Abstract
Background
Systemic lupus erythematosus (SLE) has been less deadly since the advent of corticosteroid-sparing medications. SLE patients still have a higher mortality rate than the general population. Infectious disease is reported as one of the major causes of death in patients with SLE. Although bacteria are the most often isolated pathogens from patients with SLE, Pneumocystis jirovecii pneumonia (PJP) is more deadly than bacterial infection.
Methods
We retrospectively enrolled consecutive patients with SLE concurrent with PJP (SLE-PJP) in our center between January 2014 and December 2022. The participants were classified into two groups: survivors and non-survivors. Cox regression models and Kaplan‒Meier survival analyses were conducted to explore prognostic factors for survival.
Results
There were 57 patients with SLE (42.0 ± 15.8 years old, 78.9% female) complicated with PJP, 22 (38.6%) of whom died. Compared with the survival group, the non-survival group had more patients with hyperglycemia or diabetes mellitus, invasive ventilation (p < 0.01), respiratory failure, intensive care unit admission, non-invasive ventilation, and hospital-acquired pneumonia (p < 0.05). The non-survival group showed a higher neutrophil percentage, lactate dehydrogenase, D-dimer (p < 0.001), urea, high-sensitivity C-reactive protein (hsCRP), erythrocyte sedimentation rate (ESR), and ferritin (p < 0.05). It also had lower minimal albumin, hemoglobin (p < 0.001), immunoglobulin G, complement 3, peripheral lymphocyte count, platelet, NK cell count, and CD4+ T-cell count (p < 0.05). Multivariate analysis indicated that hyperglycemia or diabetes mellitus (HR = 4.25, p < 0.01, 95% CI: 1.51–11.97), thrombocytopenia (HR = 4.22, p < 0.01, 95% CI: 1.63–10.91) and lower complement 3 (C3) (HR = 4.06, p < 0.01, 95% CI: 1.60-10.33) were independent risk factors for the survival of SLE-PJP patients.
Conclusions
The mortality rate of patients with SLE-PJP is still high. Hyperglycemia, decreased C3, and thrombocytopenia are independent survival risk factors.
Similar content being viewed by others
Introduction
Systemic lupus erythematosus (SLE) is a common chronic multisystemic autoimmune disease with heterogeneous clinical phenotypes that predominantly affects young females. Although the overall mortality rate of patients with SLE has improved dramatically since the 21st century thanks to improvements in early diagnosis and treatment, SLE patients still have a higher mortality than the general population [1]. The standardized mortality rate (SMR) of SLE has been 1.8-3.0 in epidemiologic studies [2,3,4,5]. Infectious diseases are some of the main causes of death [3, 6]. A case‒control study showed that uncontrolled SLE (20%), infection (34.2%), and both together (24.8%) were common causes of death in hospitalized patients with SLE [6]. A Chinese nationwide cohort study of 29,510 hospitalized patients with SLE reported that infection (65.8%) was the most common cause of death, followed by lupus nephritis (48.6%) and hematological abnormalities (18.1%) [3]. The lower respiratory system is one of the most involved infection sites in SLE patients [7, 8]. Opportunistic pathogens such as pneumocystis, Mycobacterium tuberculosis and cytomegalovirus are common and are also associated with a high risk of in-hospital death among SLE patients [9].
Pneumocystis jirovecii pneumonia (PJP) is a fatal opportunistic infectious disease that predominantly occurs in immunosuppressed patients. PJP was first reported as the most common opportunistic infection in patients with human immunodeficiency virus (HIV), but with suggested preventive protocols and effective antiretroviral treatments, PJP incidence and mortality have fallen dramatically in HIV patients. However, immunosuppression treatments, including chemotherapy, radiotherapy, transplantation, corticosteroids and/or immunosuppressant medications, have been gradually reported as common risk factors for PJP. Non-HIV-PJP patients have different manifestations and prognoses than HIV-PJP patients, with rapid progression to hypoxemia and high mortality [10,11,12]. Both inherently associated SLE immunodeficiency and immunosuppressant treatment might be key risk factors for common opportunistic infections, e.g., PJP, in SLE patients. Patients with SLE-PJP have a mortality rate as high as 37–60% [13]. We conducted this retrospective analysis of hospitalized SLE-PJP patients to elucidate their clinical characteristics and prognostic factors, aiming to improve the identification of high-risk SLE-PJP patients with poor prognosis and improve their clinical management.
Materials and methods
Patients
All enrolled patients who were discharged with a diagnosis of PJP and negative HIV test from January 2014 to December 2022 were screened for eligibility from the electronic medical records system at Peking Union Medical College Hospital (PUMCH). There were 246 hospitalized patients with systemic autoimmune diseases who were complicated with PJP. Among them, there were 57 patients with SLE. Their complete medical records and radiological imaging data were retrospectively reviewed through the hospital’s electronic banks. They were followed up from the day that the diagnosis PJP was confirmed. After discharge, they were followed up every 1 to 6 months, depending on the disease activity and severity. The final follow-up point was December 30, 2023. The follow-up information was obtained through outpatient records or telephone conversations. The following information was reviewed and analyzed: age, sex, the clinical manifestations, the serological results, chest high-resolution computed tomography (HRCT), treatments, and outcomes. Survival time was defined as the time from diagnosis of PJP to death or the final follow-up point.
During screening process, patient with any of following character were excluded from our study: (1) younger than 18 years old; (2) with positive HIV test; and (3) without chest CT imaging in our hospital’s data bank.
Definitions
Diagnosis of SLE were coincide with 2012 SLE classification criteria of the Systemic Lupus International Collaborating Clinics (SLICC) [14] and/or 2019 SLE classification criteria of European League Against Rheumatism /American College of Rheumatology (EULAR/ACR) [15].
Diagnostic criteria of confirmed PJP were defined as follows: (1) new presence of relevant respiratory manifestations (cough, dyspnea, sputum, and/or hypoxia) or fever (temperature ≥ 37.3 ℃); (2) new presence of pulmonary shadows (ground-glass opacities, consolidation, or patchy shadows) that were identified by chest CT; (3) Pneumocystis DNA fragments were confirmed by polymerase chain reaction (PCR) or metagenomic next-generation sequencing (mNGS), and/or Pneumocystis asci were observed at direct microscopic examination with Grocott’s methenamine silver (GMS) stain in the respiratory samples, including qualified sputum specimens, aspirates, or bronchoalveolar lavage fluid (BALF).
Respiratory failure was defined as a room air pulse oxygenation of < 90%, a room air arterial partial pressure oxygen level of < 60 mmHg (1 mmHg = 0.133 kPa), or the oxygenation index under oxygen inhalation is less than 300 mmHg.
Cytomegalovirus (CMV) viremia was defined as peripheral blood CMV-DNA > 500 copies.
This study was approved by the Ethics Committee of Peking Union Medical College Hospital (K5596) in accordance with the Declaration of Helsinki. Our study was performed using anonymized health care data. The written informed consent from each patient was waived as this study met the PUMCH IRB’s minimal risk waiver criteria.
Statistical analysis
All the data were analyzed using the IBM SPSS Statistics version 27.0 software package (IBM Corporation, North Castle Drive, MD-NC119, Armonk, NY 10504 − 1785, USA). The quantitative variables were presented as the means ± standard deviations (SD) or medians (interquartile ranges [IQRs]), and the categorical variables were presented as frequencies and percentages. Comparison between groups was conducted using t test or rank sum test for quantitative variables, and the chi-square test for categorical variables. Cox regression models were used to identify factors associated with prognosis for SLE-PJP patients. The statistically significant variables selected via univariate analysis were finally assessed by multivariate analysis. And Kaplan–Meier survival curves were used to compare mortality of different groups. The difference was statistically significant when p < 0.05.
Results
General characteristics of the enrolled SLE patients with PJP (SLE-PJP)
Fifty-seven patients with a diagnosis of SLE-PJP were enrolled in our study after a detailed medical record review. Among them were 35 survival patients (61.4%) and 22 non-survival patients (38.6%), with a median follow-up period of 198 days. 12 were male (21.1%) and 45 were female (78.9%), and they were 42.0 ± 15.8 years old (range 20 to 77 years). The average period of PJP infection was 7.7 years after the diagnosis of SLE. Among 22 patients in non-survival group, 8 (36.4%) died due to severe PJP infection, 10 (45.5%) died due to pulmonary mixed infection (CMV, bacteria, aspergillus, etc.) including PJP infection, 3 (13.6%) died due to septic shock, and 1 (4.5%) died due to the progression of the underlying ILD after PJP infection.
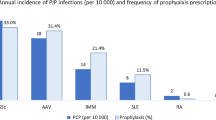
The SLE-PJP patients had several comorbidities (Fig. 1): 19 patients (33.3%) had ILD, about half of the patients (29, 50.9%) had hyperglycemia or diabetes, and most patients (41, 71.9%) had kidney disease. Among them, 36 SLE-PJP patients (63.2%) experienced respiratory failure, and 33 patients (57.9%) were transferred to intensive care unit (ICU) wards. Most patients were given glucocorticosteroids (56, 98.2%) and/or immunosuppressants/biological medications (44, 77.2%) before PJP. There were 29.5% (13/44) patients treated with mycophenolate mofetil, 25% (11/44) patients treated with cyclophosphamide, 20.5% (9/44) patients treated with other immunosuppressants (such as methotrexate, azathioprine, cyclosporine A, tacrolimus, etc.), and 25% (11/44) patients treated with the combination of the above two immunosuppressants. Some patients had coinfection with CMV viremia (38, 66.7%), hospital-acquired pneumonia (HAP) (19, 33.3%), oral candidiasis (7, 12.3%), aspergilli (10,17.5%), mycobacteria (1, 1.8%), and nocardia (1, 1.8%).
The main clinical manifestations of PJP were dyspnea (54, 94.7%), fever (52, 91.2%), cough (49, 86.0%), expectoration (40, 70.2%), and, rarely, hemoptysis (2, 3.5%). Hypoalbuminemia was common in the SLE-PCP patients; 55 patients (96.5%) had hypoalbuminemia, with minimal serum albumin (23.0 ± 5.5) g/L. Many SLS-PJP patients (48, 84.2%) had a low peripheral lymphocyte count, i.e., 0.8 ± 1.4 × 109/L. Most patients (54, 94.7%) had a low peripheral CD4+ T-cell count (129.7 ± 196.4)/µL. Bilateral (56, 98.2%), ground-glass opacities (GGOs) (48, 84.2%), and patches (46, 80.7%) were the most common chest CT manifestations. Less common chest CT findings were consolidations (22, 38.6%), lymphadenopathy (22, 38.6%), pleural effusion (27, 47.4%), and pleural thickening (34, 59.6%).
After the diagnosis of PJP, all patients (57, 100%) were prescribed trimethoprim-sulfamethoxazole (TMPco), and about half of them (27, 47.4%) also received second-line treatment with second-line anti-PJ medications: caspofungin (21, 36.8%), clindamycin (13, 22.8%), or primaquine (1, 1.8%).
Differences between the survival and non-survival groups of SLE-PJP patients
The baseline characteristics of patients with SLE-PJP, subdivided according to prognosis, i.e., the survival group vs. the non-survival group, are listed in Table 1. There were no significant differences in age, sex, interval from diagnosis of SLE to diagnosis of PJP, or interval between onset and diagnosis of PJP between the two groups. Hyperglycemia or diabetes was more common in the non-survival group (72.7% vs. 37.1%, p < 0.01).
The clinical characteristics of patients with PJP in different prognostic groups are listed in Table 2. Patients in the non-survival group were more likely to suffer from respiratory failure (72.7% vs. 37.1%, p < 0.01), to be transferred to the ICU (77.3% vs. 45.7%, p = 0.02), to need invasive ventilation (77.3% vs. 34.3%, p < 0.01), and to need noninvasive ventilation (50.0% vs. 20.0%, p = 0.02). Both groups had some patients who suffered from mixed infectious diseases. There were significantly more patients with hospital-acquired pneumonia in the non-surviving group than in the surviving group (50.0% vs. 22.9%, p = 0.03). The two groups had similar chest CT features and received glucocorticosteroid or immunosuppressant administration. As for anti-PJP treatment, patients in the non-survival group were more likely to be prescribed combination with second-line antibiotics (63.6% vs. 37.1%, p = 0.05). In the non-survival group, all 14 patients were prescribed with second-line treatment because of poor therapeutic effect and progression of disease, and 4 patients among them reduced TMPco dose due to renal impairment.
The differences in laboratory data between the two groups of SLE-PJP patients were as follows. The non-survival group had a significantly higher neutrophil percentage (89.6 ± 8.0% vs. 82.9 ± 13.0%, p < 0.001), urea [10.5 (8.4, 24.8) mmol/L vs. 7.6 (4.8, 14.6) mmol/L, p = 0.02], lactate dehydrogenase [798.0 (683.5, 1200.5) U/L vs. 500.0 (327.8, 689.8) U/L, p < 0.001], high-sensitivity C-reactive protein (78.7 ± 72.8 mg/L vs. 36.5 ± 42.7 mg/L, p = 0.02), erythrocyte sedimentation rate (65.8 ± 31.4 mm/h vs. 46.5 ± 31.1 mm/h, p = 0.03), ferritin [1071.0 (516.0, 2455.0) µg/L vs. 459.0 (185.8, 1177.8) µg/L, p < 0.05], and D-dimer [6.7 (1.4, 13.5) mg/L vs. 0.9 (0.4, 1.8) mg/L, p < 0.001]. The non-survival group had significantly lower levels of PaO2/FiO2 ratio [116.5 (86.5, 211.8) vs. 250.0 (157.0, 375.0), p < 0.001], minimal albumin (19.3 ± 4.1 g/L vs. 25.4 ± 4.9 g/L, p < 0.001), immunoglobulin G (5.6 ± 3.0 g/L vs. 8.7 ± 4.3 g/L, p < 0.01), complement 3 (C3) (0.7 ± 0.3 g/L vs. 0.9 ± 0.3 g/L, p = 0.02), peripheral lymphocyte count (0.4 ± 0.3 × 109/L vs. 1.0 ± 1.7 × 109/L, p = 0.03), hemoglobin (86.6 ± 20.2 g/L vs. 107.1 ± 19.7 g/L, p < 0.001), and platelets (102.1 ± 85.9 × 109/L vs. 169.5 ± 92.5 × 109/L, p < 0.01). NK cell count (21.6 ± 33.5 /µL vs. 56.8 ± 75.4 /µL, p = 0.04), and CD4+ T cell count (63.7 ± 43.3 /µL vs. 167.4 ± 237.3 /µL, p = 0.03).
Prognostic analysis for SLE-PJP patients
Univariate Cox regression analysis (Fig. 2A) indicated that hyperglycemia or diabetes mellitus, HAP, respiratory failure, non-invasive ventilation, invasive ventilation, ICU admission, thrombocytopenia, higher serum urea, lower immunoglobulin G and lower C3 were associated with non-survival. Finally, multivariate Cox regression analysis showed that hyperglycemia or diabetes mellitus (HR = 4.25, χ2 = 7.49, p < 0.01, 95% CI: 1.51–11.97), thrombocytopenia (HR = 4.22, χ2 = 8.84, p < 0.01, 95% CI: 1.63–10.91) and lower C3 (HR = 4.06, χ2 = 8.68, p < 0.01, 95% CI: 1.60-10.33) were independent risk factors for non-survival in patients with SLE-PJP.
Kaplan-Meier analysis (Fig. 3) also indicated that decreased C3 (p < 0.001) were associated with poor survival in SLE-PJP patients. The median survival time of non-survival group was thirty-three days.
Discussion
Our retrospective study showed that the mortality rate of SLE-PJP patients was high (38.6%, 22 of 57), and hyperglycemia, diabetes mellitus, decreased C3, and thrombocytopenia were independent risk factors for their survival. Neither corticosteroid and/or immunosuppressant administration before concurrent PJP nor peripheral CD4+ T-cell count was associated with their survival.
Previous studies have reported that risk factors for SLE-PJP include long-term use of glucocorticoids and immunosuppressants, a low CD4+ T-cell count, and renal dysfunction [16, 17]. There has not been much research on the prognostic factors of SLE-PJP. Advanced age, pneumomediastinum, low PaO2/FiO2, high D (A-a) O2, increased urea, decreased albumin, bacteremia, preexisting pulmonary underlying diseases and initial anti-PJP treatment failure were reported to be independent factors for poor prognosis in non-HIV PJP patients [18,19,20]. In our study, hyperglycemia or diabetes mellitus was one of the independent survival risk factors among SLE-PJP patients. A meta-analysis showed that diabetes mellitus (OR = 3.89, P < 0.001, 95% CI: 2.45–6.16) was associated with infection in SLE patients [21]. A retrospective nationwide study in Korea showed that diagnoses of diabetes (HR = 2.51, 95% CI: 1.19–5.31) significantly associated with PJP risk in ulcerative colitis patients [22]. Hyperglycemia can lead to the suppression of neutrophils and mononuclear phagocyte systems [23]. Diabetes mellitus can also cause lymphocyte dysfunction, reduce the activity of NK cells, change T-cell differentiation, and damage the function of B cells [24]. Therefore, patients with hyperglycemia might suffer from an inability to overcome infections. In future diagnosis and treatment, we should pay attention to SLE patients with hyperglycemia and strictly control their blood glucose during follow-up.
Our study also revealed that thrombocytopaenia increased the risk of death in SLE-PJP patients in the non-survival group (102.1 ± 85.9 × 109/L) versus survival group (169.5 ± 92.5 × 109/L). A retrospective study on the short-term prognosis of patients with SLE with infection showed deceased patients had a lower platelet count than survivors (93.0 ± 64.0 × 109/L vs. 181.3 ± 82.1 × 109/L, P < 0.001) [25]. A meta-analysis found that compared to non-infected SLE patients, infected patients had significantly fewer platelets (OR = 1.61, P < 0.001, 95% CI: 1.40–1.85) [21].
The complement system not only participates in the pathogenesis of SLE but is also an important component of innate immunity and plays an important role in regulating adaptive immunity. In SLE patients with increased complement C3 consumption and decreased production, the risk of infection might significantly increase. According to our findings, lower complement C3 was an independent risk factor for mortality in SLE-PJP patients. The C3 concentration in the non-survival group of patients was 0.7 ± 0.3 g/L, while that in the survival group was 0.9 ± 0.3 g/L. Barrera et al. investigated risk factors for drug-resistant bacterial infections in patients with SLE and reported that low pre-infection C3 levels (OR = 3.12, 95% CI: 1.91–8.22) were an independent risk factor [26]. One study investigated whether monitoring complement levels could predict the occurrence of infection in kidney transplant recipients and showed that decreased C3 at 1 month after transplantation was a risk factor for overall (AHR = 1.91, p < 0.01) and bacterial infection (AHR = 2.13, p < 0.05), while decreased C3 at 6 months predicted the occurrence of bacterial infection (AHR = 3.35, p = 0.04) in the late period (> 6 months) [27]. Although complement 4 (C4) plays a crucial role in the classical activation pathway of the complement system, like our study, that study did not show that the serum level of C4 was associated with infectious disease [27]. Another study reported that 24-hour urinary protein, peripheral lymphocyte count, and low serum C3 (OR= 0.10, 95% CI: 0.01‐0.95, p < 0.05) were independent prognostic predictors of short-term mortality in SLE patients with concurrent pulmonary infection [28]. Therefore, C3 is an important component of the complement system that is involved in microbial clearance. The opsonophagocytic capacity of neutrophils is positively correlated with the level of serum complement factors, and C3a, which is liberated by C3 during complement activation, also has direct antimicrobial activity [29]. Defending against extracellular bacteria has been considered the main role of C3 [30], and it is also important in controlling intracellular microorganism infection [31]. Moreover, it has recently been found that viruses or intracellular bacteria can decrease defense by binding complement regulatory proteins and receptors, which increases their pathogenicity [32]. Animal experiments have shown the relevance of C3 in the activation and regulation of the immune system. In Yuan’s septic model of peritonitis, exogenous C3 administration to mice at an early stage was associated with attenuated liver and kidney injuries, better bacterial clearance, and longer survival [33].
Previous reports on the adverse effects of corticosteroid and/or immunosuppressant therapy on SLE-PJP patients are inconsistent. A retrospective study showed that higher doses of glucocorticoids increased the risk of PJP in SLE patients (5–10 mg/day, OR = 25.88, 95% CI: 2.97-225.33; > 10 mg/day, OR = 286.58, 95% CI: 28.58-> 999), as did a higher 3-month cumulative dose of cyclophosphamide (> 1.4 g, OR = 11.52, 95% CI: 1.97–67.39) [34]. Another study found that cyclophosphamide did not increase the risk of PJP infection in SLE patients [17]. A retrospective study of 95 SLE patients who were hospitalized for pulmonary infections showed that the average daily steroid dose before PJP infection and high-dose steroid pulse therapy did not increase patient mortality, and immunosuppressant therapy was not associated with patient mortality [35]. Our study also showed that corticosteroid or immunosuppressant administration was not associated with mortality in SLE-PJP patients. Some immunosuppressants even have anti-PJP effects. Hydroxychloroquine (HCQ) has been reported to have antibacterial activity, possibly through pH-dependent iron depletion and an increased pH of the phagosome, which in turn inhibits the growth of intracellular organisms and the hyperinflammatory state of peripheral blood mononuclear cells (PBMCs) [36]. In SLE patients, HCQ users have had a lower risk of infection than never-users [37]. Yeo KJ et al. also showed that a cumulative dose of HCQ for 3 months was associated with lower risk of PJP in SLE patients (≤ 14 g, OR = 0.69, 95% CI: 0.21–2.24; > 14 g, OR = 0.20, 95% CI: 0.05–0.71), suggesting that HCQ has a potential protective effect on PJP [34]. In patients and rats, mycophenolate mofetil (MMF) also seems to exhibit anti-PJP activity [38, 39].
Serum albumin is not only a factor related to nutrition but also related to the prognosis of many infectious diseases. A meta-analysis showed that hypoalbuminemia was an independent predictor of poor prognosis in patients with acute illness, with a 137% increased mortality rate for each 10 g/L decrease in the serum albumin concentration [40]. The mortality of non-HIV-surviving PJP patients was also negatively correlated with albumin concentration [20, 41]. Kumagai S et al. reviewed the clinical data of 61 non-HIV PJP patients at multiple institutions and found that both crazy paving GGOs (HR = 10.80, 95% CI: 1.40–83.00, p = 0.02) and low serum albumin (HR = 0.20, 95% CI: 0.07–0.58, p < 0.01) were independent risk factors for mortality [36]. Almost all our enrolled SLE patients had hypoalbuminemia (55/57, 96.5%). Furthermore, the non-survival group had significantly lower serum albumin than the survival group [(19.3 ± 4.1) g/L vs. (25.4 ± 4.9) g/L, p < 0.001].
In our study, the peripheral lymphocyte count (0.4 ± 0.3 × 109/L vs. 1.0 ± 1.7 × 109/L, p = 0.03) and CD4+ cell count (63.7 ± 43.3/µL vs. 167.4 ± 237.3/µL, p = 0.03) were significantly lower in the non-survival group than the survival group. Peripheral lymphocytes play an important role in immune responses against infection. In clinical practice, we should pay more attention to patients treated with corticosteroids and immunosuppressant with lower peripheral lymphocyte count. Lymphocyte subset analysis in patients with peripheral lymphopenia could further evaluate patients’ immune status. A significantly decreased CD4+ cell count was associated with an immunosuppressive state, which predisposes patients to various infectious diseases. CD4+ T lymphocytes include Th1, Th2, Th17, and Treg cells, which are critical components of adaptive immunity in the lung [42]. Low lymphocyte counts and low CD4+ T lymphocyte counts have also been risk factors for PJP infection, and the number of CD4+ cells might be negatively correlated with the pneumocystis load [43, 44].
The guidelines for the prevention and treatment of HIV-PJP patients are well known to physicians. TMPco prophylaxis effectively reduces morbidity and mortality in connective tissue disease (CTD)-PJP patients [45]. However, because of disease heterogeneity and the lack of randomized controlled trials with large samples, there is no established protocol for PJP prophylaxis in CTD patients. The overall incidence of PJP in common SLE patients is low [46], and there are several adverse effects related to TMPco in SLE patients [45]. TMPco prophylaxis is not suggested for every SLE patient. However, the mortality of SLE-PJP patients is high, and the cost of anti-PJP therapy is very high. Selective prevention of PJP should be considered for SLE patients with risk factors for suffering from PJP, including those with lymphopenia, low CD4+ lymphocyte counts or specific immunosuppressant administration [47].
There are several limitations in our study. First, all patients were admitted to a famous tertiary medical center, which would lead to selective bias. Second, it was a retrospective study, therefore, much information could not be collected completely, especially detailed protocol of corticosteroids and immunosuppressants medications. Finally, due to the low incidence rate of SLE-PJP patients, the sample size is relatively limited. A multicenter, well-designed prospective study is expected in near future.
Conclusion
The mortality rate of patients with SLE-PJP was still high. Hyperglycemia or diabetes mellitus, decreased C3, thrombocytopenia were independent survival risk factors for them. For high-risk SLE-PJP patients with poor prognosis, early identification, active prevention medications, and early effective treatments might improve their prognosis.
Data availability
Upon reasonable request, the corresponding author will provide the data.
Abbreviations
- SLE:
-
Systemic lupus erythematosus
- SMR:
-
Standardized mortality rate
- PJP:
-
Pneumocystis jirovecii pneumonia
- HIV:
-
Human immunodeficiency virus
- PUMCH:
-
Peking Union Medical College Hospital
- HRCT:
-
High-resolution computed tomography
- SLICC:
-
Systemic Lupus International Collaborating Clinics
- EULAR:
-
European League Against Rheumatism
- ACR:
-
American College of Rheumatology
- PCR:
-
Polymerase chain reaction
- mNGS:
-
Metagenomic next-generation sequencing
- GMS:
-
Grocott’s methenamine silver
- BALF:
-
Bronchoalveolar lavage fluid
- CMV:
-
Cytomegalovirus
- SD:
-
Standard deviations
- IQRs:
-
Interquartile ranges
- ICU:
-
Intensive care unit
- HAP:
-
Hospital-acquired pneumonia
- GGOs:
-
Ground-glass opacities
- TMPco:
-
Trimethoprim-sulfamethoxazole
- C3:
-
Complement 3
- C4:
-
Complement 4
- HCQ:
-
Hydroxychloroquine
- PBMCs:
-
Peripheral blood mononuclear cells
- MMF:
-
Mycophenolate mofetil
- CTD:
-
Connective tissue disease
References
Barber MRW, Drenkard C, Falasinnu T, Hoi A, Mak A, Kow NY, et al. Global epidemiology of systemic lupus erythematosus. Nat Rev Rheumatol. 2021;17(9):515–32.
Bultink IEM, de Vries F, van Vollenhoven RF, Lalmohamed A. Mortality, causes of death and influence of medication use in patients with systemic lupus erythematosus vs matched controls. Rheumatology (Oxford). 2021;60(1):207–16.
Wu XY, Yang M, Xie YS, Xiao WG, Lin J, Zhou B, et al. Causes of death in hospitalized patients with systemic lupus erythematosus: a 10-year multicenter nationwide Chinese cohort. Clin Rheumatol. 2019;38(1):107–15.
Tselios K, Gladman DD, Sheane BJ, Su J, Urowitz M. All-cause, cause-specific and age-specific standardised mortality ratios of patients with systemic lupus erythematosus in Ontario, Canada over 43 years (1971–2013). Ann Rheum Dis. 2019;78(6):802–6.
Yurkovich M, Vostretsova K, Chen W, Aviña-Zubieta JA. Overall and cause-specific mortality in patients with systemic lupus erythematosus: a meta-analysis of observational studies. Arthritis Care Res (Hoboken). 2014;66(4):608–16.
Arrucha-Cozaya M, Zamora-Zúñiga NC, Miranda-Hernández D, Bustamante-González R, Martínez-Díaz G, Tovar-Rodríguez D, et al. In-hospital mortality and associated factors in patients with systemic lupus erythematosus: analysis over more than 11 years in a reference hospital center. Rheumatol Int. 2023;43(12):2221–31.
Teh CL, Wan SA, Ling GR. Severe infections in systemic lupus erythematosus: disease pattern and predictors of infection-related mortality. Clin Rheumatol. 2018;37(8):2081–6.
Chen D, Xie J, Chen H, Yang Y, Zhan Z, Liang L, et al. Infection in Southern Chinese patients with systemic Lupus Erythematosus: Spectrum, Drug Resistance, outcomes, and risk factors. J Rheumatol. 2016;43(9):1650–6.
Tektonidou MG, Wang Z, Dasgupta A, Ward MM. Burden of serious infections in adults with systemic lupus erythematosus: a National Population-based study, 1996–2011. Arthritis Care Res (Hoboken). 2015;67(8):1078–85.
Sato T, Inokuma S, Maezawa R, Nakayama H, Hamasaki K, Miwa Y, et al. Clinical characteristics of pneumocystis carinii pneumonia in patients with connective tissue diseases. Mod Rheumatol. 2005;15(3):191–7.
Schmidt JJ, Lueck C, Ziesing S, Stoll M, Haller H, Gottlieb J, et al. Clinical course, treatment and outcome of Pneumocystis pneumonia in immunocompromised adults: a retrospective analysis over 17 years. Crit Care. 2018;22(1):307.
Kanj A, Samhouri B, Abdallah N, Chehab O, Baqir M. Host factors and outcomes in hospitalizations for Pneumocystis Jirovecii Pneumonia in the United States. Mayo Clin Proc. 2021;96(2):400–7.
Weng CT, Liu MF, Weng MY, Lee NY, Wang MC, Lin WC, et al. Pneumocystis Jirovecii pneumonia in systemic lupus erythematosus from southern Taiwan. J Clin Rheumatol. 2013;19(5):252–8.
Petri M, Orbai AM, Alarcón GS, Gordon C, Merrill JT, Fortin PR, et al. Derivation and validation of the systemic Lupus International collaborating clinics classification criteria for systemic lupus erythematosus. Arthritis Rheum. 2012;64(8):2677–86.
Aringer M, Costenbader K, Daikh D, Brinks R, Mosca M, Ramsey-Goldman R, et al. 2019 European League Against Rheumatism/American College of Rheumatology classification criteria for systemic lupus erythematosus. Ann Rheum Dis. 2019;78(9):1151–9.
Wang ZG, Liu XM, Wang Q, Chen NF, Tong SQ. A retrospective study of patients with systemic lupus erythematosus combined with pneumocystis jiroveci pneumonia treated with caspofungin and trimethoprim/sulfamethoxazole. Med (Baltim). 2019;98(23):e15997.
Wang WH, Lai CC, Huang YF, Li TH, Tsao YP, Chen WS, et al. Pneumocystis Jirovecii Pneumonia in systemic lupus erythematosus: a Nationwide Cohort Study in Taiwan. Arthritis Care Res (Hoboken). 2022;74(9):1444–50.
Kim SJ, Lee J, Cho YJ, Park YS, Lee CH, Yoon HI, et al. Prognostic factors of Pneumocystis Jirovecii pneumonia in patients without HIV infection. J Infect. 2014;69(1):88–95.
Weng L, Huang X, Chen L, Feng LQ, Jiang W, Hu XY, et al. Prognostic factors for severe pneumocystis jiroveci pneumonia of non-HIV patients in intensive care unit: a bicentric retrospective study. BMC Infect Dis. 2016;16(1):528.
Chen M, Tian X, Qin F, Zhou J, Liu J, Wang M, et al. Pneumocystis Pneumonia in patients with Autoimmune diseases: a retrospective study focused on clinical characteristics and prognostic factors related to death. PLoS ONE. 2015;10(9):e0139144.
Yuan Q, Xing X, Lu Z, Li X. Clinical characteristics and risk factors of infection in patients with systemic lupus erythematosus: a systematic review and meta-analysis of observational studies. Semin Arthritis Rheum. 2020;50(5):1022–39.
Yoon J, Hong SW, Han KD, Lee SW, Shin CM, Park YS, et al. Risk factors of Pneumocystis Jirovecii Pneumonia in patients with inflammatory bowel disease: a Nationwide Population-based study. Gut Liver. 2024;18(3):489–97.
Peleg AY, Weerarathna T, McCarthy JS, Davis TM. Common infections in diabetes: pathogenesis, management and relationship to glycaemic control. Diabetes Metab Res Rev. 2007;23(1):3–13.
Frydrych LM, Bian G, O’Lone DE, Ward PA, Delano MJ. Obesity and type 2 diabetes mellitus drive immune dysfunction, infection development, and sepsis mortality. J Leukoc Biol. 2018;104(3):525–34.
Zhao X, Duan MX, Lu YY, Bai LP, Zhao XY. Short-term prognostic analysis of patients with systemic lupus erythematosus co-infection and comparison of mNGS and conventional microbiological test results. Front Cell Infect Microbiol. 2023;13:1131258.
Barrera-Vargas A, Gómez-Martín D, Merayo-Chalico J, Ponce-de-León A, Alcocer-Varela J. Risk factors for drug-resistant bloodstream infections in patients with systemic lupus erythematosus. J Rheumatol. 2014;41(7):1311–6.
Fernández-Ruiz M, López-Medrano F, Varela-Peña P, Morales JM, García-Reyne A, San Juan R, et al. Hypocomplementemia in kidney transplant recipients: impact on the risk of infectious complications. Am J Transpl. 2013;13(3):685–94.
Lu Z, Li J, Ji J, Da Z. Mortality prediction in systemic lupus erythematosus patients with pulmonary infection. Int J Rheum Dis. 2019;22(6):1077–83.
Nordahl EA, Rydengård V, Nyberg P, Nitsche DP, Mörgelin M, Malmsten M, et al. Activation of the complement system generates antibacterial peptides. Proc Natl Acad Sci U S A. 2004;101(48):16879–84.
Tedesco F. Inherited complement deficiencies and bacterial infections. Vaccine. 2008;26(Suppl 8):I3–8.
Bode J, Dutow P, Sommer K, Janik K, Glage S, Tümmler B, et al. A new role of the complement system: C3 provides protection in a mouse model of lung infection with intracellular Chlamydia psittaci. PLoS ONE. 2012;7(11):e50327.
Walport MJ, Complement. First of two parts. N Engl J Med. 2001;344(14):1058–66.
Yuan Y, Ren J, Gu G, Cao S, Li J. The effect of human complement C3 protein applied at different times in treatment of polymicrobial sepsis. Inflamm Res. 2012;61(6):581–9.
Yeo KJ, Chen HH, Chen YM, Lin CH, Chen DY, Lai CM, et al. Hydroxychloroquine may reduce risk of Pneumocystis pneumonia in lupus patients: a Nationwide, population-based case-control study. BMC Infect Dis. 2020;20(1):112.
Yang Y, Jiang H, Wang C, Jiang N, Wu C, Zhang S, et al. Clinical characteristics and prognoses of patients with systemic Lupus Erythematosus hospitalized for pulmonary infections. Front Med (Lausanne). 2021;8:732681.
Henriet SS, Jans J, Simonetti E, Kwon-Chung KJ, Rijs AJ, Hermans PW, et al. Chloroquine modulates the fungal immune response in phagocytic cells from patients with chronic granulomatous disease. J Infect Dis. 2013;207(12):1932–9.
Feldman CH, Hiraki LT, Winkelmayer WC, Marty FM, Franklin JM, Kim SC, et al. Serious infections among adult Medicaid beneficiaries with systemic lupus erythematosus and lupus nephritis. Arthritis Rheumatol. 2015;67(6):1577–85.
Azevedo LS, Castro MC, Paula FJ, Ianhez LE, David-Neto E. Mycophenolate mofetil may protect against Pneumocystis carinii pneumonia in renal transplanted patients. Rev Inst Med Trop Sao Paulo. 2005;47(3):143–5.
Oz HS, Hughes WT. Novel anti-pneumocystis carinii effects of the immunosuppressant mycophenolate mofetil in contrast to provocative effects of tacrolimus, sirolimus, and dexamethasone. J Infect Dis. 1997;175(4):901–4.
JVincent JL, Dubois MJ, Navickis RJ, Wilkes MM. Hypoalbuminemia in acute illness: is there a rationale for intervention? A meta-analysis of cohort studies and controlled trials. Ann Surg. 2003;237(3):319–34.
Kumagai S, Arita M, Koyama T, Kumazawa T, Inoue D, Nakagawa A, et al. Prognostic significance of crazy paving ground grass opacities in non-HIV pneumocystis jirovecii pneumonia: an observational cohort study. BMC Pulm Med. 2019;19(1):47.
Kolls JK. CD4(+) T-cell subsets and host defense in the lung. Immunol Rev. 2013;252(1):156–63.
Iriart X, Witkowski B, Courtais C, Abbes S, Tkaczuk J, Courtade M, et al. Cellular and cytokine changes in the alveolar environment among immunocompromised patients during pneumocystis jirovecii infection. Med Mycol. 2010;48(8):1075–87.
Li Y, Ghannoum M, Deng C, Gao Y, Zhu H, Yu X, et al. Pneumocystis pneumonia in patients with inflammatory or autoimmune diseases: usefulness of lymphocyte subtyping. Int J Infect Dis. 2017;57:108–15.
Park JW, Curtis JR, Moon J, Song YW, Kim S, Lee EB. Prophylactic effect of trimethoprim-sulfamethoxazole for pneumocystis pneumonia in patients with rheumatic diseases exposed to prolonged high-dose glucocorticoids. Ann Rheum Dis. 2018;77(5):644–9.
Gupta D, Zachariah A, Roppelt H, Patel AM, Gruber BL. Prophylactic antibiotic usage for Pneumocystis Jirovecii pneumonia in patients with systemic lupus erythematosus on cyclophosphamide: a survey of US rheumatologists and the review of literature. J Clin Rheumatol. 2008;14(5):267–72.
Wolfe RM, Peacock JE Jr. Pneumocystis Pneumonia and the rheumatologist: which patients are at risk and how can PCP be prevented? Curr Rheumatol Rep. 2017;19(6):35.
Acknowledgements
We would like to thank the patients for their assistance. And we would like to thank the support provided by the National High Level Hospital Clinical Research Funding (grant number 2022‐PUMCH‐C‐069, 2022‐PUMCH‐A‐009).
Funding
This study was supported by the National High Level Hospital Clinical Research Funding under Grant [numbers 2022-PUMCH-C-069, 2022-PUMCH-A-009].
Author information
Authors and Affiliations
Contributions
YJ.S. and H.H. conceived and designed the study. H.H. and C.S. supervised and managed the manuscript. YJ.S., RX.C., HL.S., K.X., ZY.L., MQ.W., and H.H. performed the study and data analysis. H.H. and Y.S. wrote the first draft. All the authors have read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Ethics Committee of Peking Union Medical College Hospital (K5596) in accordance with the Declaration of Helsinki. Written informed consent from each patient was waived because our study was conducted using anonymized health care data, which met the IRB’s minimal risk waiver criteria.
Consent for publication
Not Applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Shi, Y., Chen, R., Sun, H. et al. Prognostic analysis of concurrent Pneumocystis jirovecii pneumonia in patients with systemic lupus erythematosus: a retrospective study. BMC Infect Dis 24, 874 (2024). https://doi.org/10.1186/s12879-024-09757-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-024-09757-4