Abstract
Introduction and hypothesis
We hypothesized obesity increases the risk of pelvic organ prolapse recurrence (POP-R) after primary apical prolapse repair.
Methods
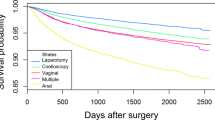
We conducted a retrospective cohort study of 353 women who underwent primary apical prolapse surgery from 2011 to 2016. Demographic and clinical data were abstracted from medical records. Multivariable Cox proportional hazard models were used to generate hazard ratios (HR) for association between obesity (BMI ≥ 30 kg/m2) and POP-R (leading edge > 0), adjusting for potential confounders. Given the potential for outcome ascertainment bias due to differential loss to follow-up, a sensitivity analysis was performed assuming all patients with < 6 months of follow-up developed POP-R.
Results
Ten percent of women developed POP-R. The median follow-up time was 7 months (range 1.4, 63.9). Twenty-four percent of patients were Black and 70% were White; 37% were obese. After controlling for confounders, obese women did not have an increased risk of POP-R (aHR 1.39; 95% CI 0.67, 2.86, p = 0.38). Although only marginally statistically significant, patients who developed POP-R were more likely to be current smokers (aHR 3.48, 95% CI 1.14, 10.67; p = 0.06) or previous smokers (aHR 1.86, 95% CI 0.82, 4.24, p = 0.06) in comparison to non-smokers. Sensitivity analysis showed loss to follow-up had the potential to influence our results.
Conclusions
Obesity was not a risk factor for POP-R in our cohort. Larger, prospective studies with longer postoperative follow-up time are needed to fully elucidate the relationship between obesity and POP-R.

Similar content being viewed by others
References
Gutman RE, Ford DE, Quiroz LH, Shippey SH, Handa VL. Is there a pelvic organ prolapse threshold that predicts pelvic floor symptoms? Am J Obstet Gynecol. 2008;199(6):683 e681–7. https://doi.org/10.1016/j.ajog.2008.07.028.
Barber MD, Maher C. Epidemiology and outcome assessment of pelvic organ prolapse. Int Urogynecol J. 2013;24(11):1783–90. https://doi.org/10.1007/s00192-013-2169-9.
Vergeldt TF, Weemhoff M, IntHout J, Kluivers KB. Risk factors for pelvic organ prolapse and its recurrence: a systematic review. Int Urogynecol J. 2015;26(11):1559–73. https://doi.org/10.1007/s00192-015-2695-8.
Hendrix SL, Clark A, Nygaard I, Aragaki A, Barnabei V, McTiernan A. Pelvic organ prolapse in the Women's Health Initiative: gravity and gravidity. Am J Obstet Gynecol. 2002;186(6):1160–6. https://doi.org/10.1067/mob.2002.123819.
Whitcomb EL, Rortveit G, Brown JS, Creasman JM, Thom DH, Van Den Eeden SK, et al. Racial differences in pelvic organ prolapse. Obstet Gynecol. 2009;114(6):1271–7. https://doi.org/10.1097/AOG.0b013e3181bf9cc8.
Nygaard I, Brubaker L, Zyczynski HM, Cundiff G, Richter H, Gantz M, et al. Long-term outcomes following abdominal sacrocolpopexy for pelvic organ prolapse. JAMA. 2013;309(19):2016–24. https://doi.org/10.1001/jama.2013.4919.
National Institutes of Health. Clinical guidelines on the identification, evaluation, and treatment of overweight and obesity in adults--the evidence report. Obes Res. 1998;6(Suppl 2):51S–209S.
Bradley CS, Kenton KS, Richter HE, Gao X, Zyczynski HM, Weber AM, et al. Obesity and outcomes after sacrocolpopexy. Am J Obstet Gynecol. 2008;199(6):690 e691–8. https://doi.org/10.1016/j.ajog.2008.07.030.
Giri A, Hartmann KE, Hellwege JN, Velez Edwards DR, Edwards TL. Obesity and pelvic organ prolapse: a systematic review and meta-analysis of observational studies. Am J Obstet Gynecol. 2017;217(1):11–26 e13. https://doi.org/10.1016/j.ajog.2017.01.039.
Turner L, Lavelle E, Lowder JL, Shepherd JP. The impact of obesity on intraoperative complications and prolapse recurrence after minimally invasive Sacrocolpopexy. Female Pelvic Med Reconstr Surg. 2016;22(5):317–23. https://doi.org/10.1097/SPV.0000000000000278.
Rappa C, Saccone G. Recurrence of vaginal prolapse after total vaginal hysterectomy with concurrent vaginal uterosacral ligament suspension: comparison between normal-weight and overweight women. Am J Obstet Gynecol. 2016;215(5):601 e601–4. https://doi.org/10.1016/j.ajog.2016.06.022.
Pratt TS, Hudson CO, Northington GM, Greene KA. Obesity and perioperative complications in pelvic reconstructive surgery in 2013: analysis of the National Inpatient Sample. Female Pelvic Med Reconstr Surg. 2018;24(1):51–5. https://doi.org/10.1097/SPV.0000000000000454.
Shah DK, Vitonis AF, Missmer SA. Association of body mass index and morbidity after abdominal, vaginal, and laparoscopic hysterectomy. Obstet Gynecol. 2015;125(3):589–98. https://doi.org/10.1097/AOG.0000000000000698.
Burneikis D, Morris-Stiff G, Chalikonda S. Time attributable to obesity in surgery: a multi-specialty report on day-of-surgery resource utilization from 189,264 cases. World J Surg. 2018;42(10):3125–33. https://doi.org/10.1007/s00268-018-4599-5.
Chong W, Bui AH, Menhaji K. Incidence and risk factors for venous thromboembolism events after different routes of pelvic organ prolapse repairs. Am J Obstet Gynecol. 2020;223(2):268 e261–26. https://doi.org/10.1016/j.ajog.2020.05.020.
Manodoro S, Frigerio M, Cola A, Spelzini F, Milani R. Risk factors for recurrence after hysterectomy plus native-tissue repair as primary treatment for genital prolapse. Int Urogynecol J. 2018;29(1):145–51. https://doi.org/10.1007/s00192-017-3448-7.
Barber MD, Brubaker L, Burgio KL, Richter HE, Nygaard I, Weidner AC, et al. Comparison of 2 transvaginal surgical approaches and perioperative behavioral therapy for apical vaginal prolapse: the OPTIMAL randomized trial. JAMA. 2014;311(10):1023–34. https://doi.org/10.1001/jama.2014.1719.
Whiteside JL, Weber AM, Meyn LA, Walters MD. Risk factors for prolapse recurrence after vaginal repair. Am J Obstet Gynecol. 2004;191(5):1533–8. https://doi.org/10.1016/j.ajog.2004.06.109.
Diez-Itza I, Aizpitarte I, Becerro A. Risk factors for the recurrence of pelvic organ prolapse after vaginal surgery: a review at 5 years after surgery. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18(11):1317–24. https://doi.org/10.1007/s00192-007-0321-0.
Friedman T, Eslick GD, Dietz HP. Risk factors for prolapse recurrence: systematic review and meta-analysis. Int Urogynecol J. 2018;29(1):13–21. https://doi.org/10.1007/s00192-017-3475-4.
Aslam MF, Osmundsen B, Edwards SR, Matthews C, Gregory WT. Preoperative prolapse stage as predictor of failure of Sacrocolpopexy. Female Pelvic Med Reconstr Surg. 2016;22(3):156–60. https://doi.org/10.1097/SPV.0000000000000233.
Kawasaki A, Corey EG, Laskey RA, Weidner AC, Siddiqui NY, Wu JM. Obesity as a risk for the recurrence of anterior vaginal wall prolapse after anterior colporrhaphy. J Reprod Med. 2013;58(5–6):195–9.
Edenfield AL, Amundsen CL, Weidner AC, Wu JM, George A, Siddiqui NY. Vaginal prolapse recurrence after uterosacral ligament suspension in normal-weight compared with overweight and obese women. Obstet Gynecol. 2013;121(3):554–9. https://doi.org/10.1097/AOG.0b013e3182839eeb.
Shull BL. Pelvic organ prolapse: anterior, superior, and posterior vaginal segment defects. Am J Obstet Gynecol. 1999;181(1):6–11. https://doi.org/10.1016/s0002-9378(99)70427-8.
Toozs-Hobson P, Boos K, Cardozo L. Management of vaginal vault prolapse. Br J Obstet Gynaecol. 1998;105(1):13–7. https://doi.org/10.1111/j.1471-0528.1998.tb09343.x.
Summers A, Winkel LA, Hussain HK, DeLancey JO. The relationship between anterior and apical compartment support. Am J Obstet Gynecol. 2006;194(5):1438–43. https://doi.org/10.1016/j.ajog.2006.01.057.
Rooney K, Kenton K, Mueller ER, FitzGerald MP, Brubaker L. Advanced anterior vaginal wall prolapse is highly correlated with apical prolapse. Am J Obstet Gynecol. 2006;195(6):1837–40. https://doi.org/10.1016/j.ajog.2006.06.065.
Bump RC, Mattiasson A, Bo K, Brubaker LP, DeLancey JO, Klarskov P, et al. The standardization of terminology of female pelvic organ prolapse and pelvic floor dysfunction. Am J Obstet Gynecol. 1996;175(1):10–7. https://doi.org/10.1016/s0002-9378(96)70243-0.
Mairesse S, Chazard E, Giraudet G, Cosson M, Bartolo S. Complications and reoperation after pelvic organ prolapse, impact of hysterectomy, surgical approach and surgeon experience. Int Urogynecol J. 2020. https://doi.org/10.1007/s00192-019-04210-6.
Park S, Baek KA. Association of General Obesity and Abdominal Obesity with the prevalence of urinary incontinence in women: cross-sectional secondary data analysis. Iran J Public Health. 2018;47(6):830–7.
Acknowledgements
We would like to thank Dr. Alexcis Ford for her help with project development and Emilie Morris for her help with data collection.
Author information
Authors and Affiliations
Contributions
ND Metcalfe: Protocol/project development, data collection/management, manuscript writing/editing.
LM Shandley: Protocol/project development, data analysis, manuscript editing.
M Young: Protocol/project development, manuscript editing.
M Higgins: Data collection/management, manuscript writing.
C Abanulo: Data collection/management.
GM Northington: Protocol/project development, manuscript editing, project mentor.
Corresponding author
Ethics declarations
Financial disclaimers/conflicts of interest
None.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
ESM 1
(DOCX 255 kb)
Rights and permissions
About this article
Cite this article
Metcalfe, N.D., Shandley, L.M., Young, M.R. et al. Pelvic organ prolapse recurrence after apical prolapse repair: does obesity matter?. Int Urogynecol J 33, 275–284 (2022). https://doi.org/10.1007/s00192-021-04806-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00192-021-04806-x