Abstract
Background and significance
The Cochrane Database of Systematic Reviews published a manuscript critical of the use of the FAST examination. The reference is Stengel D. Bauwens K. Sehouli J. Rademacher G. Mutze S. Ekkernkamp A. Porzsolt F. Emergency ultrasound-based algorithms for diagnosing blunt abdominal trauma. Cochrane Database of Systematic Reviews. (2):CD004446, 2005. UI: 15846717. The stated objective was the assessment of the “efficiency and effectiveness” of ultrasound-inclusive evaluative algorithms in patients with suspected blunt abdominal trauma (BAT). The primary outcome measures explored were Mortality, CT and DPL use, and laparotomy rates. Little or no benefit was seen and the conclusion was that “there is insufficient evidence from randomized controlled trials to justify promotion” of FAST in patients with BAT. While the review used the same rigorous methods employed in all Cochrane Reviews, it appears that several serious flaws plagued the manuscript. The finest methodological rigor cannot yield usable results, if it is not applied to a clinically relevant question. In a world of increasingly conservative management of BAT, do we need FAST, a rapid, repeatable screening modality at the point-of-care to visualize any amount of free fluid or any degree of organ injury? The obvious answer is no. However, quantifying the value of FAST to predict the need for immediate operative intervention (OR) is essential.
Methods
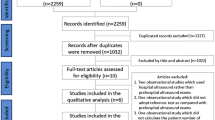
To rebut this recurrent review, a systematic literature review was conducted using verbatim methodologies as described in the Cochrane Review with the exception of telephone contacts. Data were tabulated and presented descriptively.
Results
Out of 487 citations, 163 articles were fully screened, 11 contained prospectively derived data with FAST results, patient disposition and final diagnoses, and a description of cases considered false negatives or false positives. Of the 2,755 patients, 448 (16%) went to the OR. There were a total of 5 patients with legitimately false-negative diagnoses made based on the FAST: 3 involving inadequate scans and 2 of blunt trauma-induced small bowel perforations without hemoperitoneum.
Conclusion
The FAST examination, adequately completed, is a nearly perfect test for predicting a “Need for OR” in patients with blunt torso trauma.
Similar content being viewed by others
Background
The Cochrane Database of Systematic Reviews published a manuscript critical of the use of the FAST examination. The reference is Stengel D. Bauwens K. Sehouli J. Rademacher G. Mutze S. Ekkernkamp A. Porzsolt F. Emergency ultrasound-based algorithms for diagnosing blunt abdominal trauma. Cochrane Database of Systematic Reviews. (2):CD004446, 2005. UI: 15846717 [1]. The stated objective was the assessment of the “efficiency and effectiveness” of ultrasound-inclusive evaluative algorithms in patients with suspected blunt abdominal trauma (BAT). In the 4 trials with 1,037 patients reviewed, the primary outcome measures explored were mortality, CT use, and DPL and operative intervention rates. Little or no benefit was seen and the conclusion was that “there is insufficient evidence from randomized controlled trials to justify promotion” of FAST in patients with BAT.
While the review used the same rigorous methods employed in all Cochrane Reviews, it appears that several serious flaws plague the manuscript. First, basic power calculations using data from the National Trauma Data Bank of the American College of Surgeons [2] suggest that reliably measuring a mortality difference would require over 5,000 patients rendering the first outcome measure inappropriate given the combined sample size of all published studies. Second, published literature [3–6] included in the review) have shown significant reductions in CT and DPL use, when FAST is used. Finally, finding no difference in operative intervention rates in study and control patients in the RCTs (Boulanger, Rose, and Melniker), which was criticized in the Cochrane Review, in fact indicates the assignment groups were well match, is a strength of the reviewed studies, not a weakness.
The finest methodological rigor cannot yield usable results, if they are not applied to the right, clinically relevant question. Do we need FAST to visualize any amount of free fluid or any degree of organ injury? In a world of increasingly conservative management of BAT, the obvious answer is no. However, quantifying the ability of FAST to predict the need for immediate operative intervention (OR) is essential. Toward this end, two investigations were undertaken.
In a post hoc analysis of the SOAP-1 trial, of the 69 study arm patients with blunt torso trauma necessitating OR, the FAST correctly identified all patients needing OR and cleared all patients not requiring immediate thoraco-abdominal surgery. Of interest, there were no non-therapeutic laparotomies and CT identified no other patients with intra-abdominal or intra-thoracic injuries requiring operative intervention that had not been identified by FAST.
Next, a literature review was conducted using verbatim methodologies as used in the Cochrane Review with the exception of telephone contacts. This Cochrane-sk study is described below.
Methods
Criteria for considering studies for this review
Types of studies
Randomized and quasi-randomized controlled trials compared trauma algorithms with ultrasonography, alone or in combination with other established diagnostic tests (i.e., computed tomography [CT], diagnostic peritoneal lavage [DPL], clinical monitoring), to algorithms without the use of ultrasound. Reporting of FAST findings, other test findings, operative findings, and explanations of false-positive and -negative cases was required for inclusion. Trials were included irrespective of blinding, and number of patients randomized.
Types of participants
Hemodynamically stable or unstable patients with suspected torso injury after blunt trauma, as a single injury or an injury accompanying multiple trauma, were included. Studies investigating patients with only stab wounds and gunshot wounds were excluded.
Types of intervention
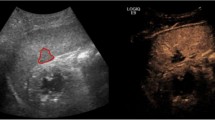
Diagnostic algorithms including ultrasonography to detect free intra-abdominal, intra-thoracic, and/or intra-pericardial fluid (focused assessment of sonography for trauma [FAST] or enhanced FAST [eFAST]), including ultrasound examinations performed by radiologists, non-radiologist clinicians, or ultrasound technicians, in combination with subsequent confirmatory tests (i.e., CT, DPL, OR reports, or clinical monitoring).
Objective
The objective is to study whether diagnostic algorithms using ultrasonography in the emergency department or trauma bay accurately predict which patients with blunt torso trauma require immediate OR.
The following hypotheses were tested:
-
That a positive FAST is predictive of a need for OR.
-
That a negative FAST is predictive of no need for OR.
Search methods for identification of studies
Trials indexed in MEDLINE and PUBMED between 1966 and May 2009 were identified by the following strategy:
-
1
Abdominal injuries
-
2
Thoracic injuries
-
3
Wounds, nonpenetrating
-
4
Multiple trauma OR polytrauma
-
5
Retroperitoneum
-
6
Rupture
-
7
Shock, traumatic
-
8
Hemoperitoneum OR haemoperitoneum OR free fluid OR intraperitoneal fluid
-
9
Spleen OR splenic
-
10
Liver OR hepatic
-
11
Accidents
-
12
Accidents, traffic
-
13
Seat belts
-
14
Bicycling
-
15
Motorcycles
-
16
Ultras* OR echotomogr* OR sonogr*
-
17
Focused assessment of sonography for trauma OR FAST OR emergency ultras*
-
18
(1 OR 2 OR 3 OR 4 OR 5 OR 6 OR 7 OR 8 OR 9 OR 10 OR 11 OR 12 OR 13 OR 14 OR 15) AND (16 OR 17)
-
19
Randomised controlled trial OR randomized controlled trial
-
20
Random allocation
-
21
Double blind method
-
22
Single blind method
-
23
(19 OR 20 OR 21 OR 22)
-
24
18 AND 23
Trials covered by EMBASE back to 1980 were tracked by
-
1
‘Intermethod comparison’/exp
-
2
‘Randomized controlled trial’/exp
-
3
‘Non invasive measurement’/exp
-
4
1 OR 2 OR 3
-
5
‘Peritoneal fluid’/exp
-
6
‘Hemoperitoneum’/exp
-
7
‘Spleen rupture’/exp
-
8
‘Spleen injury’/exp
-
9
‘Liver injury’/exp
-
10
‘Multiple trauma’/exp
-
11
‘Abdominal blunt trauma’/exp
-
12
‘Abdominal bleeding’/exp
-
13
‘Thoracic injury’/exp
-
14
‘Thoracic bleeding’/exp
-
15
5 OR 6 OR 7 OR 8 OR 9 OR 10 OR 11 OR 12 OR 13 OR 14
-
16
‘Peritoneum lavage’/exp
-
17
‘Clinical observation’/exp
-
18
‘Spiral computer assisted tomography’/exp
-
19
‘Diagnostic approach route’/exp
-
20
16 OR 17 OR 18 OR 10
-
21
‘Echography’/exp
-
22
‘Ultrasound scanner’/exp
-
23
‘Ultrasound transducer’/exp
-
24
21 OR 22 OR 23
-
25
4 AND 15 AND 20 AND 24
Electronic databases
The Cochrane Injuries Group Specialized Register and CENTRAL (the Cochrane Central Register of Controlled Trials) were searched, as were the databases of the publishers SpringerLink (including the journal Abdominal Imaging, Emergency Radiology), Elsevier (including the journal Annals of Emergency Medicine,), Wiley (including the journal Academic Emergency Medicine, British Journal of Surgery), Lippincott Williams and Wilkins (including the Journal of Trauma, Annals of Surgery, Critical Care Medicine, Shock, Journal of Computer Assisted Tomography). Finally, searches on web-based resources including the Radiological Society of North America (RSNA, covering the journals Radiology and Radiographics as well as the RSNA Index to Imaging Literature), trials registers (such as Current Controlled Trials) and Google were run. The reference lists of all retrieved articles were reviewed for further trials.
Abstract searching
Abstracts presented to the following international scientific societies were searched: Society for Academic Emergency Medicine (1999–2008), the American College of Emergency Physicians (1999–2008), the American Association for the Surgery of Trauma (1999–2007), and the World Congress on Ultrasound in Emergency and Critical Care Medicine (2005–2008).
Methods of the review: trial identification and selection
The titles or abstracts of all studies identified were assessed by the initial search and excluded clearly non-relevant studies. Full text articles were obtained for potentially relevant studies and any studies with unclear methodology. All these studies were assessed as to whether they met the inclusion criteria for this review, their method of randomization or quasi-randomization, and their adequacy of allocation concealment.
Data extraction
The author extracted the results of each included paper on a data extraction sheet.
Assessment of methodological quality
Each included trial was read for the following aspects of internal and external validity.
-
A.
Was the assigned treatment adequately concealed prior to allocation?
-
2 = method did not allow disclosure of assignment;
-
1 = small but possible chance of disclosure of assignment or unclear;
-
0 = quasi-randomized or open list/tables.
-
-
B.
Were the outcomes of patients/participants who withdrew described and included in the analysis (intention to treat)?
-
2 = withdrawals well described and accounted for in analysis;
-
1 = withdrawals described and analysis not possible;
-
0 = no mention, inadequate mention, or obvious differences and no adjustment.
-
-
C.
Were the outcome assessors blinded to the results of the index test (i.e., ultrasonography) and/or reference tests and/or patient outcome?
-
2 = effective action taken to blind assessors;
-
1 = small or moderate chance of unblinding of assessors;
-
0 = not mentioned or not possible.
-
-
D.
Were the treatment and control group comparable at entry?
-
2 = good comparability of groups, or confounding adjusted for in analysis;
-
1 = confounding small or mentioned but not adjusted for;
-
0 = large potential for confounding, or not discussed.
-
-
E.
Were care programs, other than the trial options, identical?
-
2 = care programs clearly identical;
-
1 = clear but trivial differences;
-
0 = not mentioned, or clear and important differences in care programs.
-
-
F.
Were the inclusion and exclusion criteria clearly defined?
-
2 = clearly defined;
-
1 = inadequately defined;
-
0 = not defined.
-
-
G.
Were the interventions clearly defined?
-
2 = clearly defined interventions are applied with a standardized protocol;
-
1 = clearly defined interventions are applied but the application protocol is not standardized;
-
0 = intervention and/or application protocol are poor or not defined.
-
-
H.
Were the outcome measures used clearly defined (by outcome)?
-
2 = clearly defined;
-
1 = inadequately defined;
-
0 = not defined.
-
-
I.
Was the surveillance active, and of clinically appropriate duration?
-
2 = active surveillance and appropriate duration;
-
1 = active surveillance, but inadequate duration;
-
0 = surveillance not active or not defined.
-
Data analysis
Mean differences and 95% confidence intervals were calculated for continuous variables. For dichotomous outcomes, proportions with 95% confidence intervals were calculated. Due to the heterogeneity of the data, meta-analyses and mixed regression modeling were not conducted.
Description of studies
The search delivered 487 citations of studies investigating the use of ultrasound in torso trauma. Since ultrasound findings prompted different forms of further investigation, care programs varied between groups. Most studies examined the diagnostic accuracy of ultrasonography to detect free intra-peritoneal fluid, leaving 160 studies for further screening.
Identified were 49 studies [3–52] that compared the effectiveness and efficiency of ultrasound-based clinical pathways to algorithms that did not incorporate ultrasound examinations. Thirty-eight of these were retrospective, did not define an allocation schema, or did not describe the operative findings nor describe the “false-negative cases” and were excluded from further analysis.
The 11 remaining trials were included in the formal review (See Table 1).
Methodological quality
The Melniker [3] study was a randomized clinical trial to primarily assess the effect of point-of-care, limited ultrasonography (PLUS) for trauma on the time to operative intervention; secondary outcomes included use of other diagnostics, hospital and ICU length of stay, and hospital charges. Regression models controlled for confounders and analyzed physician-to-physician variability. All analyses were conducted on an intention-to-treat basis. Results were presented as mean, first-quartile, median, and third-quartile with multiplicative change and 95% confidence intervals; or percentage with odds ratio and 95% confidence intervals. 444 patients with suspected torso trauma were eligible; 136 lacked consent and attendings refused enrollment of 46. 262 patients were enrolled: 135 PLUS and 127 controls; 45 patients were discharged from the ED or “Walked Out AMA”, leaving 111 PLUS and 106 Control patients in the final analysis. There were no baseline differences between groups. Time to OR was 64% (48, 76) less for PLUS compared to control patients. PLUS patients underwent fewer CT, Odds Ratio = 0.16 (0.07, 0.32), spent 27% (1, 46) fewer days in hospital, suffered fewer complications, Odds Ratio = 0.16 (0.07, 0.32), and charges were 35% (19, 48) less compared to control. The authors concluded that a PLUS-inclusive protocol significantly decreased time to OR in patients with suspected torso trauma, with improved resource utilization and lower charges.
One of the randomized trials [7] met some of the design standards. Patients were assigned by a computer-generated list, although it was not clear whether concealment was maintained. Sample size considerations called for 50 patients in each group to detect a 20% difference in CT scan use between groups. A secondary outcome (30-min difference in time to operative intervention) mandating inclusion of 420 patients was mentioned in the methods section of the original paper. However, no data were provided on this endpoint. A flowchart sketched the study profile according to the CONSORT recommendations.
Two other studies enrolled patients in a quasi-randomized fashion. The suitable algorithm was defined by ultrasound availability: ultrasound on weekdays from 8 a.m. to 5 p.m; no ultrasound on weekdays from 5 p.m. to 8 a.m. and on weekends [4] or the presence of one of the investigators [5]. Since no patient had the opportunity to influence the date of injury, these methods were considered proper random allocation.
In general, details of the study populations in the remaining 7 papers were sparse or missing.
Results
In the 11 studies included in the review, 2,755 patients were prospectively evaluated with Focused Assessment with Sonography in Trauma (FAST) and 448 (16%) went to operative intervention. The data demonstrated that for the detection of any amount of free fluid by ultrasound the sensitivity was 90.6% (95% CI) and the specificity was 98.6% (95% CI). As a screening tool to assess the “Need for OR”, the sensitivity was 94.2% (95% CI) and the specificity was 98.1% (95% CI).
The published reports indicated that 26 (5.8%) patients had false-negative FAST, but upon further review, 21 of these cases did not undergo operative intervention or the FAST was not done contemporaneously with the decision to operate, e.g., negative FAST on presentation and on Hospital Day-2 instability developed necessitating operation, which revealed hemoperitoneum. Two cases were associated with rare blunt trauma-induced small bowel perforation without hemoperitoneum, an injury type that CT is insensitive to identifying; and 3 FAST exams were technically poor and, therefore, uninterpretable resulting in a legitimate false-negative rate of 1.1 or 98.9% sensitivity for the “Need for OR”, when an adequate FAST exam was completed.
The debate at WCU2
Dr. Stengel, primary author of the Cochrane Review on FAST, was contacted in August 2005 and invited to attend the 2nd World Congress on Ultrasound in Emergency and Critical Care Medicine (WCU2) in June 2006 in New York City to debate the ““Emergency ultrasound-based algorithms for diagnosing blunt abdominal trauma (Review), from the Cochrane Collaboration.” The Congress organizers funded the air travel and accommodations in New York for Drs. Stengel, Bauwens, and Sehouli. Participants in the debate were Drs. Melniker (Chair, WCU2 Organizing Committee and Principal Investigator, SOAP-1 Trial), Dulchavsky (representing the American College of Surgeons), and Kirkpatrick (enhanced FAST investigator). On June 12, 2006, the Opening Plenary Session of WCU2 featured the debate of the Cochrane Review on FAST, which was digitally recorded.
Dr. Stengel and his colleagues presented the review and each speaker and several delegates to the Congress offered comments and posed questions. Key points from the session were that the review, while methodologically strong, did not evaluate all critical endpoints needed to judge the effectiveness of FAST. Dr. Stengel agreed to include the commentary from the debate and any new published data in all future updates of the Cochrane Review. Furthermore, it was agreed that more investigation was needed and, toward that end, it was desirable to establish a “FAST Registry” or build on existing registries, e.g., the National Trauma Data Bank of the American College of Surgeons, to include more FAST-related data points.
Cochrane Review of FAST: 2008 update
In January of 2008, the Cochrane Review of FAST was updated by Stengel et al. [53]. The update neither includes any methodological changes nor any new endpoints analyzed. There was no mention of the debate at WCU2 in New York or the need for a FAST Registry. Some limited aspects of the Melniker et al. [3] findings were presented, but it was erroneously stated that the data were analyzed in a manner “contradicting the intention-to-treat principle” and included the following statement: “We did not receive a response to our letter to the research team.”
The 2008 Update concluded: “There is currently insufficient evidence from RCTs to justify promotion of ultrasound-based clinical pathways in diagnosing patients with suspected blunt abdominal trauma.” The authors recommended widespread use of CT of the chest, abdomen, and pelvis for patients with blunt torso trauma.
The Cochrane Reviewers
The authors of the Cochrane Review on FAST are well published with over 100 citations, individually and collaboratively, but only 3 references for ultrasound-related investigations. None of the 3 ultrasound studies involved prospective investigations or any use of ultrasound by the authors; all are literature reviews with data-pooling and meta-analyses and each speak to a lack of methodological rigor in most studies of clinician-performed ultrasound for trauma.
Stengel et al. are qualified researchers, but lack professional investment in point-of-care testing, specifically, bedside ultrasound. They have demonstrated a predilection for the use of CT in their studies and recommendations.
Discussion
Many torso injuries do not require repair; therefore, operative intervention rather than the presence of free fluid or organ injury is the optimal endpoint for study. Although testing is normally thought of as identifying the presence of injury, not “need for treatment”, the unstated assumption is that all “injuries” require “treatment”, and it is clear that with torso injury, especially in the pediatric population, this is not the case. Likewise, after head CT, not all patients with subdural hemorrhage are taken to neurosurgery, but for the purpose of defining the effectiveness of CT, it is reasonable to ask whether all patients ultimately requiring neurosurgery are identified by a positive CT. What is essential to know is which patients require immediate operative intervention, the direct and not a proxy endpoint is preferred.
Need for operative intervention, as opposed to the decision to operate, can be objectively defined and determined prospectively or retrospectively. This allows determination of whether a positive FAST exam result accurately predicts those patients who require immediate OR from those who do not. The ways in which this result is integrated into the surgical decision-making process are, of course, subjective, because not all patients with positive FAST scans are taken to OR.
Indeed, a part of the impetus to bring ultrasound machines into the trauma bay in the first place was the high reported rates of non-therapeutic laparotomies caused by the oversensitivity of the diagnostic peritoneal lavage (DPL), in the range of 20–25%. This is probably a result of growing recognition of the ability of many intra-abdominal injuries to heal without surgical repair. It should be noted that no clear and consistent definition of non-therapeutic laparotomy has been reported. It is also apparent that there is a clinically relevant, albeit small, incidence of complications with DPL, many of which require surgical repair. FAST allows the grading of hemoperitoneum, a great improvement over the ‘Yes/No’ binary response from DPL.
The primary measure of accuracy of a screening test is its ability to “rule out” a disease process, characterized by sensitivity: a measure of false negativity. The results of this review demonstrate a sensitivity of 94.2%, with 422 of 448 ultrasound-screened patients who needed operative intervention having positive findings on their FAST scan. Twenty-one of the 26 patients without a positive scan had either delayed onset of internal bleeding, which is not a deficiency of FAST—it is designed to demonstrate pooling of blood in body cavities, not to predict future bleeding. Excluding “pseudo” false negatives in the sensitivity analysis enhances the rate of detection of “Need for OR” to 422 of 427 patients, or 98.9%. This figure is more representative of the true value of adequately completed FAST exams. Five patients who needed operative intervention were not identified on their FAST exams, which upon review 3 exams were found to be technically inadequate. The other 2 false-negative findings were in patients with rare blunt trauma-induced small bowel perforations without hemoperitoneum whose injuries were not of such severity as to make the delay of clinical significance and, interestingly, CT is also insensitive to detect these injuries. Although proponents of CT may argue that current results show better accuracy, the logistic difficulties and dangers of transport during the first few minutes after a trauma patient’s arrival are such that it is often not feasible as a screening test. The sensitivity of 94.2–98.9% found in this review compares favorably with CT results.
The specificity was 98.1% (2263 negative studies among 2,307 ultrasound-screened patients who did not require operative intervention). Thirty of the 44 patients whose FAST exam was judged clearly positive were found not to require operative intervention. Only 14 (3.0%) patients with positive FAST exams resulted in non-therapeutic laparotomies, and 7 of them had significant hemoperitoneum. This is notably better than the rates reported for DPL.
Trauma to the torso is a dynamic process; occult injuries may evolve. FAST allows monitoring of deterioration due to the ability to conduct serial exams at the point-of-care, in the emergency department, operative suite, and in the hospital. Hemoperitoneum Scoring Systems such as the University of Miami/McKenney Score have been developed and validated. DPL is more difficult to repeat and is not reliably quantifiable, but may have lingering utility when small bowel perforation is suspected. Repeat CT scans are logistically difficult and somewhat dangerous in view of the need to move the patient out of the resuscitation suite.
The FAST examination is the logical choice for screening for the “Need for OR” in patients with possible torso injury due to blunt trauma. Finally, while in developed countries CT is generally available, in most of the world this kind of advanced imaging is virtually non-existent. Therefore, on a global basis, the expansion of portable ultrasound use, clinician-performed at the point-of-care for trauma victims, represents a low-cost, high-technology solution.
References
Stengel D, Bauwens K, Sehouli J, Rademacher G, Mutze S, Ekkernkamp A, Porzsolt F (2005) Emergency ultrasound-based algorithms for diagnosing blunt abdominal trauma]. [Review] [40 refs] Cochrane Database Syst Rev 2:CD004446
National Trauma Data Bank of the American College of Surgeons. Accessed at http://www.facs.org/trauma/ntdb/index.html on multiple occasions
Melniker LA, Liebner E, McKenney MG, Lopez P, Briggs WM, Mancuso MA (2006) Randomized controlled clinical trial of point-of-care, limited ultrasonography (PLUS) for Trauma in the Emergency Department: the First Sonography Outcomes Assessment Program (SOAP-1) trial. Ann Emerg Med 48(3):227–235
Arrillaga A, Graham R, York JW, Miller RS (1999) Increased efficiency and cost-effectiveness in the evaluation of the blunt abdominal trauma patient with the use of ultrasound. Am Surg 65(1):31–35
Boulanger BR, Brenneman FD, McLellan BA, Rizoli SB, Culhane J, Hamilton P (1995) A prospective study of emergent abdominal sonography after blunt trauma. J Trauma Injury Infect Crit Care 39(2):325–330
Rose JS (2004) Ultrasound in abdominal trauma. Emerg Med Clin North Am 22(3):581–599 [Review] [61 refs], vii
Ma OJ, Kefer MP, Stevison KF, Mateer JR (2001) Operative versus nonoperative management of blunt abdominal trauma: role of ultrasound-measured intraperitoneal fluid levels. Am J Emerg Med 19(4):284–286
Akgur FM, Aktug T, Olguner M, Kovanlikaya A, Hakguder G (1997) Prospective study investigating routine usage of ultrasonography as the initial diagnostic modality for the evaluation of children sustaining blunt abdominal trauma. J Trauma Injury Infect Crit Care 42(4):626–628
McElveen TS, Collin GR (1997) The role of ultrasonography in blunt abdominal trauma: a prospective study. Am Surg 63(2):184–188
Healey MA, Simons RK, Winchell RJ, Gosink BB, Casola G, Steele JT, Potenza BM, Hoyt DB (1996) A prospective evaluation of abdominal ultrasound in blunt trauma: is it useful? J Trauma Injury Infect Crit Care 40(6):875–883 (discussion 883–885)
Rozycki GS (1995) Abdominal ultrasonography in trauma. Surg Clin N Am 75(2):175–191 [Review] [33 refs]
Goletti O, Ghiselli G, Lippolis PV, Chiarugi M, Braccini G, Macaluso C, Cavina E (1994) The role of ultrasonography in blunt abdominal trauma: s in 250 consecutive cases. J Trauma Injury Infect Crit Care 36(2):178–181
Liu M, Lee CH, P’eng FK (1993) Prospective comparison of diagnostic peritoneal lavage, computed tomographic scanning, and ultrasonography for the diagnosis of blunt abdominal trauma. J Trauma Injury Infect Crit Care 35(2):267–270
Gruessner R, Mentges B, Duber C, Ruckert K, Rothmund M (1989) Sonography versus peritoneal lavage in blunt abdominal trauma. J Trauma Injury Infect Crit Care 29(2):242–244
Stengel D, Bauwens K, Porzsolt F, Rademacher G, Mutze S, Ekkernkamp A (2005) Association between compliance with methodological standards of diagnostic research and reported test accuracy: meta-analysis of FAST, 2005. Zentralbl Chir 130(12):1027–1037 [German]
Stengel D, Bauwens K, Sehouli J, Porzsolt F, Rademacher G, Mutze S, Ekkernkamp A (2001) Systematic review and meta-analysis of emergency ultrasonography for blunt abdominal trauma. Br J Surg 88(7):901–912 [Review] [80 refs]
Jalli R, Kamalzadeh N, Lotfi M, Farahangiz S, Salehipour M (2009) Accuracy of sonography in detection of renal injuries caused by blunt abdominal trauma: a prospective study. Turkish J of Trauma Emerg Surg TJTES 15(1):23–27
Browning JG, Wilkinson AG, Beattie T (2008) Imaging paediatric blunt abdominal trauma in the emergency department: ultrasound versus computed tomography. Emerg Med J 25(10):645–648
Helling TS, Wilson J, Augustosky K (2007) The utility of focused abdominal ultrasound in blunt abdominal trauma: a reappraisal. Am J Surg 194(6):728–732 (discussion 732–733)
Holmes JF, Gladman A, Chang CH (2007) Performance of abdominal ultrasonography in pediatric blunt trauma patients: a meta-analysis. J Pediatr Surg 42(9):1588–1594 [Review] [48 refs]
Griffin XL, Pullinger R (2007) Are diagnostic peritoneal lavage or focused abdominal sonography for trauma safe screening investigations for hemodynamically stable patients after blunt abdominal trauma? A review of the literature. J Trauma Injury Infect Crit Care 62(3):779–784 [Review] [44 refs]
Lee BC, Ormsby EL, McGahan JP, Melendres GM, Richards JR (2007) The utility of sonography for the triage of blunt abdominal trauma patients to exploratory laparotomy. Am J Roentgenol 188(2):415–421
Kirkpatrick AW, Sirois M, Laupland KB, Goldstein L, Brown DR, Simons RK, Dulchavsky S, Boulanger BR (2005) Prospective evaluation of hand-held focused abdominal sonography for trauma (FAST) in blunt abdominal trauma. Can J Surg 48(6):453–460
Nural MS, Yardan T, Guven H, Baydin A, Bayrak IK, Kati C (2005) Diagnostic value of ultrasonography in the evaluation of blunt abdominal trauma. Diagn Interv Radiol 11(1):41–44
Helling TS, Wilson J, Augustosky K (2007) The utility of focused abdominal ultrasound in blunt abdominal trauma: a reappraisal. Am J Surg 194(6):728–732 (discussion 732–733)
Tas F, Ceran C, Atalar MH, Bulut S, Selbes B, Isik AO (2004) The efficacy of ultrasonography in hemodynamically stable children with blunt abdominal trauma: a prospective comparison with computed tomography. Eur J Radiol 51(1):91–96
Suthers SE, Albrecht R, Foley D, Mantor PC, Puffinbarger NK, Jones SK, Tuggle DW (2004) Surgeon-directed ultrasound for trauma is a predictor of intra-abdominal injury in children. Am Surg 70(2):164–167 (discussion 167–168)
Murphy R, Ghosh A (2002) Towards evidence based emergency medicine: best BETs from Manchester royal infirmary: ultrasound or computed tomography in paediatric blunt abdominal trauma. Emerg Med J 19(6):554–556
McKenney MG, McKenney KL, Hong JJ, Compton R, Cohn SM, Kirton OC, Shatz DV, Sleeman D, Byers PM, Ginzburg E, Augenstein J (2001) Evaluating blunt abdominal trauma with sonography: a cost analysis. Am Surg 67(10):930–934
Foo E, Su JW, Menon D, Tan D, Chan ST (2001) A prospective evaluation of surgeon performed sonography as a screening test in blunt abdominal trauma. Ann Acad Med Singap 30(1):11–14
Henderson SO, Sung J, Mandavia D (2000) Serial abdominal ultrasound in the setting of trauma. J Emerg Med 18(1):79–81
McKenney KL (1999) Ultrasound of blunt abdominal trauma. Radiologic Clin North Am 37(5):879–893 [Review] [34 refs]
Teitelbaum DH (1999) Ultrasound is an effective triage tool to evaluate blunt abdominal trauma in the pediatric population. J Trauma Injury Infect Crit Care 46(2):357–359
Abu-Zidan FM, Sheikh M, Jadallah F, Windsor JA (1999) Blunt abdominal trauma: comparison of ultrasonography and computed tomography in a district general hospital. Aust Radiol 43(4):440–443
Bode PJ, Edwards MJ, Kruit MC, van Vugt AB (1999) Sonography in a clinical algorithm for early evaluation of 1,671 patients with blunt abdominal trauma. Am J Roentgenol 172(4):905–911
Richards JR (1998) Ultrasound versus CT in evaluating blunt abdominal trauma. West J Med 169(5):288–289
McKenney KL, Nunez DB Jr, McKenney MG, Asher J, Zelnick K, Shipshak D (1998) Sonography as the primary screening technique for blunt abdominal trauma: experience with 899 patients. Am J Roentgenol 170(4):979–985
Bennett MK, Jehle D (1997) Ultrasonography in blunt abdominal trauma. Emerg Med Clin North Am 15(4):763–787 [Review] [46 refs]
Branney SW, Moore EE, Cantrill SV, Burch JM, Terry SJ (1997) Ultrasound based key clinical pathway reduces the use of hospital res for the evaluation of blunt abdominal trauma. J Trauma Injury Infect Crit Care 42(6):1086–1090
Nordenholz KE, Rubin MA, Gularte GG, Liang HK (1997) Ultrasound in the evaluation and management of blunt abdominal trauma. Ann Emerg Medicine 29(3):357–366 [Review] [51 refs]
Abu-Zidan FM, Zayat I, Sheikh M, Mousa I, Behbehani A (1996) Role of ultrasonography in blunt abdominal trauma: a prospective study. Eur J Surg 162(5):361–365 [Review] [19 refs]
Bode PJ, Niezen RA, van Vugt AB, Schipper J (1993) Abdominal ultrasound as a reliable indicator for conclusive laparotomy in blunt abdominal trauma. J Trauma Injury Infect Crit Care 34(1):27–31
Feliciano DV (1991) Diagnostic modalities in abdominal trauma: peritoneal lavage, ultrasonography, computed tomography scanning, and arteriography. Surg Clin North Am 71(2):241–256 [Review] [71 refs]
Thal ER, Meyer DM (1991) The evaluation of blunt abdominal trauma: computed tomography scan, lavage, or sonography? Adv Surg 24:201–228 [Review] [82 refs]
Wening JV (1989) Evaluation of ultrasound, lavage, and computed tomography in blunt abdominal trauma. Surg Endosc 3(3):152–158
Krettek C (2008) Ultrasound for abdominal and thorax trauma. Unfallchirurg 111(12):957 [German]
Svinos H (2009) Best BETs from the Manchester Royal Infirmary. BET 1 using ultrasound to detect peritoneal fluid in a pregnant patient with abdominal trauma. Emerg Med J 26(3):201–202 [Review] [3 refs]
Moriwaki Y, Sugiyama M, Toyoda H, Kosuge T, Arata S, Iwashita M, Tahara Y, Suzuki N (2009) Ultrasonography for the diagnosis of intraperitoneal free air in chest-abdominal-pelvic blunt trauma and critical acute abdominal pain. Arch Surg 144(2):137–141 discussion 142
Clevert DA, Weckbach S, Minaifar N, Clevert DA, Stickel M, Reiser M (2008) Contrast-enhanced ultrasound versus MS-CT in blunt abdominal trauma. Clinical Hemorheol Microcirculation 39(1–4):155–169
Vosburgh KG, Stoll J, Noble V, Pohl K, San Jose Estepar R, Takacs B (2008) Image registration assists novice operators in ultrasound assessment of abdominal trauma. Studies Health Technol Inform 132:532–537
Zagrodsky V, Phelan M, Shekhar R (2007) Automated detection of a blood pool in ultrasound images of abdominal trauma. Ultrasound Med Biol 33(11):1720–1726
Bhan C, Forshaw MJ, Bew DP, Kapadia YK (2007) Diagnostic peritoneal lavage and ultrasonography for blunt abdominal trauma: attitudes and training of current general surgical trainees. Eur J Emerg Med 14(4):212–215
Stengel D, Bauwens K, Sehouli J, Rademacher G, Mutze S, Ekkernkamp A, Porzsolt F (2008) Emergency ultrasound-based algorithms for diagnosing blunt abdominal trauma. Cochrane Database Syst Rev Issue 1. Art. No.: CD004446. doi:10.1002/14651858.CD004446.pub2. http://www.cochrane.org/reviews/en/ab004446.html. Accessed 15 Feb 2008
Suggested readings
Valentino M, Serra C, Pavlica P, Barozzi L (2007) Contrast-enhanced ultrasound for blunt abdominal trauma. Semin Ultrasound CT & MR 28(2):130–140 [Review] [39 refs]
Menaker J, Cushman J, Vermillion JM, Rosenthal RE, Scalea TM (2007) Ultrasound-diagnosed cardiac tamponade after blunt abdominal trauma-treated with emergent thoracotomy. J Emerg Med 32(1):99–103
Gales H, Perry M (2006) Is there a role for planned serial chest radiographs and abdominal ultrasound scans in the resuscitation room following trauma? Ann R Coll Surg Engl 88(6):535–539
McGahan JP, Horton S, Gerscovich EO, Gillen M, Richards JR, Cronan MS, Brock JM, Battistella F, Wisner DH, Holmes JF (2006) Appearance of solid organ injury with contrast-enhanced sonography in blunt abdominal trauma: preliminary experience. Am J Roentgenol 187(3):658–666
Valentino M, Serra C, Zironi G, De Luca C, Pavlica P, Barozzi L (2006) Blunt abdominal trauma: emergency contrast-enhanced sonography for detection of solid organ injuries. Am J Roentgenol 186(5):1361–1367
Moriwaki Y, Sugiyama M, Toyoda H, Kosuge T, Takahashi K, Iwashita M, Matsuzaki S, Tahara Y, Suzuki N (2006) Monitoring and evaluation of intraperitoneal bleeding (IPB) by small portable ultrasonography during transcatheter arterial embolization (TAE) in abdominal-pelvic trauma patients with shock: as a monitor for early detection of increase of IPB. Hepatogastroenterology 53(68):175–178
Walcher F, Weinlich M, Conrad G, Schweigkofler U, Breitkreutz R, Kirschning T, Marzi I (2006) Prehospital ultrasound imaging improves management of abdominal trauma. Br J Surg 93(2):238–242
Soundappan SV, Holland AJ, Cass DT, Lam A (2005) Diagnostic accuracy of surgeon-performed focused abdominal sonography (FAST) in blunt paediatric trauma. Injury 36(8):970–975
Rose JS, Richards JR, Battistella F, Bair AE, McGahan JP, Kuppermann N (2005) The fast is positive, now what? Derivation of a clinical decision rule to determine the need for therapeutic laparotomy in adults with blunt torso trauma and a positive trauma ultrasound. J Emerg Med 29(1):15–21
Bari V, Ashraf K, Rafique MZ, Usman MU (2005) Focused abdominal ultrasound for blunt abdominal trauma. J Coll Phys Surg Pak 15(5):315–316
Bakker J, Genders R, Mali W, Leenen L (2005) Sonography as the primary screening method in evaluating blunt abdominal trauma. J Clin Ultrasound 33(4):155–163
Brown MA, Sirlin CB, Farahmand N, Hoyt DB, Casola G (2005) Screening sonography in pregnant patients with blunt abdominal trauma. J Ultrasound Med 24(2):175–181 quiz 183–184
Sato M, Yoshii H (2004) Reevaluation of ultrasonography for solid-organ injury in blunt abdominal trauma. J Ultrasound Med 23(12):1583–1596
Boysen SR, Rozanski EA, Tidwell AS, Holm JL, Shaw SP, Rush JE (2004) Evaluation of a focused assessment with sonography for trauma protocol to detect free abdominal fluid in dogs involved in motor vehicle accidents. J Am Veterinary Med Assoc 225(8):1198–1204
Massarutti D, Berlot G, Saltarini M, Trillo G, D’Orlando L, Pessina F, Modesto A, Meduri S, Da Ronch T, Carchietti E (2004) Abdominal ultrasonography and chest radiography are of limited value in the emergency room diagnostic work-up of severe trauma patients with hypotension on the scene of accident. Radiol Med 108(3):218–224
Scaglione M (2004) The use of sonography versus computed tomography in the triage of blunt abdominal trauma: the European perspective. Emerg Radiol 10(6):296–298
Rhea JT, Garza DH, Novelline RA (2004) Controversies in emergency radiology. CT versus ultrasound in the evaluation of blunt abdominal trauma. Emerg Radiol 10(6):289–295 [Review] [55 refs]
Kirkpatrick AW, Sirois M, Ball CG, Laupland KB, Goldstein L, Hameed M, Brown DR, Simons RK, Kortbeek J, Dulchavsky S, Boulanger BB (2004) The hand-held ultrasound examination for penetrating abdominal trauma. Am J Surg 187(5):660–665
Holmes JF, Harris D, Battistella FD (2004) Performance of abdominal ultrasonography in blunt trauma patients with out-of-hospital or emergency department hypotension. Ann Emerg Med 43(3):354–361
Soudack M, Epelman M, Maor R, Hayari L, Shoshani G, Heyman-Reiss A, Michaelson M, Gaitini D (2004) Experience with focused abdominal sonography for trauma (FAST) in 313 pediatric patients. J Clin Ultrasound 32(2):53–61
Brown MA, Sirlin CB, Hoyt DB, Casola G (2003) Screening ultrasound in blunt abdominal trauma. J Int Care Med 18(5):253–260 [Review] [39 refs]
Staunton M, Malone DE (2003) Ultrasonography or computed tomography for diagnosis in hemodynamically stable patients with recent blunt abdominal trauma? Can Assoc Radiol J 54(5):279–280
Musa HA (2003) Ultrasound as a primary tool to evaluate patients with blunt abdominal trauma. Saudi Med J 24(7):793–794
Al-Salamah SM, Mirza SM, Ahmad SN, Khalid K (2002) Role of ultrasonography, computed tomography and diagnostic peritoneal lavage in abdominal blunt trauma. Saudi Med J 23(11):1350–1355
Stassen NA, Lukan JK, Carrillo EH, Spain DA, Norfleet LA, Miller FB, Polk HC Jr (2002) Examination of the role of abdominal computed tomography in the evaluation of victims of trauma with increased aspartate aminotransferase in the era of focused abdominal sonography for trauma. Surgery 132(4):642–646 (discussion 646–647)
McGahan JP, Richards J, Gillen M (2002) The focused abdominal sonography for trauma scan: pearls and pitfalls. J Ultrasound Med 21(7):789–800 [Review] [45 refs]
Brooks A, Davies B, Connolly J (2002) Prospective evaluation of handheld ultrasound in the diagnosis of blunt abdominal trauma. J Royal Army Med Corps 148(1):19–21
Holmes JF, Brant WE, Bond WF, Sokolove PE, Kuppermann N (2001) Emergency department ultrasonography in the evaluation of hypotensive and normotensive children with blunt abdominal trauma. J Pediatr Surg 36(7):968–973
Brown MA, Casola G, Sirlin CB, Hoyt DB (2001) Importance of evaluating organ parenchyma during screening abdominal ultrasonography after blunt trauma. J Ultrasound Med 20(6):577–583 quiz 585
Blaivas M (2001) Triage in the trauma bay with the focused abdominal sonography for trauma (FAST) examination. J Emerg Med 21(1):41–44
Fernandez Cordoba MS, Gonzalvez Pinera J, Puertas Hernandez F, Marco Macian A (2001) Usefulness of ultrasonography in the initial assessment of blunt abdominal trauma in children]. Cirugia Pediatrica 14(1):9–13 [Spanish]
Sirlin CB, Casola G, Brown MA, Patel N, Bendavid EJ, Hoyt DB (2001) Quantification of fluid on screening ultrasonography for blunt abdominal trauma: a simple scoring system to predict severity of injury. J Ultrasound Med 20(4):359–364
Sirlin CB, Casola G, Brown MA, Patel N, Bendavid EJ, Hoyt DB (2001) Patterns of fluid accumulation on screening ultrasonography for blunt abdominal trauma: comparison with site of injury. J Ultrasound Med 20(4):351–357
Goodwin H, Holmes JF, Wisner DH (2001) Abdominal ultrasound examination in pregnant blunt trauma patients. J Trauma Injury Infect Crit Care 50(4):689–693 discussion 694
Udobi KF, Rodriguez A, Chiu WC, Scalea TM (2001) Role of ultrasonography in penetrating abdominal trauma: a prospective clinical study. J Trauma Injury Infect Crit Care 50(3):475–479
Pershad J, Gilmore B (2000) Serial bedside emergency ultrasound in a case of pediatric blunt abdominal trauma with severe abdominal pain. Pediatr Emerg Care 16(5):375–376
Benya EC, Lim-Dunham JE, Landrum O, Statter M (2000) Abdominal sonography in examination of children with blunt abdominal trauma. Am J Roentgenol 174(6):1613–1616
Coley BD, Mutabagani KH, Martin LC, Zumberge N, Cooney DR, Caniano DA, Besner GE, Groner JI, Shiels WE 2nd (2000) Focused abdominal sonography for trauma (FAST) in children with blunt abdominal trauma. J Trauma Injury Infect Crit Care 48(5):902–906
Herman M, el Sheikh H (2000) The role of emergent sonography after blunt abdominal trauma. Am J Roentgenol 174(2):570–571
Buhne KH (999) Pitfalls in ultrasound diagnosis of acute abdominal trauma. Rontgenpraxis 52(3/4):110–117 [Review] [13 refs] [German]
Nilsson A, Loren I, Nirhov N, Lindhagen T, Nilsson P (1999) Power Doppler ultrasonography: alternative to computed tomography in abdominal trauma patients. J Ultrasound Med 18(10):669–672
Mutabagani KH, Coley BD, Zumberge N, McCarthy DW, Besner GE, Caniano DA, Cooney DR (1999) Preliminary experience with focused abdominal sonography for trauma (FAST) in children: is it useful? J Pediatr Surg 34(1):48–52 (discussion 52–54)
Patel JC, Tepas JJ 3rd (1999) The efficacy of focused abdominal sonography for trauma (FAST) as a screening tool in the assessment of injured children. J Pediatr Surg 34(1):44–47 (discussion 52−54)
Yeo A, Wong CY, Soo KC (1999) Focused abdominal sonography for trauma (FAST). Ann Acad Med Singap 28(6):805–809
Akgur FM, Olguner M, Aktug T (1999) Investigating the effectiveness of ultrasound as a triage tool to evaluate blunt abdominal trauma in children. J Trauma Injury Infect Crit Care 47(6):1162–1163 [Review] [13 refs]
Porras-Ramirez G, Ramirez-Reyes F, Hernandez-Herrera MH, Porras-Hernandez JD (1999) Clinical recognition and management of pediatric blunt abdominal trauma without ultrasound or computed tomography scan in community hospitals in Mexico. J Pediatr Surg 34(11):1700–1702
McGahan JP, Richards JR (1999) Blunt abdominal trauma: the role of emergent sonography and a review of the literature. Am J Roentgenol 172(4):897–903 [Review] [28 refs]
Tumbarello C (1998) Ultrasound evaluation of abdominal trauma in the emergency department. J Trauma Nurs 5(3):67–72 [Review] [21 refs], quiz 79–80
Fernandez L, McKenney MG, McKenney KL, Cohn SM, Feinstein A, Senkowski C, Compton RP, Nunez D (1998) Ultrasound in blunt abdominal trauma. J Trauma Injury Infect Crit Care 45(4):841–848 [Review] [53 refs]
Partrick DA, Bensard DD, Moore EE, Terry SJ, Karrer FM (1998) Ultrasound is an effective triage tool to evaluate blunt abdominal trauma in the pediatric population. J Trauma Injury Infect Crit Care 45(1):57–63
Yoshii H, Sato M, Yamamoto S, Motegi M, Okusawa S, Kitano M, Nagashima A, Doi M, Takuma K, Kato K, Aikawa N (1998) Usefulness and limitations of ultrasonography in the initial evaluation of blunt abdominal trauma. J Trauma Injury Infect Crit Care 45(1):45–50 (discussion 50–51)
Bain IM, Kirby RM, Tiwari P, McCaig J, Cook AL, Oakley PA, Templeton J, Braithwaite M (1998) Survey of abdominal ultrasound and diagnostic peritoneal lavage for suspected intra-abdominal injury following blunt trauma. Injury 29(1):65–71
McKenney MG, McKenney KL, Compton RP, Namias N, Fernandez L, Levi D, Arrillaga A, Lynn M, Martin L (1998) Can surgeons evaluate emergency ultrasound scans for blunt abdominal trauma? J Trauma Injury Infect Crit Care 44(4):649–653
Thourani VH, Pettitt BJ, Schmidt JA, Cooper WA, Rozycki GS (1998) Validation of surgeon-performed emergency abdominal ultrasonography in pediatric trauma patients. J Pediatr Surg 33(2):322–328
Singh G, Arya N, Safaya R, Bose SM, Das KM, Khanna SK (1997) Role of ultrasonography in blunt abdominal trauma. Injury 28(9/10):667–670
Raum MR, Bouillon B, Eypasch E, Tiling T (1997) Technology assessment of ultrasound in acute diagnosis of blunt abdominal trauma. Langenbecks Archiv fur Chirurgie Suppl Kongressband 114:461–464 [Review] [5 refs] [German]
Kluger Y, Soffer D (1997) Abdominal injuries without hemoperitoneum: a potential limitation of focused abdominal sonography for trauma (FAST). J Trauma Injury Infect Crit Care 43(4):728
McGahan JP, Rose J, Coates TL, Wisner DH, Newberry P (1997) Use of ultrasonography in the patient with acute abdominal trauma. J Ultrasound Med 16(10):653–662 quiz 663-664
Givre S, Kessler S (1997) The evaluation of blunt abdominal trauma: the evolving role of ultrasound. Mount Sinai J Med 64(4/5):311–315 [Review] [23 refs]
Chiu WC, Cushing BM, Rodriguez A, Ho SM, Mirvis SE, Shanmuganathan K, Stein M (1997) Abdominal injuries without hemoperitoneum: a potential limitation of focused abdominal sonography for trauma (FAST). J Trauma Injury Infect Crit Care 42(4):617–623 (discussion 623–625)
Krupnick AS, Teitelbaum DH, Geiger JD, Strouse PJ, Cox CS, Blane CE, Polley TZ (1997) Use of abdominal ultrasonography to assess pediatric splenic trauma. Potential pitfalls in the diagnosis. Ann Surg 225(4):408–414
Thomas B, Falcone RE, Vasquez D, Santanello S, Townsend M, Hockenberry S, Innes J, Wanamaker S (1997) Ultrasound evaluation of blunt abdominal trauma: program implementation, initial experience, and learning curve. J Trauma Injury Infect Crit Care 42(3):384–388 (discussion 388–390)
Wherrett LJ, Boulanger BR, McLellan BA, Brenneman FD, Rizoli SB, Culhane J, Hamilton P (1996) Hypotension after blunt abdominal trauma: the role of emergent abdominal sonography in surgical triage. J Trauma Injury Infect Crit Care 41(5):815–820
Ingeman JE, Plewa MC, Okasinski RE, King RW, Knotts FB (1996) Emergency physician use of ultrasonography in blunt abdominal trauma. Acad Emerg Med 3(10):931–937
Katz S, Lazar L, Rathaus V, Erez I (1996) Can ultrasonography replace computed tomography in the initial assessment of children with blunt abdominal trauma? J Pediatr Surg 31(5):649–651
Boulanger BR, McLellan BA, Brenneman FD, Wherrett L, Rizoli SB, Culhane J, Hamilton P (1996) Emergent abdominal sonography as a screening test in a new diagnostic algorithm for blunt trauma. J Trauma Injury Infect Crit Care 40(6):867–874
Pearl WS, Todd KH (1996) Ultrasonography for the initial evaluation of blunt abdominal trauma: a review of prospective trials. Ann Emerg Med 27(3):353–361 [Review] [36 refs]
Hahn H, Farber D, Spitzer I (1995) Blunt abdominal trauma in childhood. Value of conventional radiologic and ultrasound diagnosis. Radiologe 35(6):391–396 [Review] [29 refs] [German]
Glaser K, Tschmelitsch J, Klingler P, Wetscher G, Bodner E (1994) Ultrasonography in the management of blunt abdominal and thoracic trauma. Arch Surg 129(7):743–747
Akgur FM, Aktug T, Kovanhkaya A, Erdag G, Olguner M, Hosgor M, Obuz O (1993) Initial evaluation of children sustaining blunt abdominal trauma: ultrasonography vs. diagnostic peritoneal lavage. Eur J Pediatr Surg 3(5):278–280
Meenen NM, Dallek M, Tesch C, Wening JV, Lambrecht W, Jungbluth KH (1993) Sonography of blunt abdominal trauma within the scope of pediatric polytrauma. Chirurg 64(11):849–851 [Review] [15 refs] [German]
Conrad LC (1993) Ultrasonography in blunt abdominal trauma. West J Med 159(5):594
Jehle D, Guarino J, Karamanoukian H (1993) Emergency department ultrasound in the evaluation of blunt abdominal trauma. Am J Emerg Med 11(4):342–346
Forester D (1993) Abdominal ultrasound as a reliable indicator for conclusive laparotomy in blunt abdominal trauma. J Trauma Injury Infect Crit Care 35(3):492
Stylianos S (1993) Commentary: the role of sonography in the initial evaluation of children after blunt abdominal trauma. Pediatr Radiol 23(3):164
Luks FI, Lemire A, St-Vil D, Di Lorenzo M, Filiatrault D, Ouimet A (1993) Blunt abdominal trauma in children: the practical value of ultrasonography. J Trauma Injury Infect Crit Care 34(5):607–610 (discussion 610–611)
Rothlin MA, Naf R, Amgwerd M, Candinas D, Frick T, Trentz O (1993) Ultrasound in blunt abdominal and thoracic trauma. J Trauma Injury Infect Crit Care 34(4):488–495
Forster R, Pillasch J, Zielke A, Malewski U, Rothmund M (1993) Ultrasonography in blunt abdominal trauma: influence of the investigators’ experience. J Trauma Injury Infect Crit Care 34(2):264–269
Rothlin M, Naf R, Amgwerd M, Candinas D, Trentz O (1992) How much experience is required for ultrasound diagnosis of blunt abdominal trauma? Langenbecks Archiv fur Chirurgie 377(4):211–215 [German]
Riesener KP, Schumpelick V (1992) Ultrasound diagnosis in abdominal trauma–how much experience does the surgeon need to perform ultrasonic diagnosis? Langenbecks Archiv fur Chirurgie 377(4):205–206 [German]
Schnarkowski P, Brecht-Krauss D, Goldmann A, Friedrich JM, Limmer J (1992) Abdominal sonography in primary diagnosis of blunt abdominal trauma. Ultraschall Med 13(3):102–105 [German]
Tso P, Rodriguez A, Cooper C, Militello P, Mirvis S, Badellino MM, Boulanger BR, Foss FA Jr, Hinson DM, Mighty HE (1992) Sonography in blunt abdominal trauma: a preliminary progress report. J Trauma Injury Infect Crit Care 33(1):39–43 (discussion 43–44)
Hoffmann R, Nerlich M, Muggia-Sullam M, Pohlemann T, Wippermann B, Regel G (1992) Tscherne H. Blunt abdominal trauma in cases of multiple trauma evaluated by ultrasonography: a prospective analysis of 291 patients. J Trauma Injury Infect Crit Care 32(4):452–458
Barth JA (1991) Blunt abdominal trauma: diagnostic peritoneal lavage and/or ultrasound examination? Zentralbl Chir 116(2):125–127 [German]
Lara JR, Rojas M, Garassini MA, Nieves M (1989) Ultrasonography as diagnostic method in abdominal trauma and wounds. Gen 43(4):272–275 [Spanish]
Liess S, Baier A (1989) Ultrasound detection of vascular rupture of the intestine following blunt abdominal trauma. [German] Zentralblatt fur Chirurgie 114(22):1471–1472
Langfeldt S, Pedersen PR, Nepper-Rasmussen J (1989) Diagnosis of retroperitoneal air using ultrasound and radiology in duodenal rupture after blunt abdominal trauma. Rontgen-Blatter 42(11):478–479 [German]
Narain H, Talwar S, Kapoor R, Rana BS (1989) Role of ultrasound in the evaluation of blunt abdominal trauma. Ind Pediatr 26(6):539–543
Hoffmann R, Pohlemann T, Wippermann B, Reimer P, Milbradt H, Tscherne H (1989) Management of sonography in blunt abdominal trauma. Unfallchirurg 92(10):471–476 [German]
Kohlberger EJ, Ruf G, Lausen M, Haring R Jr (1989) Significance of ultrasonic-guided pleural punctures/thoracic drainage after abdominal procedures and blunt abdominal/thoracic trauma. Helvetica Chirurgica Acta 56(1/2):155–157 [German]
Kohlberger EJ, Strittmatter B, Waninger J (1989) Ultrasound diagnosis following blunt abdominal trauma. Sonography in acute and follow-up diagnosis. Fortschritte der Medizin 107(11):244–247 [Review] [17 refs] [German]
Chambers JA, Pilbrow WJ (1988) Ultrasound in abdominal trauma: an alternative to peritoneal lavage. Arch Emerg Med 5(1):26–33
Filiatrault D, Longpre D, Patriquin H, Perreault G, Grignon A, Pronovost J, Boisvert J (1987) Investigation of childhood blunt abdominal trauma: a practical approach using ultrasound as the initial diagnostic modality. Pediatr Radiol 17(5):373–379
Schiller K, Funk EM, Pfeifer KJ, Schweiberer L (1987) Value of sonography in blunt abdominal trauma. A contribution based on an animal experiment study. Unfallchirurg 90(5):246–250 [German]
Peiper HJ, Schmid A, Steffens H, Tiling T (1987) Ultrasound diagnosis in acute abdomen and blunt abdominal trauma. Chirurg 58(4):189–198 [German]
Hoelzer DJ, Brian MB, Balsara VJ, Varner WD, Flynn TC, Miner ME (1986) Selection and nonoperative management of pediatric blunt trauma patients: the role of quantitative crystalloid resuscitation and abdominal ultrasonography. J Trauma Injury Infect Crit Care 26(1):57–62
Hager J, Egender G (1985) Value of sonography for acute diagnosis and for further examination of blunt abdominal trauma in children. Rofo: Fortschritte auf dem Gebiete der Rontgenstrahlen und der Nuklearmedizin 143(1):44–48 [German]
Kuligowska E, Mueller PR, Simeone JF, Fine C (1984) Ultrasound in upper abdominal trauma. Semin Roentgenol 19(4):281–295
Klels E, Pringot J, Dardenne AN, Dautrebande J, Coppens JP (1983) Computed tomography in abdominal and thoracic trauma; comparative evaluation with abdominal ultrasonography and chest radiography. J Belge de Radiologie 66(1):31–38 [French]
Kuhn FP, Schreyer T, Schild H, Klose K, Gunther R (1983) Sonography in blunt abdominal trauma. Rofo: Fortschritte auf dem Gebiete der Rontgenstrahlen und der Nuklearmedizin 139(3):310–313 [German]
Hauenstein KH, Wimmer B, Billmann P, Noldge G, Zavisic D (1982) Sonography of blunt abdominal trauma (author’s transl)]. [German] Radiologe. 22(3):106–111
Kaude JV, McInnis AN (1982) Pancreatic ultrasound following blunt abdominal trauma. Gastrointestinal Radiol 7(1):53–56
Wellmann W, Gebel M (1981) After blunt abdominal trauma: peritoneal lavage or sonography?]. Deutsche Medizinische Wochenschrift 106(7):221–222 [German]
Jang T, Sineff S, Naunheim R, Aubin C (2004) Residents should not independently perform focused abdominal sonography for trauma after 10 training examinations. J Ultrasound Med 23(6):793–797
Strode CA, Rubal BJ, Gerhardt RT, Bulgrin JR, Boyd SY (2003) Wireless and satellite transmission of prehospital focused abdominal sonography for trauma. Prehospital Emerg Care 7(3):375–379
Jones PG, Peak S, McClelland A, Holden A, Higginson I, Gamble G (2003) Emergency ultrasound credentialling for focused assessment sonography in trauma and abdominal aortic aneurysm: A practical approach for Australasia. Emerg Med (Fremantle, WA). 15(1):54–62
Stassen NA, Lukan JK, Carrillo EH, Spain DA, Richardson JD (2002) Abdominal seat belt marks in the era of focused abdominal sonography for trauma. Arch Surg 137(6):718–722 (discussion 722–723)
Lukan JK, Franklin GA, Spain DA, Carrillo EH (2001) Incidental” pericardial effusion during surgeon-performed ultrasonography in patients with blunt torso trauma. J Trauma Injury Infect Crit Care 50(4):743–745
McCarter FD, Luchette FA, Molloy M, Hurst JM, Davis K Jr, Johannigman JA, Frame SB, Fischer JE (2000) Institutional and individual learning curves for focused abdominal ultrasound for trauma: cumulative sum analysis. Ann Surg 231(5):689–700
Salen PN, Melanson SW, Heller MB (2000) The focused abdominal sonography for trauma (FAST) examination: considerations and recommendations for training physicians in the use of a new clinical tool. [20 refs] Acad Emerg Med 7(2):162–168 [Review]
Hegenbarth R, Rehagel HJ (1995) Ultrasound findings in rupture of the colon after blunt abdominal trauma. Ultraschall Med 16(6):297–298 [German]
Conflict of interest statement
There is no conflict of interest related to the publication of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Additional information
CR abstract and ‘plain language summary’ in Appendix below.
Appendices
Appendix: 2005 FAST Cochrane review abstract
Background
Ultrasonography is regarded as the tool of choice for early diagnostic investigations in patients with suspected blunt abdominal trauma. Although its sensitivity is too low for definite exclusion of abdominal organ injury, proponents of ultrasound argue that ultrasound-based clinical pathways enhance the speed of primary trauma assessment, reduce the number of computed tomography scans and cut costs.
Objectives
To assess the efficiency and effectiveness of trauma algorithms that include ultrasound examinations in patients with suspected blunt abdominal trauma.
Selection criteria
Studies: randomised controlled trials (RCTs) and quasi-randomised trials (qRCTs). Participants: patients with blunt torso, abdominal or multiple trauma undergoing diagnostic investigations for abdominal organ injury. Interventions: diagnostic algorithms comprising emergency ultrasonography (US). Controls: diagnostic algorithms without US ultrasound examinations (for example, primary computed tomography [CT] or diagnostic peritoneal lavage [DPL]). Outcome measures: mortality, use of CT and DPL, cost-effectiveness, operative intervention and negative operative intervention rates, delayed diagnoses, and quality of life.
Data collection and analysis
Two authors independently selected trials for inclusion, assessed methodological quality and extracted data. Where possible, data were pooled and relative risks (RRs), risk differences (RDs) and weighted mean differences, each with 95% confidence intervals (CIs), were calculated by fixed- or random-effects modeling, as appropriate.
Main results
We identified four studies meeting our inclusion criteria. Overall, trials were of moderate methodological quality. Few trial authors responded to our written inquiries seeking to resolve controversial issues and to obtain individual patient data. We pooled mortality data from three trials involving 1,254 patients; relative risk in favor of the US arm was 1.00 (95% CI 0.50–2.00). US-based pathways significantly reduced the number of CT scans (random-effects RD −0.52, 95% CI −0.83 to −0.21), but the meaning of this result is unclear. Given the low sensitivity of ultrasound, the reduction in CT scans may either translate to a number needed to treat or number needed to harm of two.
Conclusions
There is currently insufficient evidence from RCTs to justify promotion of ultrasound-based clinical pathways in diagnosing patients with suspected blunt abdominal trauma.
Plain language summary
No evidence in favor of using ultrasound to aid diagnosis of patients with a ‘blunt’ injury of the abdomen.
Many people admitted to hospital after an injury have ‘blunt’ (that is, not penetrating) damage to the abdomen. Doctors treating these patients need to know whether the organs within the abdomen have been injured. Ultrasound scans are believed to help diagnose the condition of the patients. In this review, the authors looked for studies that compared death rates in patients with an abdominal injury where ultrasound was used to aid diagnosis with death rates where no ultrasound was used. They also looked for evidence that ultrasound use could reduce the need to carry out other more complex and more expensive diagnostic tests. However, very few trials have been done and the authors conclude there is insufficient evidence to justify the use of ultrasound as part of the diagnosis of patients with abdominal injury.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 2.0 International License ( https://creativecommons.org/licenses/by/2.0 ), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.
About this article
Cite this article
Melniker, L.A. The value of focused assessment with sonography in trauma examination for the need for operative intervention in blunt torso trauma: a rebuttal to “emergency ultrasound-based algorithms for diagnosing blunt abdominal trauma (review)”, from the Cochrane Collaboration. Crit Ultrasound J 1, 73–84 (2009). https://doi.org/10.1007/s13089-009-0014-7
Published:
Issue Date:
DOI: https://doi.org/10.1007/s13089-009-0014-7