Abstract
Background
Acute respiratory infections are a leading cause of morbidity and mortality in children. However, studies on the prevalence of respiratory viruses among children with acute respiratory infections in Kunming, China, are lacking. Therefore, we aimed to investigate the epidemiological characteristics of respiratory pathogens among children with acute respiratory infections in Kunming during the coronavirus disease 2019 pandemic.
Methods
Nasopharyngeal swab samples were collected from 4956 children with acute respiratory infections at Yunnan Provincial First People’s Hospital between January 2020 and December 2022, patients with COVID-19 were excluded from the study. Multiplex reverse transcription polymerase chain reaction was used to detect respiratory pathogens.
Results
The frequency of respiratory pathogens among children was significantly lower in 2020 than in 2021 and 2022. The following pathogens had the highest prevalence rates (in descending order) from 2020 to 2022: HRV > RSV > PIV > ADV > MP; HRV > RSV > HADV > PIV > MP and HRV > Mp > HADV > H3N2 > HMPV. The overall frequency of respiratory pathogens exhibited an inverted U-shape with increasing age among the children. Human bocavirus, human parainfluenza virus, and human respiratory syncytial virus were the dominant respiratory viruses in children aged ≤ 3 years, whereas Mycoplasma pneumoniae was the dominant respiratory pathogen in children aged > 3 years. HRV has the highest prevalence and is the main pathogen of mixed infection. The prevalence of the influenza A virus has decreased significantly, whereas HRSV and Mp are found to be seasonal.
Conclusions
Our findings offer an objective evaluation of transmission dynamics and epidemiological shifts in respiratory pathogens during the coronavirus disease 2019 pandemic in Kunming, serving as a basis for informed decision-making, prevention, and treatment strategies.
Similar content being viewed by others
Background
Acute respiratory infections (ARIs) are one of the leading causes of childhood mortality in children aged less than 5 years worldwide [1], and up to 90% of ARIs in children are attributable to respiratory viruses [2]. The lack of an etiological diagnosis is the primary reason why over 50% of ARI cases receive unnecessary or inappropriate antibiotic prescriptions [3]. Given that children with ARIs often exhibit similar clinical symptoms, the etiological diagnosis of ARIs requires clinical laboratory confirmation and cannot be identified based on clinical symptoms and signs alone [4, 5]. Owing to the advancements in molecular biology technology over the past twenty years, several newly discovered viruses, including human bocavirus (Boca), human respiratory syncytial virus (HRSV), human metapneumovirus (HMPV), human parainfluenza virus (HPIV), and human coronavirus (HCOV), have been identified [2, 6]. Respiratory viral infections are primarily spread through contact and droplet routes [7]. Moreover, these infections are generally considerably more prevalent in children than in adults, especially as co-infections with different viral species [8].
The prevalence of respiratory viruses in children with ARIs varies across regions and seasons [9]. Kunming is the capital of Yunnan Province in Southwest China, with a resident population of 8.46 million. Its advantageous geographical location contributes to its pleasant climate. Although the Han Chinese constitute the majority, Kunming is a city with a diverse ethnic composition, with significant populations of Yi, Bai, Hani, Dai, and other ethnic minority groups residing in it. To the best of our knowledge, studies on the prevalence of respiratory viruses among children with ARIs in Kunming are lacking. Therefore, the epidemiological shifts in respiratory viruses among children with ARIs must be examined to facilitate the establishment of a comprehensive spectrum of respiratory viruses and the formulation of precise diagnosis and treatment strategies for ARIs.
As a novel viral respiratory disease, coronavirus disease 2019 (COVID-19) presents a huge challenge to global health care [10]. A range of non-pharmaceutical interventions (NPIs) have been implemented globally to control the spread of COVID-19, such as mask use, hand hygiene, social distancing, travel restrictions, school closures, screening, and isolation [11]. These measures were implemented gradually in Kunming from February 2020 and were ultimately revoked entirely in December 2022. Data from several studies indicate that the NPIs have led to an overall decrease in the spread of respiratory viruses [12]. However, with the lifting of the NPIs, some other respiratory viruses have gradually developed an epidemic propensity [13]. Thus, it is important to investigate the epidemiological changes in respiratory viruses during the COVID-19 pandemic.
In this study, we aimed to investigate the epidemiological characteristics of respiratory pathogens among children with ARIs in Kunming during the COVID-19 pandemic. This study provides important insights into better understanding the epidemiological shifts in respiratory viruses among children with ARIs during the COVID-19 pandemic in Kunming, offers a scientific foundation for enhancing the quality of clinical diagnosis and treatment, and establishes evidence to inform more effective epidemic prevention strategies for the post-pandemic era.
Methods
Study population and sample collection
In total, 4956 patients who were diagnosed with ARIs were continuously recruited at the First People’s Hospital of Yunnan Province from January 2020 to December 2022. The patients exhibited symptoms of acute respiratory tract diseases, including cough, sore throat, flu-like symptoms (such as fever, fatigue, headache, nasal congestion, and a runny nose), and difficulty breathing. The inclusion criteria were as follows: (1) age < 18 years; (2) diagnosis of an ARI; and (3) received no clinical treatment prior to sample collection. Importantly, for each patient, only the results of the first specimen were collected and analyzed during the course of the disease [12, 14]. Considering the extremely low frequency of COVID-19, therefore, Patients with COVID-19 were excluded from the study. This research was approved by the Institutional Review Board of the First People’s Hospital of Yunnan Province and carried out strictly in accordance with the Declaration of Helsinki. Informed consent was obtained from the parents or guardians of all participants. Data were stored and analyzed anonymously.
Throat swabs were collected from each patient and stored in sterile sample tubes containing cell preservation solution (HEALTH Gene Technologies Co., Ltd., Ningbo, China). Specimens were transported, stored at 4℃, and tested for respiratory viruses within 24 h of collection.
Nucleic acid extraction and purification
Nucleic acid was extracted from clinical samples using a Nucleic Acid Extraction or Purification Kit (HEALTH Gene Technologies Co., Ltd., Ningbo, China), Nucleic acid extraction and Purification reagents lots:211,109,002、220,118,010、220,210,005. The entire extraction process was conducted using automatic nucleic acid extraction equipment. Nucleic acid was used to detect respiratory pathogens and stored at − 80℃.
Detection of respiratory pathogens
The respiratory pathogens were detected using a Multiple Detection Kit for Thirteen Respiratory Pathogens (13× kit; HEALTH Gene Technologies Co., Ltd., Ningbo, China), detection reagents lots: 201,117,005, 210,323,004, 220,329,007. The kit utilizes multiplex reverse transcription polymerase chain reaction (RT-PCR) amplification and automatic capillary electrophoresis to identify 11 respiratory pathogens, including human bocavirus(Boca), human respiratory syncytial virus(HRSV), human rhinovirus (HRV), human coronavirus(HCOV), human metapneumovirus(HMPV), human parainfluenza virus(HPIV), human adenovirus (HADV), influenza virus type A (InfA), InfA-H1N1, InfA-H3N2, influenza virus type B (InfB), Mycoplasma Pneumoniae (Mp), and chlamydia (Ch, including Chlamydia Trachomatis and Chlamydia Pneumoniae), in a single analysis [15]. HCOV detectable subtypes of coronavirus, excluding severe acute respiratory syndrome coronavirus 2, include 229E, NL63, HKU1, and OC43.
Statistical analysis
Statistical analysis was performed using SPSS statistical software (version 25.0, SPSS, Inc., Chicago, IL, USA). The chi-square test was used to analyze the differences in the frequency of respiratory pathogens between various groups (i.e., sex, age, or season). A descriptive analysis was performed using absolute and relative frequencies (percentages) of the variables studied. Differences were considered statistically significant at P-values < 0.05.
Results
Overall frequency of respiratory pathogens
A total of 4956 patients with ARIs, excluding COVID-19 positives, were recruited, comprising 1158, 2128, and 1670 patients enlisted in 2020, 2021, and 2022, respectively. The overall frequency of respiratory pathogens in children with ARIs from 2020 to 2022 was 58.17% (95% confidence interval (CI), 56.80–59.55%) (Table 1). The overall frequency was significantly higher in 2022 (59.40%, 95% CI, 57.04–61.76%) and 2021 (61.65%, 95% CI, 59.59–63.72%) than in 2020 (50.00%, 95% CI, 47.12–52.88%) (P < 0.001). Although the proportion of boys was higher than that of girls (57.67% vs. 42.33%), the overall frequency of respiratory pathogens did not differ significantly between the sexes (59.31% vs. 56.63%, P = 0.059).
Distribution of each Respiratory Pathogen
As shown in Table 1, the five most detected pathogens were HRV (21.29%, 95% CI, 20.15–22.43%), HRSV (6.90%, 95% CI, 6.19–7.61%), HADV (6.70%, 95% CI, 6.00–7.40%), Mp (6.17%, 95% CI, 5.50–6.84%), and HPIV (5.51%, 95% CI, 4.87–6.14%). Although the frequency of respiratory pathogens from throat swab samples of children with ARIs has been changing since 2020, that of HRV remained the highest of all pathogens. During the COVID-19 pandemic, the frequencys of HRSV and HPIV gradually decreased. The frequency of HRSV decreased from 9.24% in 2020 to 3.05% in 2022 (P < 0.0001), and that of HPIV dropped from 6.65% in 2020 to 4.07% in 2022 (P = 0.002). Conversely, the frequencys of HMPV and Mp exhibited a gradual increase, from 1.38% in 2020 to 4.67% in 2022 and from 2.42% in 2020 to 10.18% in 2022, respectively (P < 0.0001). Moreover, the frequency of HADV was only 3.54% in 2020 but significantly increased in 2021 and 2022 (8.04% and 7.19%, respectively; P < 0.0001). The frequency of InfA was markedly low in 2020 (1.47%) and 2021 (0.24%) but significantly increased to 5.27% in 2022 (P < 0.0001), and the H3N2 type was more prevalent than the H1N1 type in 2022 (4.97% vs. 0.06%, P < 0.0001) (Fig. 1).
Distribution of each respiratory pathogen among children with acute respiratory infections in Kunming, 2020–2022. The length of the colored bars and the number indicate the frequency of each pathogen. The frequencies of the H1N1 and H3N2 subtypes of influenza A were calculated. From 2020 to 2021, the frequencies of some pathogens increased significantly, including Rhinovirus (20.4% vs. 24.3%, P = 0.011), Metapneumovirus (1.4% vs. 4.5%, P < 0.0001), Adenovirus (3.5% vs. 8.0%, P < 0.0001), Influenza B (1.2% vs. 2.4%, P = 0.016), and Mycoplasma pneumoniae (2.4% vs. 5.1%, P < 0.0001). Conversely, the frequencies of some pathogens decreased significantly from 2020 to 2021, including coronavirus (1.9% vs. 0.6%, P = 0.001) and influenza A (1.5% vs. 0.2%, P < 0.0001). Furthermore, the frequencies of some pathogens increased significantly from 2021 to 2022, including coronavirus (0.6% vs. 1.8%, P = 0.001) and Mycoplasma pneumoniae (5.1% vs. 10.2%, P < 0.0001). However, the frequencies of some pathogens decreased significantly from 2021 to 2022, including rhinovirus (24.3% vs. 18.1%, P < 0.0001), parainfluenza (6.0% vs. 4.1%, P = 0.007), and respiratory syncytial virus (8.6% vs. 3.1%, P < 0.0001)
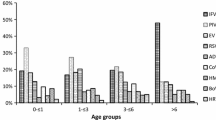
Frequency of respiratory pathogens among various age groups
As shown in Table 2, patients were categorized into five age groups: 0–28 days, 1–12 months, 1–3 years, 4–6 years, and ≥ 7 years [12]. A comparison of the frequencies of respiratory pathogens across these age groups revealed an inverted U-shaped trend in pathogen prevalence with age. Specifically, the highest frequency was observed in children aged 1–3 years (72.04%), followed by those aged 4–6 years (67.21%) and 1–12 months (56.96%). Notably, the rate was considerably lower in children aged ≥ 7 years (42.70%) and infants aged 0–28 days (20.78%). HRV was the most prevalent respiratory pathogen in all age groups. The frequency of HRV demonstrated a significant increase with age among children under 3 years, rising from 11.69% in infants aged 0–28 days to 26.73% in children aged 1–3 years (P = 0.003). However, it gradually decreased in children aged over 3 years, especially in those aged ≥ 7 years, decreasing significantly to 16.18% (P < 0.0001). Furthermore, the prevalence of other respiratory pathogens also varied across different age groups. The frequency of HRSV was the highest in infants aged 1–12 months and the lowest among children aged ≥ 7 years (16.98% vs. 1.01%, P < 0.0001). Only three pathogens, namely HRV (11.69%), Boca (1.30%), and HRSV (7.79%), were detected in newborns aged 0–28 days. Therefore, except for newborns aged 0–28 days, the frequency of HADV was the lowest in infants aged 1–12 months and the highest in children aged 4–6 years (2.85% vs. 12.13%, P < 0.0001). The frequencys of InfB and Mp exhibited a gradual increase with age, rising from 0.99% and 1.31–3.09% and 10.96%, respectively.
We also analyzed the frequency of respiratory pathogens in infants aged ≤ 3 years and children aged > 3 years. As shown in Table 2, the overall frequency of respiratory pathogens among infants aged ≤ 3 years was significantly higher than that among children aged > 3 years (64.82% vs. 51.66%, P < 0.0001). The frequencies of HRV, Boca, HPIV, and HRSV in infants ≤ 3 years were all significantly higher than those in children aged > 3 years (22.87% vs. 19.74%, P = 0.007; 2.49% vs. 0.28%, P < 0.0001; 8.44% vs. 2.64%, P < 0.0001; and 12.03% vs. 1.88%, P < 0.0001; respectively), whereas that of Mp was significantly lower in infants aged ≤ 3 years than in children aged > 3 years (2.49% vs. 9.79%, P < 0.0001).
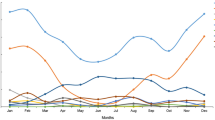
Seasonal distribution of respiratory pathogens
We further investigated the seasonal distribution of common respiratory pathogens during the three research periods from 2020 to 2022 (Fig. 2). As HRV was the most common respiratory pathogen, its spread was detected in every season from January 2020 to December 2022, with an activity peak in June and July of each year. Similarly, during the three research periods, the spread of HADV was detected throughout the year. The frequency of HADV was distributed almost evenly throughout 2020, except for a slight increase in March. The epidemic peak of HADV in 2021 and 2022 primarily occurred in winter, with a notable maximum activity observed in December 2021 and January 2022, amounting to 16.01% and 18.82%, respectively. HMPV exhibited a different trend; it was scarcely detected from February to August 2020. In contrast, the virus was consistently detected throughout 2021 and 2022, and peaks of the epidemic were observed in January and December 2021, as well as in July and August 2022. The spread of HRSV and Mp exhibited an obvious seasonal distribution pattern, with a higher prevalence in the winter months. InfA was detected only in January (12.60%) and February (1.96%) throughout 2020, but was barely detected after February 2020. However, no new influenza incidences were detected until March 2021. The frequency of InfA was low in 2021, and influenza cases were detected only in March (0.64%) and September (3.51%). In contrast, except for April and December, the spread of InfA was detected throughout 2022, with an activity peak in July (11.11%) and August (13.86%).
Coinfection Pattern of respiratory pathogens
We also analyzed the coinfection pattern of respiratory pathogens in children with ARIs. Although single infection was the predominant pattern, 7.77% (385/4956) of children with ARIs were infected with two pathogens at the same time. Moreover, there was a high viral-viral coinfection rate in children, and Rhinovirus coinfection with other pathogens was the most common pattern. During the research periods spanning 2020 to 2022, the most prevalent co-infection patterns were HRV-HADV (0.99%), HRV-HPIV (0.89%), HRV-HRSV (0.89%), HRV-Mp (0.77%), and HRV-HMPV (0.69%). The coinfection pattern underwent annual changes. Specifically, in 2020, the dominant patterns were HRV-HPIV (0.95%) and HRV-HRSV (0.95%). In 2021, HRV-HADV (1.46%) emerged as the most common, followed by HRV-HRSV (1.22%) and HRV-HMPV (1.13%). Notably, in 2022, the coinfection rate of HRV-Mp reached its peak at 1.32% among children. Comprehensive details are presented in Table 3; Fig. 3.
Coinfection pattern of respiratory pathogens in children with acute respiratory infections. Coinfection rates were calculated pairwise. The numerator was the number of patients co-infected with both pathogens, and the denominator was the total number of patients who were tested for both pathogens. The bigger size and darker color of the circles indicate higher coinfection rates between two pathogens
Boca, human bocavirus; Ch, chlamydia; HADV, human adenovirus; HCOV, human coronavirus; HMPV, human metapneumovirus; HPIV, human parainfluenza virus; HRSV, human respiratory syncytial virus; HRV, human rhinovirus; InfA, influenza A; InfB, influenza B; Mp, Mycoplasma pneumoniae
Discussion
During COVID-19, many restrictive public health measures were implemented worldwide, which dramatically impacted the spread of other common respiratory pathogens. However, as the COVID-19 pandemic progressed, these measures were gradually lifted. In this study, we investigated the prevalence of respiratory pathogens among children with ARIs during the COVID-19 pandemic, and analyzed and compared the epidemiological changes in 13 respiratory pathogens among children of different ages between 2020 and 2022 to determine the impact of the COVID-19 pandemic on other common respiratory pathogens. This study showed the lowest prevalence in 2020, followed by a rebound in prevalence. In addition, Boca, HPIV, and HRSV were the dominant respiratory viruses in young children, whereas MP was the dominant respiratory pathogen in children aged > 3 years. The prevalence of influenza A virus decreased significantly, whereas HRV remained highly prevalent throughout the study period. Our results indicated that the frequency of respiratory pathogens among children with ARIs was significantly lower in 2020 than in 2021 and 2022, followed by a rebound in prevalence, and coincides with the implementation of NPI measures and subsequent relaxation, which is consistent with previous research [12, 13, 16]. One possible explanation for this phenomenon is that implementing restrictive public health measures over a long period at the beginning of the pandemic curtailed the spread of other respiratory pathogens to some extent [17]. This impact was short-lived, as the frequency of common respiratory pathogens among affected children increased as various public health measures were lifted in the subsequent two years. Although the transmission of common respiratory pathogens in children was disrupted during the COVID-19 pandemic, the duration and magnitude of this disruption varied among pathogens. In 2020, the prevalence of HADV and Mp was low (3.54% and 2.42%, respectively) but gradually increased from 2021 onwards, with their frequencys increasing to 8.04% and 5.08%, respectively. By 2022, the HADV frequency decreased slightly to 7.19%, whereas the Mp frequency continued to increase to 10.18%. In contrast, the transmissions of Boca and Ch have been maintained at low levels since 2020 and were not significantly affected by the COVID-19 pandemic. The transmission of InfA was maintained at low levels in 2020 and 2021, with frequencys of 1.47% and 0.24%, respectively. However, the transmission was more active in 2022, especially the H3N2 strain, with the frequency increasing from 1.30% in 2020 to 4.97% currently. Similarly, transmission of InfB remained at low levels during the early stages of the pandemic, with frequencys of 1.21% in 2020, but its frequency gradually increased to 2.44% and 2.99% in 2021 and 2022, respectively. Implementing restrictive public health measures at the beginning of the pandemic resulted in a prolonged period without natural exposure to influenza viruses, and the decreased transmission of influenza virus over the past two years may foreshadow the severity of the upcoming influenza season. Lower levels of herd immunity, especially in younger children, may predict more widespread disease and potentially more severe illness when the transmission of the influenza virus resumes [18]. Therefore, transmission levels of common respiratory pathogens may continue to undergo alterations as public health measures are adjusted, and further evaluation is warranted to assess changes in the transmission of each common pathogen in the post-pandemic era.
The changes observed in the level of HRV transmission warrant attention. Even during the first half of 2020, which was a critical period for COVID-19 prevention and control, the frequency of HRV reached 9.37% (31/331), which was considerably higher than that of other pathogens. In the second half of 2020, the frequency of HRV significantly escalated to 24.55% (203/827) and subsequently sustained high levels in the ensuing years (24.30% in 2021 and 18.18% in 2022). Importantly, under strict epidemic prevention and control measures, maintaining a higher frequency may be intricately linked to the stability, diversity, and persistence of HRV. As a non-enveloped virus, the unique transmission patterns and shifts in predominant strains of HRV warrant further investigation [16, 19].
The present study included more boys than girls (57.67% vs. 42.33%). However, similar frequencys of respiratory pathogens were observed in both sexes (59.31% vs. 56.63%, P = 0.059), suggesting that respiratory pathogen infection is not related to sex but may be influenced by age in children. Our findings demonstrated that the overall frequency of respiratory pathogens was significantly higher among infants and children aged ≤ 3 years than among children aged > 3 years (64.82% vs. 51.66%, P < 0.0001), with the overall frequency of respiratory pathogens among children aged 1–3 years being the highest among all age groups (72.04%). A possible reason for this observation is that children aged ≤ 3 years are immunonaive and more susceptible to pathogens. Children of different ages have different levels of immunity, experience different living environments, and exhibit different behaviors, contributing to differences in the prevalence of common respiratory pathogens among age groups [20]. Our results suggest that children aged ≤ 3 years must be monitored for Boca, HPIV, and HRSV infections, which are detected at significantly higher rates in this age group than in those aged > 3 years. In contrast, children aged > 3 years must be monitored for Mp, a pathogen whose frequency is significantly higher in these children than in those aged ≤ 3 years. A previous study reported that the prevalence of Mp was highest in school-aged children, with some transmission among children aged 1–5 years, whereas infants and toddlers aged > 1 year were rarely infected by Mp [21]. Consistently, our results revealed that the frequency of Mp in infants and children aged < 1 year was only 1.21% (12/990), whereas that among schoolchildren aged ≥ 7 years was 10.96%, which was the highest among all age groups. Our findings suggest that Mp affects children aged < 1 year, despite the low frequency observed in these children. In addition, the differences in frequencies of HRV in children of different ages were not compared, and it was detected at relatively high rates in children of all ages, making it one of the most common respiratory pathogens in children with ARIs.
Seasonality is a major factor affecting pathogen transmission [22]. Our findings suggest a clear seasonal distribution of HRSV and Mp transmission, with relatively high frequencies in winter. In contrast, HRV was prevalent throughout the year, with peak transmission from June to July each year. Notably, InfA was detected solely in January (12.60%) and February (1.96%) of 2020, and almost no InfA was observed after February 2020, with no new influenza cases recorded until March 2021. However, the overall frequency of InfA in 2021 was low, with cases detected only in March (0.64%) and September (3.51%) 2021. The spread of InfA was detected throughout 2022, except in April and December, with peak activity in July (11.11%) and August (13.86%). However, from 2020 to 2021, the infection rate of RSV in children aged < 3 years remained high, which was inconsistent with that reported in Netherlands and Italy [23, 24], indicating that there were great differences in prevalence among regions. In 2022, with the rebound of the influenza virus, the prevalence of RSV decreased significantly. The prevalence of RSV and influenza showed a negative correlation trend, which was consistent with the Netherlands [25], but the related interference needs further study. Concerning seasonal epidemics of influenza and HRSV are the cause of substantial morbidity and mortality among children [26].Therefore, We need to be vigilant for outbreaks of RSV and influenza, whereas closely monitoring seasonal and epidemiological changes in common respiratory pathogens.
To the best of our knowledge, the present study is the first to focus on the epidemiological characteristics of respiratory pathogens among children with ARIs in the Kunming area during the COVID-19 pandemic. The study data were obtained during the COVID-19 pandemic, and a cohort of children with relatively high frequencies of respiratory pathogens was selected, and excluded patients with COVID-19. The uniform background data on individuals in this population enables an objective and accurate assessment of the transmission dynamics in respiratory pathogens in this region, and provides important insights to better understand the epidemiological shifts in respiratory viruses among children with ARIs during the COVID-19 pandemic in Kunming, offers a scientific foundation for enhancing the quality of clinical diagnosis and treatment, and establishes evidence to inform more effective epidemic prevention strategies for the post-pandemic era.
However, this study had limitations. First, the source of samples was limited, limiting our comprehensive understanding of the epidemiological dynamics of respiratory pathogens in Yunnan Province. Second, owing to the lack of data on the detection of respiratory pathogens in children with ARIs before COVID-19, the prevalence of respiratory pathogens before and after the pandemic could not be compared. Finally, bacterial pathogens were not detected in this study owing to limitations in laboratory testing conditions.
Conclusions
In conclusion, we analyzed the epidemiological characteristics of respiratory pathogens, including the overall frequency, age distribution, seasonal distribution, and coinfection pattern, among children with ARIs in Kunming during the COVID-19 pandemic. Our results offer an objective evaluation of transmission dynamics and epidemiological shifts in respiratory pathogens during the COVID-19 pandemic in the Kunming area. The initial understanding of the interference between respiratory pathogens has enhanced our understanding of the interaction between pathogens and serves as a basis for informed decision-making, prevention, and treatment strategies.
Data availability
The data are available from the corresponding authors on reasonable request.
Abbreviations
- ARI:
-
Acute respiratory infections.
- Boca:
-
Human bocavirus
- Ch:
-
Chlamydia
- COVID-19:
-
Coronavirus disease 2019.
- HADV:
-
Human adenovirus.
- HCOV:
-
Human coronavirus.
- HMPV:
-
Human metapneumovirus.
- HPIV:
-
Human parainfluenza virus.
- HRSV:
-
Human respiratory syncytial virus.
- HRV:
-
Human rhinovirus.
- InfA:
-
Influenza virus type A.
- InfB:
-
Influenza virus type B.
- Mp:
-
Mycoplasma Pneumoniae.
- NPI:
-
Non-pharmaceutical interventions.
- RT-PCR:
-
Reverse transcription polymerase chain reaction.
References
Williams BG, Gouws E, Boschi-Pinto C, Bryce J, Dye C. Estimates of world-wide distribution of child deaths from acute respiratory infections. Lancet Infect Dis. 2002;2:25–32.
Jartti T, Jartti L, Ruuskanen O, Söderlund-Venermo M. New respiratory viral infections. Curr Opin Pulm Med. 2012;18:271–8.
Tregoning JS, Schwarze J. Respiratory viral infections in infants: causes, clinical symptoms, virology, and immunology. Clin Microbiol Rev. 2010;23:74–98.
Kesson AM. Respiratory virus infections. Paediatr Respir Rev. 2007;8:240–8.
Kurskaya O, Ryabichenko T, Leonova N, Shi W, Bi H, Sharshov K, et al. Viral etiology of acute respiratory infections in hospitalized children in Novosibirsk City, Russia (2013–2017). PLoS ONE. 2018;13:e0200117.
Debiaggi M, Canducci F, Ceresola ER, Clementi M. The role of infections and coinfections with newly identified and emerging respiratory viruses in children. Virol J. 2012;9:1–18.
Liang M, Gao L, Cheng C, Zhou Q, Uy JP, Heiner K, et al. Efficacy of face mask in preventing respiratory virus transmission: a systematic review and meta-analysis. Travel Med Infect Dis. 2020;36:101751.
Mandelia Y, Procop GW, Richter SS, Worley S, Liu W, Esper F. Dynamics and predisposition of respiratory viral co-infections in children and adults. Clin Microbiol Infect. 2021;27:631. .e1-631.e6.
Dong W, Chen Q, Hu Y, He D, Liu J, Yan H, et al. Epidemiological and clinical characteristics of respiratory viral infections in children in Shanghai, China. Arch Virol. 2016;161:1907–13.
Ciotti M, Ciccozzi M, Terrinoni A, Jiang WC, Wang CB, Bernardini S. The COVID-19 pandemic. Crit Rev Clin Lab Sci. 2020;57:365–88.
Perra N. Non-pharmaceutical interventions during the COVID-19 pandemic: a review. Phys Rep. 2021;913:1–52.
Ye Q, Wang D. Epidemiological changes of common respiratory viruses in children during the COVID-19 pandemic. J Med Virol. 2022;94:1990–97.
Wan WY, Thoon KC, Loo LH, Chan KS, Oon LLE, Ramasamy A, et al. Trends in respiratory virus infections during the COVID-19 pandemic in Singapore, 2020. JAMA Netw Open. 2021;4:e2115973–2115973.
Hall CB, Weinberg GA, Iwane MK, et al. The burden of respiratory syncytial virus infection in young children[J]. N Engl J Med. 2009;360(6):588–98.
Zhao MC, Li GX, Zhang D, Zhou HY, Wang H, Yang S, et al. Clinical evaluation of a new single-tube multiplex reverse transcription PCR assay for simultaneous detection of 11 respiratory viruses, Mycoplasma pneumoniae and Chlamydia in hospitalized children with acute respiratory infections. Diagn Microbiol Infect Dis. 2017;88:115–59.
Chow EJ, Uyeki TM, Chu HY. The effects of the COVID-19 pandemic on community respiratory virus activity. Nat Rev Microbiol. 2023;21:195–210.
Oster Y, Michael-Gayego A, Rivkin M, Levinson L, Wolf DG, Nir-Paz R. Decreased prevalence rate of respiratory pathogens in hospitalized patients during the COVID-19 pandemic: possible role for public health containment measures? Clin Microbiol Infect. 2020;27:811–2.
Olsen SJ, Winn AK, Budd AP, Prill MM, Steel J, Midgley CM, et al. Changes in influenza and other respiratory virus activity during the COVID-19 pandemic—United States, 2020–2021. MMWR Morb Mortal Wkly Rep. 2021;70:1013–19.
Kim HM, Lee EJ, Lee NJ, Woo SH, Kim JM, Rhee JE, et al. Impact of Coronavirus Disease 2019 on respiratory surveillance and explanation of high detection rate of human rhinovirus during the pandemic in the Republic of Korea. Influenza Other Respir Viruses. 2021;15:721–31.
Liao X, Hu Z, Liu W, Lu Y, Chen D, Chen M, et al. New epidemiological and clinical signatures of 18 pathogens from respiratory tract infections based on a 5-year study. PLoS ONE. 2015;10(9):e0138684.
Defilippi A, Silvestri M, Tacchella A, Giacchino R, Melioli G, Di Marco E, et al. Epidemiology and clinical features of Mycoplasma pneumoniae infection in children. Respir Med. 2008;102:1762–8.
Shaman J, Kohn M. Absolute humidity modulates influenza survival, transmission, and seasonality. Proc Natl Acad Sci USA. 2009;106:3243–8.
van Asten L, Bijkerk P, Fanoy E, an Ginkel A, Suijkerbuijk A, van der Hoek W, Meijer A, et al. Early occurrence of influenza A epidemics coincided with changes in occurrence of other respiratory virus infections. Influenza Other Respir Viruses. 2016;10:14–26.
Buonsenso D. Disease and age-related inequalities in paediatric research, funding and communication: lessons from the COVID-19 pandemic. Acta Paediatr. 2020;109:1932–3.
Di Mattia G, Nenna R, Mancino E, Rizzo V, Pierangeli A, Villani A, et al. During the COVID-19 pandemic where has respiratory syncytial virus gone?[J]. Pediatr Pulmonol. 2021;56:3106–9.
Buchholz U, Lehfeld AS, Tolksdorf K, Cai W, Reiche J, Biere B, et al. Respiratory infections in children and adolescents in Germany during the COVID-19 pandemic. J Health Monit. 2023;8:20–38.
Acknowledgements
We thank the members of the Molecular Biology Laboratory of the Laboratory Department of the First People’s Hospital of Yunnan Province for their help in detecting respiratory pathogens, and all the participants for their contribution to the study.
Funding
This work was supported by the National Natural Science Foundation of China (grant number 82260395); Yunnan Provincial Department of Science and Technology-Kunming Medical University Applied Fundamental Research Joint Special Fund (grant number 202201AY070001-245); Yunnan Provincial Key Laboratory of Clinical Virology (grant number 2023A4010403-05).
Author information
Authors and Affiliations
Contributions
Guiqian Zhang integrated the data and wrote the manuscript; Yu Zhang contributed the revision of the manuscript; Limei Ba, Luping Liu, Ting Su responsible for data collection and analysis; Ziqin Dian and Yi Sun supplied the support, resources, and supervision required to perform the study. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This research was approved by the Institutional Review Board of the First People’s Hospital of Yunnan Province and carried out strictly in accordance with the Declaration of Helsinki. Informed consent was obtained from all participants and from their legal guardians who were aged < 16 years. Data were stored and analyzed anonymously.1)population, place and period of study: In total, 4956 patients who were diagnosed with ARIs were continuously recruited at the First People’s Hospital of Yunnan Province from January 2020 to December 2022. The patients exhibited symptoms of acute respiratory tract diseases, including cough, sore throat, flu-like symptoms (such as fever, fatigue, headache, nasal congestion, and a runny nose), and difficulty breathing. The inclusion criteria were as follows: (1) age under 18 years; (2) diagnosis of an ARI; and (3) received no clinical treatment prior to sample collection. Importantly, for each patient, only the results of the first specimen were collected and analyzed during the course of the disease [12]. Patients with COVID-19 were excluded from the study. 2) Sample collection: Throat swabs were collected from each patient and stored in sterile sample tubes containing cell preservation solution (HEALTH Gene Technologies Co., Ltd., Ningbo, China). Specimens were transported, stored at 4℃, and tested for respiratory viruses within 24 h of collection.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Zhang, G., Zhang, Y., Ba, L. et al. Epidemiological changes in respiratory pathogen transmission among children with acute respiratory infections during the COVID-19 pandemic in Kunming, China. BMC Infect Dis 24, 826 (2024). https://doi.org/10.1186/s12879-024-09733-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-024-09733-y