Abstract
Background
Toxoplasma gondii (T. gondii) and Helicobacter pylori (H. pylori) are among the most prevalent foodborne parasitic and bacterial infections worldwide. However, the concurrent impact of coinfection on gastric pathology has yet to be studied in depth. The effect of coinfection generally either adds a synergetic or antagonistic impact; we aimed in the current work to assess the impact of T. gondii coinfection on the progression of H. pylori-associated gastric pathology and reporting H. pylori virulent strains. The study was conducted on 82 patients complaining of persistent gastrointestinal symptoms with failed treatment response and prone to endoscopy. They were subjected to stool examination to detect H. pylori antigen, serological screening for latent toxoplasmosis, endoscopy, histopathological examination, and molecular detection of H. pylori virulence strains in gastric biopsies. Out of the 82 patients, 62 patients were positive for H. pylori antigen in stool and 55 patients confirmed positivity by histopathology; out of them, 37 patients had isolated Vac As1 variants, 11 patients had combined Vac As1 and Cag A variants, and 7 patients had combined Vac As1, Cag A and VacAs2 variants. Patients with the combined two or three variances showed significantly deteriorated histopathological features than patients with a single Vac As1 variant (P < 0.05). Latent toxoplasmosis was positive among 35/82 patients. Combined H. pylori and Toxoplasma gondii infection had significantly marked inflammation than patients with isolated infection (P < 0.05). Conclusion: Screening for toxoplasmosis among H. pylori-infected patients is recommended as it is considered a potential risk factor for gastric inflammation severity. H. pylori gastric inflammation may be heightened by Toxoplasma coinfection.
Similar content being viewed by others
Introduction
Infectious diseases incorporate a wide range of conditions that significantly threaten the health of humans [26].. Humans are commonly infected with multiple pathogens simultaneously or consecutively, and synergistic and antagonistic pathogenic effects can subsequently impact the overall host responses and the severity of diseases [1].
Helicobacter pylori and Toxoplasma gondii are among the most prevalent bacterial and parasitic infections, respectively. H. pylori is a bacterium characterized by its spiral shape and gram-negative nature, which has a global prevalence, surpassing 50% of the global population, with greater occurrence in developing nations. It is widely recognized as the primary etiological factor responsible for chronic or atrophic gastritis, peptic ulcer, gastric lymphoma, and gastric carcinoma [31]. Considering its carcinogenic properties, the World Health Organization has classified H. pylori as a grade I carcinogen [4].
Various virulence factors contribute to the pathogenicity of this bacterium, including CagA, VacA, and others [21]. However, the clinical manifestations associated with the infection are variable [27].
The cytotoxin-associated gene A (CagA) has been recognized as a substantial carcinogen, and CagA-positive strains were associated with an elevated risk of peptic ulcer disease (PUD) or gastric cancer (GC) [18]. The Vacuolating cytotoxin A gene (Vac A) is a protein capable of inducing Vacuolation and various cellular activities and is found in all strains of H. pylori [29]. It exhibits allelic variation in three primary regions: the signal (s) region (specifically, s1a, s1b, s1c, and s2), the intermediate (i) region (i1 and i2), and the middle (m) region (m1 and m2). The diverse combination of S and M regions plays a crucial role in determining the production of cytotoxic activity and forms a mosaic gene structure [25].
Toxoplasmosis arises from the infection with T. gondii, a protozoal parasite capable of invading nucleated cells, including the human brain, eye, and muscle tissue. While human reproduction of cysts was not observed [28], it has been found that muscle and brain cysts can endure throughout the host’s lifespan [14]. The prevalence of T. gondii infection is estimated to be 30% globally [9].
The association between toxoplasmosis and other pathogens, either bacterial or viruses has been reported with different outcomes in the form of increased disease severity or protecting effect. The immunomodulatory underlying protozoal coinfection frequently hurts cellular and humoral immune responses toward co-infecting bacterial pathogens. This phenomenon leads to the promotion of bacterial persistence and ultimately results in the manifestation of more severe disease symptoms. Interestingly, the coinfection is believed to cause treatment failure, antibiotic resistance, and inefficient Vaccination programs [1].
One of the reported reciprocal impacts of Toxoplasma association with the severity of diseases was the concurrent infection with tuberculosis in an earlier study in Egypt [23]. Toxoplasma infection was also positively associated with diabetes type-1 [8]. Studies also reported that schizophrenic patients with T. gondii infection have more cognitive impairment [30]. In an earlier study, T. gondii infection produced changes in the immunological response to Helicobacter felis in experimental mice, making a resistant host susceptible to infection. For both pathogens, there was a notable increase in gastric mucosal levels of IFN-γ and IL-12, but IL-10 levels were dramatically decreased. The alterations were linked to significant stomach lining inflammation, loss of parietal cells, atrophy, and changes in cell structure.There were significant connections between the immune response to different species and indicate that these interactions may affect clinical illness (Stoicov et al., 2004).However, reports on concurrent infection with H. pylori and its impact on gastric pathology are lacking. Hence, our study aimed to study the incidence of Toxoplasma association among H. pylori-infected patients as both pathogens contribute to infection among a large sector of the human population and to document the effect of coinfection on histopathological alteration changes and to report H. pylori virulent strains effect on gastric pathology.
Methods
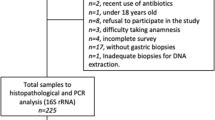
This cross-sectional study was conducted from January 2023 to June 2023 at the National Liver Institute (NLI) on one hundred patients after approval of the ethical committee under the number N. 00423/2022 from the ethical committee at the NLI. Routine stool examination was done for patients who agreed to participate in the study and complained of persistent gastrointestinal tract symptoms, while individuals with other diseases or having other concurrent intestinal parasites detected by stool examination, individuals under treatment with antibiotics or proton pump inhibitors within the past month, and individuals who were unwilling to participate were excluded. A comprehensive questionnaire was obtained from the patients, encompassing details regarding age, gender, and presenting symptoms.
H. pylori surface antigen test: A fecal specimen was obtained from each participant and subsequently preserved at a temperature of -20C for further examination. The detection of H. pylori stool antigen (HpSA) was performed using an enzyme immunoassay (EIA) method, following the guidance provided by the manufacturers. Then, it was assessed using the SD Bioline H. pylori Ag kit (Standard Diagnostics, Inc.), a commercially accessible product, following the instructions provided by the manufacturer [17].
Detection of latent toxoplasmosis
The detection of anti-Toxoplasma IgG was performed by screening serum samples utilizing commercially available ELISA kits (Abcam, USA). The optical density measurement was conducted at a wavelength of 450 nm, and after that, antibody titer for all samples was determined. According to the manufacturer’s protocol, a positive Toxoplasma IgG titer of seven was obtained.
Endoscopy
Endoscopy procedures were performed on all patients under the administration of local lignocaine anesthetic. Upper gastrointestinal (GI) endoscopy was conducted using the Olympus X Q40 instrument manufactured by Olympus Optical in Tokyo, Japan. During the endoscopic procedure, two sets of biopsy specimens were obtained from every patient’s antrum and stomach corpus. The initial batch biopsy was submitted for histological analysis and promptly immersed in a 10% formalin solution for fixation. The other specimen was placed into a buffered solution containing 10 mmol/L Tris (pH 8), 10 mmol/L ethylenediaminetetraacetic acid, and 0.5% sodium dodecyl sulfate. It was frozen at -80 °C to facilitate DNA extraction and subsequent polymerase chain reaction (PCR) experiments.
DNA extraction and polymerase chain reaction (PCR)
The DNA extraction process involved retrieving genomic DNA from stomach biopsy specimens, which was achieved by utilizing the QIAamp DNA Mini Kit (50) 51,304, manufactured by QIAGEN, USA. The extraction procedure was conducted following the directions provided by the manufacturer. A polymerase chain reaction (PCR) was conducted on the extracted DNA using primers to target the H. pylori CagA and VacA genes according to Falsafi et al. [11] protocol. The PCR experiment included a negative control sample. The identification of the bands was determined by comparing their diameters with the molecular weight markers of 100 base pairs (Thermo Scientific, (EU) Lithuania). Positive samples were deemed as such when the observable band had a comparable size to that of the positive control DNA. Primers used in the procedures are listed in Table 1.
Histopathology
Biopsy specimens were sent to the Pathology Department at the Faculty of Medicine- Menoufia University to create paraffin-embedded tissue blocks. These blocks were then used to produce 4 μm sections. Two sets of tissue slices were made for histopathological analysis. One group was stained with hematoxylin-eosin (H&E), while the other was stained with Giemsa stain (Epredia-USA; Portsmouth, NH, USA), which allowed for identifying H. pylori’s effects in the gastric mucosa. The biopsies were evaluated for the extent of inflammatory mononuclear cellular infiltrates {categorized into mild, moderate, or severe}, inflammation activity characterized by neutrophilic infiltrations {either present or absent}, glandular atrophy { present or absent}, metaplasia {present or absent }and atypia { present or absent} [7].
Results
The study included one hundred patients complaining of recurrent abdominal pain and dyspepsia. First, routine stool analysis was done for all patients with screening for H. pylori infection, which revealed that 18 out of the 100 patients had combined parasitic infections (H. pylori with either Entamoeba histolytica or Giardia lamblia) who were excluded from the study. The mean age of the remaining 82 patients was 33.68 ± 6.82 years. Most of the patients were males [68.3%]. Nearly two-thirds of the cases lived in rural areas [61%]. Secondary education and levels below were the prevalent level of education [64.6%]. The most common recorded symptoms were recurrent abdominal pain [100%] followed by dyspepsia [74.4%], then nausea [39%] and recurrent vomiting [14.6] (Table 2).
Of the 82 patients, 62 were positive for H. pylori antigen in stool, and 20 were negative. Histopathological analysis revealed that only 55 patients had H. pylori-positive gastric mucosa, and 27 had H. pylori-negative mucosa. Toxoplasma screening was done for all the patients; 35 patients had positive Toxoplasma antibodies (Fig. 1).
Diffuse redness, antral nodularity, spotty fundal hemorrhage, enlarged gastric folds, sticky tenacious mucus and xanthoma were the prominent endoscopic findings in patients with H. pylori-associated chronic gastritis. The fundic gland polyp, regular arrangement of collecting venules, raised erosion, and hematin spots were the commonest findings in patients with H. pylori-negative gastric mucosa (Table 2; Fig. 2).
According to the previous screenings, we further divided the 82 patients with abdominal pain into 3 groups; the first group included 27 patients negative for both H. pylori and Toxoplasma gondii infection, 19 (70.4%) of them were males, and 8 (29.6%) were females, their mean age was 33.74 ± 5.9 years. The second group included 24 patients with isolated H. pylori infection, which included 17 males (70.8%) and 7 females (29.2%), with a mean age of 34.5 ± 6.2 years. The third group included 20 males (64.5%) and 11 females (35.5%) positive for the two pathogens; their mean age was 33.68 ± 8 years. The gender and age distribution were comparable between the 3 groups with no statistically significant difference (P = < 0.05).
The patients who were negative for both H. pylori and Toxoplasma infection showed significantly better histopathological criteria than patients with either single or combined H. pylori infection. All the patients with negative screenings had no activity, atrophy, intestinal metaplasia, or atopy, and just 14.8% had moderate to severe inflammation (P < 0.05).
On comparing patients with isolated H. pylori versus combined H. pylori and Toxoplasma gondii infection, we found that patients with combined H. pylori and Toxoplasma gondii infection had significantly marked inflammation than patients with isolated infection (P < 0.05). At the same time, there was no statistically significant difference in the degree of activity and occurrence of atrophy, intestinal metaplasia, or atopy (P > 0.05) (Table 3; Fig. 3). There was no significant correlation on correlating the Toxoplasma antibodies titer with the chronic inflammation stage (r = 0.167, P = 0.395) and degree of activity (r = 0.103, P = 0.600).
Histopathological examination of gastric biopsy stained with Giemsa and H & E. (A) Gastric biopsy showing mucosal gastric glands containing scattered H. pylori bacilli and the intervening lamina propria showed moderate infiltration by acute and chronic inflammatory cells (H & E x400). (B) H pylori bacilli carpeting lumen of gastric glands [green arrow] (Geimsa x 400). (C) Severe activity in case of H. pylori associated chronic gastritis associated with T. gondii infection (H&E x400) (D) H. pylori -Severely active gastritis with neutrophils [red arrow] attacking mucosal associated with T. gondii infection (H & E x 400)
Further screening for the virulent strains of H. pylori was done for patients with positive immune staining. Out of the 55 patients with positive immune staining, 37 patients had isolated Vac As1 variants, 11 had combined Vac As1 and Cag A variants, and 7 had combined Vac As1, Cag A and Vac As2 variants. Patients with the combined 2 or 3 variances showed significantly deteriorated histopathological features than patients with a single Vac As1 variant (P < 0.05) (Table 4; Fig. 4).
Discussion
The global prevalent H. pylori infection is known to have the potential rise to various complications in the gastroduodenal region, including cancer development [2]. However, its successful eradication is predicted to decrease the occurrence of gastric cancer significantly (GC) [20].
The present study revealed a substantial prevalence rate of 75.6% and 67% among symptomatic patients who sought medical care at the Outpatient Clinics of the Gastroenterology unit at NLI using H. pylori antigen in stools and histopathological examination as diagnostic procedures, respectively. These findings were close to a recent study by Kishk et al. [22] and reports from Africa, which exhibited the highest prevalence of H pylori infection, with a rate of 70.1%. In contrast, Oceania demonstrated the lowest prevalence, with a rate of 24.4%. The prevalence also exhibited significant variation among different countries, ranging from a minimum of 18.9% in Switzerland to a maximum of 87.7% in Nigeria [19].
The variations in infection rates were attributed to differences in research methodology, participant diversity and inclusion criteria, number of participants, and approaches used for detecting H. pylori [15].
In the present study, the assessment of infection with H. pylori was conducted using different diagnostic procedures for symptomatic patients. Our study revealed false positive results detected by the SAT exhibited and were negative in gastric biopsies. These results contrasted with a recent study conducted in Uganda, which emphasized the exceptional role of the SAT in detecting H. pylori in regions with a high prevalence of the disease Owot et al. [24] and agreed with the results of Zubair et al. [33] who reported the limited sensitivity and diagnostic accuracy of the HPSA test.
The study found that several socio-demographic variables were associated with H. pylori infection. These variables included increasing age, residing in rural areas, and lower educational level, which agreed with previously studied risk factors for infection in earlier studies in Egypt and African countries [3, 15]. Abdominal pain and dyspepsia were the presenting symptoms of most cases in the current work, which agreed with many researchers as they contributed to many cases of infection with H. pylori [15, 22].
In our study, screening for the virulent strains of H. pylori was done for patients with positive immune staining; 37/55 (67%) patients had isolated Vac As1 variant, 11/55 (20%) patients had combined Vac As1 and Cag A variants and 7 /55 ( 12.7%) patients had combined Vac As1, Cag A and Vac As2 variants. Similar results were obtained by Kishk et al. [22], who showed that all strains with the CagA gene were VacA gene positive.
Concerning the genotypes of CagA and VacA, it was observed that the VacA s1 allele, which was the most prevalent, agreed with a prior investigation conducted on patients from Cuba; the presence of the VacA gene was observed in 61.6% of the H. pylori strains examined, with this gene being identified as the predominant virulence factor in most of the strains [13]. Nevertheless, the findings of this study opposed the previous research conducted by Kishk et al. [22] [12], where they observed that the VacA+/CagA − genotype s1 had the lowest prevalence. Conversely, a separate study conducted in Algeria revealed the presence of the CagA gene in 58% of the examined patients [5].
Interestingly, CagA + was not found in our study as a single genotype. It was rather linked to VacA s1 in (11/55) or to Vac As2 alle in (7/55) patients, and this was consistent with [22]. Additionally, the lower percentage of the VacA s2 genotype is considered a less virulent form as compared with the acutely damaging VacA s1, as stated by Falsafi et al. [12]. This study investigated the association between the VacA and CagA genotypes and clinical outcomes, as endoscopic results showed. Patients with the combined 2 or 3 variances showed significantly deteriorated histopathological features than patients with a single Vac As1 variant (P < 0.05).
The significant impact of association of H. pylori and T. gondii on gastric inflammation severity was reported in this study, which is documented for the first time based on research on different databases.
The potential correlation between H. pylori and T. gondii was investigated in the context of gastritis and the development of peptic ulcers. The observed correlation can be attributed to the fecal-oral route, a frequently seen infection pathway for both pathogens. The elevated rates of H. pylori discovery in feline fecal samples have prompted consideration of potential zoonotic transmission of these infections [6, 16].
In earlier studies, the co-infection of H. pylori with either Ascaris lumbricoides or T. gondii resulted in modified H. pylori gastritis in mouse experimental models [10]. The present study’s findings indicate that among a cohort of 31 individuals who were simultaneously infected with both H. pylori and T. gondii, a substantial majority (80.6%) experienced gastritis of moderate to severe intensity. The results were in line with Ghazy et al. [16].
This report presents novel findings regarding the impact of toxoplasmosis on the severity of gastritis in humans. Specifically, it is the first documented record to investigate and compare patients with isolated H. pylori infection and those with combined H. pylori and T. gondii infection. The results indicated that patients with combined infections exhibited significantly more advanced inflammation stages than patients with isolated infections (P < 0.05). However, when examining the relationship between the titer of Toxoplasma antibodies and the stage of chronic inflammation (r = 0.167, P = 0.395) as well as the degree of activity (r = 0.103, P = 0.600), no statistically significant association was seen for either variable. The findings of this study were incongruent with the research conducted by Ghazy et al. [16] since their study demonstrated a positive correlation between the severity of gastritis cases and elevated levels of serum anti-Toxoplasma IgG.
Conclusion and recommendations
Prevalence of chronic T. gondii infection in individuals with concomitant H. pylori infection. The results revealed an elevated prevalence of latent Toxoplasma infection among patients infected with H. pylori. Furthermore, a notable association was observed about heightened gastrointestinal severity. Furthermore, the predominant genotype observed in our examined population was Vac As1. However, there were notable variations in genotype combinations associated with significantly more severe histopathological manifestations than individuals with a single Vac As1 variant (P < 0.05). Advanced molecular techniques have emerged as reliable means for identifying virulent strains of H. pylori due to their enhanced sensitivity and specificity. Future studies are required to examine the mechanism lying behind this association.
Data availability
The datasets present in the current investigation can be upon a reasonable request.Contact prof. Marwa Ahmed Gouda Email:
Abbreviations
- T.gondii:
-
Toxoplasma gondii
- H. pylori :
-
Helicobacter pylori
- CagA:
-
The cytotoxin-associated gene A
- PUD:
-
peptic ulcer disease
- GC:
-
gastric cancer
- VacA:
-
Vacuolatingcytotoxin A gene
- HpSA:
-
H. pylori stool antigen
- EIA:
-
enzyme immunoassay
References
Akoolo L, Rocha SC, Parveen N. (2022). Protozoan co-infections and parasite influence on the efficacy of Vaccines against bacterial and viral pathogens. Front Microbiol, 4723.
Alsulaimany FAS, Awan ZA, Almohamady AM, Koumu MI, Yaghmoor BE, Elhady SS, Elfaky MA. Prevalence of Helicobacter pylori infection and diagnostic methods in the Middle East and North Africa Region. Med (Kaunas Lithuania). 2020;56(4). https://doi.org/10.3390/medicina56040169.
Aminde JA, Dedino GA, Ngwasiri CA, Ombaku KS, Makon M, C. A., Aminde LN. Helicobacter pylori infection among patients presenting with dyspepsia at a primary care setting in Cameroon: seroprevalence, five-year trend and predictors. BMC Infect Dis. 2019;19(1):30. https://doi.org/10.1186/s12879-019-3677-0.
Ansari S, Yamaoka Y. Helicobacter pylori virulence factors exploiting gastric colonization and its pathogenicity. Toxins. 2019;11(11). https://doi.org/10.3390/toxins11110677.
Bachir M, Allem R, Tifrit A, Medjekane M, Drici AE-M, Diaf M, Douidi KT. Primary antibiotic resistance and its relationship with CagA and VacA genes in Helicobacter pylori isolates from Algerian patients. Brazilian J Microbiology: [Publication Brazilian Soc Microbiology]. 2018;49(3):544–51. https://doi.org/10.1016/j.bjm.2017.11.003.
Bui D, Brown HE, Harris RB, Oren E. Serologic evidence for fecal-oral transmission of Helicobacter pylori. Am J Trop Med Hyg. 2016;94(1):82–8. https://doi.org/10.4269/ajtmh.15-0297.
Cardos AI, Maghiar A, Zaha DC, Pop O, Fritea L, Groza M, F., Cavalu S. Evolution of diagnostic methods for Helicobacter pylori infections: from traditional tests to High Technology, Advanced sensitivity and discrimination tools. Diagnostics (Basel Switzerland). 2022;12(2). https://doi.org/10.3390/diagnostics12020508.
Catchpole A, Zabriskie BN, Bassett P, Embley B, White D, Gale SD, Hedges D. Association between Toxoplasma Gondii Infection and Type-1 diabetes Mellitus: a systematic review and Meta-analysis. Int J Environ Res Public Health. 2023;20(5). https://doi.org/10.3390/ijerph20054436.
Dubey JP, Bealty CP. Toxoplasmosis of animals and humans. Boca Raton, FL: CRC; 2010.
Ek C, Whary MT, Ihrig M, Bravo LE, Correa P, Fox JG. Serologic evidence that ascaris and Toxoplasma infections impact inflammatory responses to Helicobacter pylori in Colombians. Helicobacter. 2012;17(2):107–15. https://doi.org/10.1111/j.1523-5378.2011.00916.x.
Falsafi T, Favaedi R, Mahjoub F, Najafi M. Application of stool-PCR test for diagnosis of Helicobacter pylori infection in children. World J Gastroenterol. 2009;15(4):484–8. https://doi.org/10.3748/wjg.15.484.
Falsafi T, Khani A, Mahjoub F, Asgarani E, Sotoudeh N. Analysis of VacA/CagA genotypes/status in Helicobacter pylori isolates from Iranian children and their association with clinical outcome. Turk J Med Sci. 2015;45(1):170–7. https://doi.org/10.3906/sag-1311-2.
Feliciano O, Gutierrez O, Valdés L, Fragoso T, Calderin AM, Valdes AE, Llanes R. (2015). Prevalence of Helicobacter pylori VacA, CagA, and iceA Genotypes in Cuban Patients with Upper Gastrointestinal Diseases. BioMed Research International, 2015, 753710. https://doi.org/10.1155/2015/753710.
Flegr J, Prandota J, Sovičková M, Israili ZH. (2014). Toxoplasmosis–a global threat. Correlation of latent toxoplasmosis with specific disease burden in a set of 88 countries. PLoS ONE, 9(3), e90203.
Galal YS, Ghobrial CM, Labib JR, Abou-Zekri ME. Helicobacter pylori among symptomatic Egyptian children: prevalence, risk factors, and effect on growth. J Egypt Public Health Assoc. 2019;94(1):17. https://doi.org/10.1186/s42506-019-0017-6.
Ghazy A, Elawamy W, Haydara T, Taha A. The impact of H. Pylori and/or T. gondii infection on recurrence of gastritis and gastric ulcer. Parasitologists United J. 2021;14(3):286–92.
Ghorbani F, Gheisari E, Dehkordi FS. Genotyping of VacA alleles of Helicobacter pylori strains recovered from some Iranian food items. Trop J Pharm Res. 2016;15(8):1631–6.
Hatakeyama M. Anthropological and clinical implications for the structural diversity of the Helicobacter pylori CagA oncoprotein. Cancer Sci. 2011;102(1):36–43. https://doi.org/10.1111/j.1349-7006.2010.01743.x.
Hooi JKY, Lai WY, Ng WK, Suen MMY, Underwood FE, Tanyingoh D, Malfertheiner P, Graham DY, Wong VWS, Wu JCY, Chan FKL, Sung JJY, Kaplan GG, Ng SC. Global prevalence of Helicobacter pylori infection: systematic review and Meta-analysis. Gastroenterology. 2017;153(2):420–9. https://doi.org/10.1053/j.gastro.2017.04.022.
Hu Y, Zhu Y, Lu N-H. The management of Helicobacter pylori infection and prevention and control of gastric cancer in China. Front Cell Infect Microbiol. 2022;12:1049279. https://doi.org/10.3389/fcimb.2022.1049279.
Kao C-Y, Sheu B-S, Wu J-J. Helicobacter pylori infection: an overview of bacterial virulence factors and pathogenesis. Biomedical J. 2016;39(1):14–23. https://doi.org/10.1016/j.bj.2015.06.002.
Kishk RM, Soliman NM, Anani MM, Nemr N, Salem A, Attia F, Allithy ANA, Fouad M. (2021). Genotyping of Helicobacter pylori Virulence Genes CagA and VacA: Regional and National Study. International Journal of Microbiology, 2021, 5540560. https://doi.org/10.1155/2021/5540560.
Mashaly M, Nabih N, Fawzy IM, El Henawy AA. Tuberculosis/toxoplasmosis co-infection in Egyptian patients: a reciprocal impact. Asian Pac J Trop Med. 2017;10(3):315–9.
Owot JC, Tuhumwire C, Tumuhimbise C, Tusiime F, Emmanuel B, Lumori BAE, Okello S. Diagnostic performance of fecal Helicobacter pylori antigen test in Uganda. BMC Gastroenterol. 2022;22(1):518. https://doi.org/10.1186/s12876-022-02551-z.
Rhead JL, Letley DP, Mohammadi M, Hussein N, Mohagheghi MA, Hosseini E, M., Atherton JC. A new Helicobacter pylori Vacuolating cytotoxin determinant, the intermediate region, is associated with gastric cancer. Gastroenterology. 2007;133(3):926–36. https://doi.org/10.1053/j.gastro.2007.06.056.
Shen S-S, Qu X-Y, Zhang W-Z, Li J, Lv Z-Y. Infection against infection: parasite antagonism against parasites, viruses and bacteria. Infect Dis Poverty. 2019;8(1):49. https://doi.org/10.1186/s40249-019-0560-6.
Šterbenc A, Jarc E, Poljak M, Homan M. Helicobacter pylori virulence genes. World J Gastroenterol. 2019;25(33):4870–84. https://doi.org/10.3748/wjg.v25.i33.4870.
Torrey EF, Yolken RH. Toxoplasma oocysts as a public health problem. Trends Parasitol. 2013;29(8):380–4.
Utsch C, Haas R. VacA’s induction of VacA-Containing Vacuoles (VCVs) and their immunomodulatory activities on human T cells. Toxins. 2016;8(6). https://doi.org/10.3390/toxins8060190.
Veleva I, Stoychev K, Stoimenova-Popova M, Stoyanov L, Mineva-Dimitrova E, Angelov I. Toxoplasma Gondii seropositivity and cognitive function in adults with schizophrenia. Schizophrenia Res Cognition. 2022;30:100269. https://doi.org/10.1016/j.scog.2022.100269.
Xu W, Xu L, Xu C. Relationship between Helicobacter pylori infection and gastrointestinal microecology. Front Cell Infect Microbiol. 2022;12:938608. https://doi.org/10.3389/fcimb.2022.938608.
Xue Z, Yang H, Su D, Song X, Deng X, Yu C, Sun C, He L, You Y, Gong Y, Fan D, Sun L, Han X, Fan R, Zhang M, Yan X, Qian J, Zhang J. Geographic distribution of the CagA, VacA, iceA, oipA and dupA genes of Helicobacter pylori strains isolated in China. Gut Pathogens. 2021;13(1):39. https://doi.org/10.1186/s13099-021-00434-4.
Zubair M, Nawaid MA, Afridi NK, Baig B, Hanif M, Mahmoud TM, Gabalunos HS. Comparison of stool antigen test with histopathology of endoscopic gastric biopsies for detection for helicobacter pylori; a hospital-based study. Pakistan Armed Forces Med J. 2022;72:S268.
Acknowledgements
We would like to express our sincere gratitude to everyone who took part in this study. We truly appreciate everyone who agreed to help us and offered some of their necessary time.
Funding
The study paper was written, edited, and published without outside funding.
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Author information
Authors and Affiliations
Contributions
The study’s commencement and conception involved the collaborative input of all authors. The materials were generated, and the data was collected and assessed by M.A.G., S.A.S., S.A., A.E., A.A.S., R.G.M., A.S., and A.E. The manuscript’s first version was authored by M. A.G., S. A.S., and R.G.M. with the subsequent writers providing their input on earlier iterations. The final version of the work was comprehensively evaluated by all authors and received universal endorsement.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This experiment was approved by the National Liver Disease Institute’s Research Ethics Committee (NLI IRB procedure N. 00423/2022). The Declaration of Helsinki’s essential principles and practices were followed throughout the research.
Consent to participate
Every participant gave their written authorization after being informed of the study’s objectives and any potential negative side effects.
Consent for publication
Not Applicable.
Competing interests
This study's research, writing, and publication were all done without any actual or prospective conflicts of interest.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Gouda, M.A., Saied, S.A., Edrees, A. et al. Effect of concurrent infection of Helicobacter pylori with Toxoplasma gondii infection on gastric pathology. BMC Infect Dis 24, 408 (2024). https://doi.org/10.1186/s12879-024-09270-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-024-09270-8