Abstract
Patients on B cell immunosuppressive treatments have been shown to have persistent infection of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). In this report, a woman treated with ibrutinib for chronic lymphocytic leukemia experienced more than 40 days of coronavirus disease 2019 (COVID-19) infection. Unexpectedly, her peripheral blood experiments showed a normal SARS-CoV-2-specific antibody level and a relatively elevated percentage of CD19 + B cells, while an obvious decrease in the percentages of NK cells, CD4 + T cells and CD8 + T cells. Further SARS-CoV-2-specific T cell analysis in this patient indicated a significant decrease in the percentage of SARS-CoV-2-specific IFN-γ, TNF-α or IL-2 producing CD4 + T or CD8 + T cells. Most notably, ten days after the cease of ibrutinib, the PCR for SARS-CoV-2 turned negative and the reduced proportions of peripheral CD4 + T cells and CD8 + T cells recovered. Our research predicted that the depleted B-cell function therapies may play considerable role in the development of long COVID-19 and the abnormal T-cell subset distribution might be the underlying mechanism.
Similar content being viewed by others
Introduction
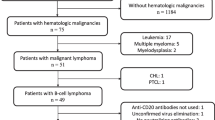
The duration of viral shedding of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is usually less than two weeks. Patients with hematological malignancies, especially chronic lymphocytic leukemia (CLL) are often on therapeutic drugs that suppress the immune system, putting them at a particularly high risk for persistent viral replication or severe secondary infections when infected with SARS-CoV-2 [1,2,3]. Ibrutinib is a potent Burton’s tyrosine kinase (BTK) inhibitor and has been used in different B cell malignancies, including CLL [4,5,6,7]. It has aroused heated clinical and scientific debate about whether the CLL patients infected with COVID-19 should maintain or discontinue ibrutinib treatment. In this scenario, the scholars who advocated ibrutinib discontinuation believed that the immunosuppressive activity of ibrutinib might bear responsibility for viral persistence and exacerbate secondary infection in susceptible patients [8,9,10]. The decision to continue ibrutinib was supported by data suggesting that BTK inhibition might mitigate the cytokine storm which was associated with a series of complications, including lung injury, DIC, and myocardial complications [8, 11, 12].
Here, we describe a patient who developed persistent symptomatic COVID-19 infection for more than forty days. The patient had a past history of CLL for which she had been receiving ibrutinib monotherapy for two years prior to the onset of symptoms of COVID-19. Initially admitted to another hospital and during twenty-day treatment period, the patient was instructed to continue taking ibrutinib to prevent tumor recurrence. However, Polymerase Chain Reaction (PCR) from nasopharyngeal specimens remained positive results for SARS-CoV-2. Contrary to previous studies that indicated decreased B cell levels and IgG levels during ibrutinib exposure [13, 14], this patient’s B cell counts and neutralizing antibody profiles for COVID-19 were comparable to those of convalescent patients. After creasing ibrutinib and receiving comprehensive treatment for approximately ten days, the SARS-CoV-2 PCR on the nasopharyngeal swab turned negative result. Specifically, we observed a notable recovery in the percentages of NK cells, CD4+ T cells, CD8+ T cells. Our findings suggest that impaired antiviral T cell responses to SARS-CoV-2 may underlie viral persistence, and we discussed the scientific rationale for discontinuing ibrutinib in CLL patients with persistent COVID-19 infection.
Methods
Data were collected from electronic health records. The diagnosis of COVID-19 was confirmed through PCR analysis of nasopharyngeal swabs using the SARS-CoV-2 assay from Roche and the Cobas 6800/8800 system. Plasma samples were analyzed for SARS-CoV-2 IgG using pseudovirus neutralization assays as described previously [15]. To detect SARS-CoV-2-specific CD4 + and CD8 + T cells, peripheral blood mononuclear cells (PBMCs) were isolated from blood, and 1 × 106 PBMCs were stimulated with SARS-CoV-2 S protein in 200 μl in 96-well U-bottom plates (Corning, PA, USA) in a 5% CO2 incubator at 37 °C for 20 h. To assess antigen-specific intracellular cytokine levels, including TFN-α, IFN-γ and IL-2, GolgiStop (BD Bioscience) was added 14 h after SARS-CoV-2 S protein stimulation, and the obtained cells were stained for phenotypic lymphocyte markers.
Results
A 68-year-old woman without SARS-CoV-2 vaccination developed symptoms including fever, progressive shortness of breath, and cough. On January 17, 2023 (day 8 of her illness), she sought medical attention at a local hospital. The patient had previously been diagnosed with CLL and had been receiving ibrutinib as a maintenance therapy for two years prior to the onset of her COVID-19 symptoms. A chest computed tomography (CT) was performed at the local hospital on January 19, 2023, revealed multiple ground glass nodules in bilateral lungs, which were characteristic findings of COVID-19. A nasopharyngeal specimen tested positive for SARS-CoV-2 via PCR assay, and her oxygen saturation levels of peripheral artery were below normal. During her hospitalization, she continued to receive ibrutinib for her CLL as well as a 7-day course of azvudine (5 mg/day). She was also administrated low doses of corticosteroids (specific details were not available), and medications to alleviate cough, phlegm and asthma. Despite these treatments, her body temperature continued to fluctuated, and her respiratory symptoms progressively worsened. Remarkably, a follow-up chest CT scan on February 5 showed significant progression with bilateral diffuse ground glass opacities. Additionally, a new nodular lesion was identified in the upper lobe of the right lung. Subsequently, the patient was discharged from the local hospital on February 10 (day 32 of her illness) and transferred to our hospital on February 17 for further treatment.
A nasopharyngeal swab performed on February 17 continued to yield positive results by RT-PCR, with detection of the ORF1ab gene (Ct 28.51) and the N gene (Ct 23.10). Blood tests showed moderate leukocytopenia and thrombocytopenia (3.0*10^9/L and 82.0*10^9/L, respectively), lymphopenia(0.6*10^9/L), elevated levels of CRP (93.30 mg/L), interleukin-6 (11.7 pg/ml), and ferritin (1733.00 ng/ml), as well as significant hypogammaglobulinemia for IgA, IgG, IgM and IgE (0.268 g/l, 4.67 g/l, 0.182 g/l and < 19.4 IU/ml, respectively). The peripheral blood flow cytometry revealed a reduction in NK cells (7.16%), CD4 + T cells (17.71%), and CD8 + T cells (12.65%), though the CD4 + /CD8 + cell ratio was within normal range (1.4). Unexpectedly, the percentage of CD19 + B cells did not decrease (54.32%). Notably, serological testing showed that the levels of neutralizing antibodies in this patient for multiple Omicron variants were detectable and very high (Table 1), aligning with prior evidence of no significant decline in CD19 + B cell percentages. As seen in Table 2, Table 3 and Table S1, after stimulated with the S protein of omicron or wild-type strain, we observed deficiency in naïve T cells and B cells, no significant differences in the proportion of T effector cells (Teff) or CD4 + , CD8 + effector memory T cells (Tem) and plasma cells between our patient and healthy controls who received two doses of the inactivated vaccine [15]. However, the percentage of SARS-CoV-2-specific IFN-γ-producing CD4 + T or CD8 + T cells was lower in our patient. All microbiologic tests for other respiratory pathogens showed negative results. The (1/3)-β-D-glucan test, GM test, latex agglutination test and the interferon-gamma release assay for tuberculosis were all negative. The levels of procalcitonin were normal and the blood culture was negative for fungus, bacteria, and anaerobes. At admission, treatment with dexamethasone was initiated, followed by a prolonged tapering corticosteroid regimen. Meanwhile, a second course of antiviral treatment (molnupiravir; 800 mg, twice a day, for 5 days) and intravenous piperacillin-tazobactam were administered. She also received supportive and symptomatic treatments including intravenous immunoglobulin, low-molecular-weight heparin, leucogen and ambroxol hydrochloride tablets (Table 4). After an interdisciplinary discussion with hematologist, the patient was asked to cease ibrutinib on the second day of her admission. The enhanced chest CT examination on February 20 showed bilateral diffuse ground glass opacities and the lesions in the dorsal segment of the left lower lobe trended towards consolidation. A lump was identified in the upper lobe of the right lung, with a diameter of about 3.2 cm and obvious enhancement at the edge. Burr-like changes and pleural traction were seen at lower edge of the lump (Fig. 1). For this reason, we consulted an interventional radiologist for their opinion about whether it was necessary to perform a puncture examination on the lump and were advised to strengthen the anti-infection therapy first. Therefore, Piperacillin-Tazobactam was replaced with imipenem on the fifth day of hospitalization. The SARS-CoV-2 RNA became undetectable on February 24 (the 8th day of her admission, 43 days after her initial symptoms), and remained negative on February 28. The follow-up peripheral blood flow cytometry on February 28 revealed a recovered NK cells (14.19%), CD4 + T cells (29.74%), CD8 + T cells (45.09%), and an inversion of the ratio of CD4 + /CD8 + cells (0.81). Significantly, the percentage of CD19 + B cells returned to 9.71%. The neutralizing antibody levels for SARS-CoV-2 detected in the repeated serologic test on February 28 are comparable to those on February 18 (Table 1). After about 10 days of treatment including the anti-infection therapy (Imipenem and Cilastatin Sodium, 1 g, iv, every 8 h a day), intravenous immunoglobulin (5 g, ivgtt, once a day), glucocorticoid (Dexamethasone, 3 mg, iv, once a day, for three days, then switch to prednisone acetate; 15 mg, po, once a day, tapering by 1 tablet every 3 days), low-molecular-weight heparin (4000 IU, ih, once a day) and ambroxol hydrochloride tablets (30 mg, po, three times a day), multiple indicators significantly improved in blood tests (Table 4). A follow-up CT scan on March 1 showed a resolution of bilateral inflammation. Moreover, the solid lesions in the upper lobe of the right lung transformed into air space opacities with gas-fluid levels (Fig. 1). Her general condition continued to improve, and she was finally discharged to home on March 2 (day 49) of her illness. Since then, the patient has been well without recurrence of symptoms and the PCR for SARS-CoV-2 remains to be negative. One month later, she became able to resume maintenance treatment with ibrutinib for CLL. Nowadays, the patient has been able to restart her active lifestyle.
Radiological characteristics on chest CT. A Enhanced chest CT images taken on February 20 revealed diffuse ground glass opacities in both lungs and partial consolidation in the dorsal segment of the left lower lobe. A nodular lesion of about 3.2 cm was found in the upper lobe of the right lung(red arrow). Left: images of the lung window; Right: images of the mediastinal window. B Follow-up enhanced chest CT was performed on March 1, indicating that the opacities were gradually resolving, and the solid lesions in the upper lobe of the right lung had shrunk to 2.8 cm and turned into air space opacities with fluid accumulation (red arrow). Left: images of the lung window; Right: images of the mediastinal window
Discussion
The viral shedding of SARS-CoV-2 from upper respiratory specimens declines after initiation of symptoms and turned negative around 10 days after infection [2]. However, immunocompromised population, especially patients with hematologic malignancies have been reportedly shed the active virus for longer periods [16, 17]. We described a case of a hematologic patient on ibrutinib monotherapy who experienced persistent COVID-19 infection. We ruled out reinfection or viral evolution, as all nasopharyngeal samples showed Ct values below 30 when SARS-CoV-2 RNA was positive, and neutralizing antibody levels mirrored changes in viral RNA clearance. Our investigation then focused on the patient's humoral and cellular immunity, revealing that despite a deficiency in naïve B cells, the patient exhibited levels of plasma cells and neutralizing antibodies comparable to those in recovered patients with similar disease courses. We also noted a temporary decrease in peripheral CD4 + and CD8 + T cells, which returned to normal after cessation of ibrutinib. Additionally, our patient showed reduced production of IL-2, IFN-γ and TNF-α in SARS-CoV-2-specific CD4 + and CD8 + T cells, indicating impaired T response.
The immunologic factors associated with chronic SARS-CoV-2 infection, such as CD4 + lymphopenia and B-cell aplasia, are distinct from those observed in acute severe COVID-19 infection. Hao et al. studied 104 COVID-19 patients and reported that decreased T cells and B cells were linked to prolonged viral shedding of SARS-CoV-2 [18]. Initially, we assessed our patient's neutralizing antibody profiles to explore whether ibrutinib, which can potentially impair humoral immunity, might influence the magnitude and duration of viral RNA shedding. The results showed that despite the patient's deficiency in naïve B cells, their levels of neutralizing antibodies against COVID-19 and plasma cell counts were normal. There is limited data on how BTKi affect neutralizing antibody levels in hematologic disorder patients post COVID-19 infection, but studies have shown increased Spike-IgG levels in serum after five COVID-19 vaccine doses in some ibrutinib-treated patients [19]. This variability may arise from patient heterogeneity or immune reconstitution, as Sun noted partial restoration of normal B cells and humoral immunity in CLL patients treated with ibrutinib [13]. Another possible reason for our patient’s high Spike-IgG levels could be that sampling for neutralizing antibody detection was performed one month after the initial onset of symptoms, a period was sufficient for activating humoral immunity and generating neutralizing antibodies. Furthermore, Ibrutinib significantly impacted the production of naïve B cells in this patient, while memory B cells and plasma cells were less affected.
Given the abnormal T-cell subset distribution and function reported in CLL [18], an alternative explanation for prolonged viral shedding in our patient could be an impaired antiviral T-cell response to SARS-CoV-2. We observed a decreased proportion of peripheral CD4 + and CD8 + T cells and a poor T-cell response to SARS-CoV-2 in our patient. These findings align with other studies that have indicated impaired T-cell responses in some patients with severe symptoms or poor viral control early in the disease course [20, 21]. The compromised T-cell response in our patient's peripheral blood may be attributed to the tumor clone, which can disrupt T-cell subgroup balance and impair T-cell-mediated immune responses, or to ibrutinib reducing granzyme and IFNγ in CD8 + T cells [19]. This latter possibility is supported by the observed recovery of CD4 + and CD8 + T cells following cessation of ibrutinib. Further studies are necessary to confirm or differentiate between these potential causes of persistent viral shedding in more COVID-19 cases.
Many studies have reported persistent COVID-19 infection in patients with undergoing B-cell depletion therapy for hematologic malignancies, which can result in humoral defects [22,23,24]. However, our findings point to immune dysregulation characterized by impaired T cell responses as a causal factor in the development of long COVID-19 and developed infection lesions in the lungs. This also raises the controversy of whether ibrutinib therapy has an impact on the disease course and outcome in SARS-CoV-2 infected patients. We suggest that for such patients, it may be advisable to consider continuing BTKi therapy to manage underlying conditions only after controlling viral, bacterial, fungal, or other pathogenic infections. However, there are some contrary reports suggesting that BTKi can suppress excessive inflammatory responses and reduce the risk of severe infections of COVID-19 [8]. Hence, personalized treatment is essential for different patients. Future studies should aim to elucidate the immunologic defects associated with this clinical phenomenon, beyond the risk identified in our report related to BTKi treatment. Meanwhile, resuming antiviral treatment in immunocompromised patients with prolonged COVID-19 viral shedding should also be considered as a favorable factor for patient’s recovery. Taken together, our results seem to support the prognostic values of monitoring SARS-CoV-2-reactive antibodies and analyzing SARS-CoV-2-specific T cells in patients receiving ibrutinib for CLL therapy.
Availability of data and materials
All data generated or analyzed during this study are included in this published article and its supplementary information files.
Data availability
Data is provided within the manuscript or supplementary information files.
References
Young BE, Ong SWX, Kalimuddin S, Low JG, Tan SY, Loh J, et al. Epidemiologic Features and Clinical Course of Patients Infected With SARS-CoV-2 in Singapore. JAMA. 2020;323(15):1488–94.
Aydillo T, Gonzalez-Reiche AS, Aslam S, van de Guchte A, Khan Z, Obla A, et al. Shedding of Viable SARS-CoV-2 after Immunosuppressive Therapy for Cancer. N Engl J Med. 2020;383(26):2586–8.
Liang W, Guan W, Chen R, Wang W, Li J, Xu K, et al. Cancer patients in SARS-CoV-2 infection: a nationwide analysis in China. Lancet Oncol. 2020;21(3):335–7.
Koffman B, Mato A, Byrd JC, Danilov A, Hedrick B, Ujjani C, et al. Management of CLL patients early in the COVID-19 pandemic: An international survey of CLL experts. Am J Hematol. 2020;95(8):E199–203.
Davids MS, Brown JR. Ibrutinib: a first in class covalent inhibitor of Bruton’s tyrosine kinase. Future Oncol. 2014;10(6):957–67.
Treon SP, Tripsas CK, Meid K, Warren D, Varma G, Green R, et al. Ibrutinib in previously treated Waldenström’s macroglobulinemia. N Engl J Med. 2015;372(15):1430–40.
Kim ES, Dhillon S. Ibrutinib: a review of its use in patients with mantle cell lymphoma or chronic lymphocytic leukaemia. Drugs. 2015;75(7):769–76.
Chong EA, Roeker LE, Shadman M, Davids MS, Schuster SJ, Mato AR. BTK Inhibitors in Cancer Patients with COVID-19: “The Winner Will be the One Who Controls That Chaos” (Napoleon Bonaparte). Clin Cancer Res. 2020;26(14):3514–6.
Mato AR, Roeker LE, Lamanna N, Allan JN, Leslie L, Pagel JM, et al. Outcomes of COVID-19 in patients with CLL: a multicenter international experience. Blood. 2020;136(10):1134–43.
Scarfò L, Chatzikonstantinou T, Rigolin GM, Quaresmini G, Motta M, Vitale C, et al. COVID-19 severity and mortality in patients with chronic lymphocytic leukemia: a joint study by ERIC, the European Research Initiative on CLL, and CLL Campus. Leukemia. 2020;34(9):2354–63.
Lin AY, Cuttica MJ, Ison MG, Gordon LI. Ibrutinib for chronic lymphocytic leukemia in the setting of respiratory failure from severe COVID-19 infection: Case report and literature review. EJHaem. 2020;1(2):596–600.
Fiorcari S, Atene CG, Maffei R, Debbia G, Potenza L, Luppi M, et al. Ibrutinib interferes with innate immunity in chronic lymphocytic leukemia patients during COVID-19 infection. Haematologica. 2021;106(8):2265–8.
Sun C, Tian X, Lee YS, Gunti S, Lipsky A, Herman SEM, et al. Partial reconstitution of humoral immunity and fewer infections in patients with chronic lymphocytic leukemia treated with ibrutinib. Blood. 2015;126(19):2213–9.
Byrd JC, Furman RR, Coutre SE, Flinn IW, Burger JA, Blum KA, et al. Targeting BTK with ibrutinib in relapsed chronic lymphocytic leukemia. N Engl J Med. 2013;369(1):32–42.
Wei D, Chen Y, Yu X, Lai YD, Xu W, Ji P, et al. Comparable antigen-specific T cell responses in vaccinees with diverse humoral immune responses after the primary and booster BBIBP-CorV vaccination. Emerging microbes & infections. 2022;11(1):2474–84.
Levi G, Rocchetti C, Magri R, Uccelli S, Bottone D, Quadri F, et al. Hyperimmune plasma infusion in an immunocompromised Covid-19 patient previously treated for follicular lymphoma. Monaldi Arch Chest Dis. 2021;91(4).
Nakamura S, Kanemasa Y, Atsuta Y, Fujiwara S, Tanaka M, Fukushima K, et al. Characteristics and outcomes of coronavirus disease 2019 (COVID-19) patients with cancer: a single-center retrospective observational study in Tokyo. Japan Int J Clin Oncol. 2021;26(3):485–93.
Hao S, Lian J, Lu Y, Jia H, Hu J, Yu G, et al. Decreased B Cells on Admission Associated With Prolonged Viral RNA Shedding From the Respiratory Tract in Coronavirus Disease 2019: A Case-Control Study. J Infect Dis. 2020;222(3):367–71.
Bacova B, Kohutova Z, Zubata I, Gaherova L, Kucera P, Heizer T, et al. Cellular and humoral immune response to SARS-CoV-2 mRNA vaccines in patients treated with either Ibrutinib or Rituximab. Clin Exp Med. 2023;23(2):371–9.
Bergamaschi L, Mescia F, Turner L, Hanson AL, Kotagiri P, Dunmore BJ, et al. Longitudinal analysis reveals that delayed bystander CD8+ T cell activation and early immune pathology distinguish severe COVID-19 from mild disease. Immunity. 2021;54(6):1257–1275.e1258.
Notarbartolo S, Ranzani V, Bandera A, Gruarin P, Bevilacqua V, Putignano AR, et al. Integrated longitudinal immunophenotypic, transcriptional and repertoire analyses delineate immune responses in COVID-19 patients. Sci Immunol. 2021;6(62):eabg5021.
Baang JH, Smith C, Mirabelli C, Valesano AL, Manthei DM, Bachman MA, et al. Prolonged Severe Acute Respiratory Syndrome Coronavirus 2 Replication in an Immunocompromised Patient. J Infect Dis. 2021;223(1):23–7.
Lee CY, Shah MK, Hoyos D, Solovyov A, Douglas M, Taur Y, et al. Prolonged SARS-CoV-2 Infection in Patients with Lymphoid Malignancies. Cancer Discov. 2022;12(1):62–73.
Martínez-Chinchilla C, Vazquez-Montero L, Palazón-Carrión N, Fernández-Román IM, López-Barba J, de la Cruz-Merino L, et al. Persistence of SARS-CoV-2 Infection in Severely Immunocompromised Patients With Complete Remission B-Cell Lymphoma and Anti-CD20 Monoclonal Antibody Therapy: A Case Report of Two Cases. Front Immunol. 2022;13: 860891.
Acknowledgements
We thank the patient for a retrospective re-interview and for providing epidemiologically related information relevant to this study.
Funding
This work was supported by the Shanghai Science and Technology Innovation Action Plan, experimental animal research project (No. 23141901900); Basic Research Project of the Sixth People's Hospital of Shanghai (No.ynms202306).
Author information
Authors and Affiliations
Contributions
S.M., D. W. and W. H. performed and analyzed experiments. M.X. and Y. Z. provided patient care, clinical information, and samples from the patient. X. C. and J. C. supervised the research. J. C., S. M. and D. W. wrote the manuscript, and all the co-authors revised, edited, and approved the manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Ethics approval is not necessary for this case report. Informed consent was obtained from this patient for being included in the study.
Consent for publication
Written informed consent was obtained from the patient for the publication of this case report.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Ma, S., Wei, D., Hu, W. et al. A case report of prolonged viral shedding of SARS-CoV-2 in a patient who receive ibrutinib for CLL therapy. BMC Infect Dis 24, 895 (2024). https://doi.org/10.1186/s12879-024-09794-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-024-09794-z