan BD van Doorn (University of Groningen), Dr. Itte de Waard-Siebinga (University of Groningen), Dr. Kees Kramers (Radboud University Nijmegen), Dr. Bas Schouwenberg (Radboud University Nijmegen), Dr. TB Yves Liem (University of Utrecht), and Dr. Benjamin Drukarch (VU University Medical Centre).
The authors would like to thank the other members of the Education Committee/working group Research of the Dutch Society of Clinical pharmacology and Biopharmacy (NVKF&B) for their contribution in the design of the study: Dr. Milan C. Richir (VU University Medical Centre) and Dr. Floris H.M. van Molkot (University Maastricht).
The authors would like to thank Sascha Bosman, medical student, who participated in the data collection.
Sources of support
Expertise Centre Pharmacotherapy in Old Persons (EPHOR) is funded by The Netherlands Organisation for Health Research and Development (ZonMw, project number 11.310.4001)
Declaration of interest
All authors have completed the Unified Competing Interest form at www.icmje.org/coi_disclosure.pdf (available on request from the corresponding author). Prof. Dr. Brouwers reports personal fees from Consultancy Europe-ExproMuenchen[Germ], personal fees from Consultancy Eijkman & Kuipers [NL], personal fees from Consultancy W-Pharma Wavre [B], personal fees from President Ethical Review Board, personal fees from Pharmaceutischweekblad, personal fees from Tijdschr v Prakt. Farmacotherapie MFM, grants from St. Ondersteuningsfonds Ephor, all outside the submitted work. All other authors declare no support from any organization for the submitted work, no financial relationships with any organizations that might have an interest in the submitted work in the previous 3 years, and no other relationships or activities that could appear to have influenced the submitted work.
Funding
EPHOR is funded by the Netherlands Organisation for Health Research and Development (ZonMw, project number 11.310.4001) in the Netherlands (www.zonmw.nl). The sponsor did not have any role in the design and conduct of the study, collection, management, analysis, interpretation of the data, review or approval of the manuscript, and decision to submit the manuscript for publication.
Contribution of author statement
PJ and CK had full access to all the data and take responsibility for the integrity of the data and the accuracy of the data analysis.
Study concept and design: Keijsers, de Wit, Tichelaar, de Vries, de Wildt, Brouwers, and Jansen.
Acquisition of data: Keijsers and Bosman
Analysis and interpretation of data: Keijsers and Tichelaar
Drafting of the manuscript: Keijsers
Critical revision of the manuscript for important intellectual content: Tichelaar, de Wit, de Wildt, Brouwers, Jansen, and de Vries
Obtained funding: Brouwers and Jansen
Administrative, technical, or material support: Jansen
Study supervision: De Wildt, Brouwers and Jansen
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
ESM 1
(DOCX 28 kb)
Rights and permissions
About this article
Cite this article
Keijsers, C.J.P.W., de Wit, J.E., Tichelaar, J. et al. Education on prescribing for older patients in the Netherlands: a curriculum mapping. Eur J Clin Pharmacol 71, 603–609 (2015). https://doi.org/10.1007/s00228-015-1830-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00228-015-1830-2