Abstract
Background
This real-world study assessed the epidemiology and clinical complications of Clostridioides difficile infections (CDIs) and recurrences (rCDIs) in hospital and community settings in Germany from 2015 − 2019.
Methods
An observational retrospective cohort study was conducted among adult patients diagnosed with CDI in hospital and community settings using statutory health insurance claims data from the BKK database. A cross-sectional approach was used to estimate the annual incidence rate of CDI and rCDI episodes per 100,000 insurants. Patients’ demographic and clinical characteristics were described at the time of first CDI episode. Kaplan-Meier method was used to estimate the time to rCDIs and time to complications (colonic perforation, colectomy, loop ileostomy, toxic megacolon, ulcerative colitis, peritonitis, and sepsis). A Cox model was used to assess the risk of developing complications, with the number of rCDIs as a time-dependent covariate.
Results
A total of 15,402 CDI episodes were recorded among 11,884 patients. The overall incidence of CDI episodes declined by 38% from 2015 to 2019. Most patients (77%) were aged ≥ 65 years. Around 19% of CDI patients experienced at least one rCDI. The median time between index CDI episode to a rCDI was 20 days. The most frequent complication within 12-months of follow-up after the index CDI episode was sepsis (7.57%), followed by colectomy (3.20%). The rate of complications increased with the number of rCDIs. The risk of any complication increased by 31% with each subsequent rCDI (adjusted hazard ratio [HR]: 1.31, 95% confidence interval: 1.17;1.46).
Conclusions
CDI remains a public health concern in Germany despite a decline in the incidence over recent years. A substantial proportion of CDI patients experience rCDIs, which increase the risk of severe clinical complications. The results highlight an increasing need of improved therapeutic management of CDI, particularly efforts to prevent rCDI.
Similar content being viewed by others
Background
Clostridioides difficile is a leading cause of healthcare-associated infectious diarrhoea [1, 2], with 20−30% of C. difficile infections (CDIs) being acquired in community settings [3]. CDI symptoms range from mild diarrhoea to severe complications, including colitis, toxic megacolon, colonic perforation, and sepsis [4, 5]. Around a quarter of CDI patients experience a recurrence (rCDI), of which 40–65% experience multiple rCDIs [6]. Frequent rCDIs lead to repeated hospitalisations, reduced health-related quality of life [7,8,9], and risk of death [10]. Common risk factors to CDI and rCDI include antibiotic use, advanced age, and admission to healthcare facilities [11]. CDI is routinely treated with antibiotics, including vancomycin and fidaxomicin (metronidazole may also be used only if vancomycin and fidaxomicin are not available), while surgical intervention and non-antimicrobial management (via faecal microbiota transplant) may be required for severe or unresponsive patients with multiple rCDIs [12, 13].
The European Centre for Disease Prevention and Control (ECDC) surveillance report for 2016–2017 reported a crude incidence density of 3.48 cases per 10,000 patient-days in acute-care hospitals [14]. Recurrences were reported in 6.4% of cases and these were almost twice as likely to develop complications when compared with non-recurrent cases [14]. A systematic review and meta-analysis of studies and surveillance reports between 2005 and 2015 estimated a median overall incidence rate (IR) of 4.00 CDI cases per 10,000 patient-days [15]. Among European countries, one of the highest median overall incidences was reported in Germany (7.00 CDI cases per 10,000 patient-days) [15]. Recent studies on the burden of hospitalised CDI in Germany over the last decade have shown a decline in the incidence of CDI [16, 17]. It is however expected that the burden of CDI is likely underestimated as the surveillance system in Germany (as in other countries) is based on hospitalised cases only [17].
The present study aims to generate real-world evidence on the epidemiology and clinical complications of CDI and rCDI both in hospital and community settings in Germany using claims data between 2015 and 2019.
Materials and methods
Study design and data source
This observational retrospective study used claims data from BKK insurants (i.e., members of Betriebskrankenkassen, company-based sickness funds), part of the German Statutory Health Insurance (SHI) scheme database covering about 90% of the German population (i.e., 73 million people). The SHI database includes primary and specialty care data linked to hospital data and covers registrations, out- and in-patient care, drug prescriptions in community settings, and other services. The BKK database contains anonymised data of 5 million insurants and is representative of the entire SHI-insured population in terms of age, sex, prescriptions, and hospital diagnoses.
In this study, a cross-sectional approach spanning a five-year period (January 1, 2015 to December 31, 2019) was used to describe the annual incidence of CDI episodes and patient characteristics. A pre-index period of 12 months was used to characterise patients at baseline, namely on comorbidities, comedications and other potential risk factors. The year 2020 was not considered in the study period due to the potential impact of the COVID-19 pandemic on hospitalisations and ambulatory care as well as on the timely impact on data to be retrieved from BKK.
A longitudinal approach was performed to estimate the time from index CDI to rCDI, time from an rCDI to subsequent rCDI, and to assess the rate and risk of clinical complications at 12 months of follow-up. Patients were censored at the time of death, loss to follow-up, or at the end of the study period (December 31, 2019), whichever occurred first.
Study population
Adult patients (≥ 18 years) diagnosed with CDI (International Classification of Diseases version 10 [ICD-10] code: A04.7) in a hospital or community setting between 2015 and 2019 and with a valid database record at least 12 months before the index date were included. Patients experiencing a CDI episode within 60 days prior to index episode were excluded from the study.
In community settings, diagnoses were only available on quarterly basis. To rule out potential false positives, patients with ≥ 1 gastrointestinal condition(s) (ICD-10 codes A09, K52, A48, K50, K57) during the same or previous quarter of CDI diagnoses and patients with no record of biological tests for identification of bacterial toxin A or B, nor prescriptions of CDI-related antibiotics within the quarter of the diagnosis were excluded. A sensitivity analysis was conducted without excluding these patients to estimate the upper range of CDI incidence.
Definitions of CDI, rCDI episodes and new occurrence of CDI
The first CDI episode reported during the study period was designated as the index episode. Index episodes were classified according to the setting of treatment (hospital [hospitalised CDI] or community setting [community-treated CDI]) and setting of infection (healthcare-, community-associated CDI or unknown) (Fig. S1).
A CDI episode occurring within 60 days from the first CDI episode was considered a rCDI. The same criterion was applied to a subsequent CDI episode (i.e., second and third rCDI) occurring within 60 days of the previous rCDI. rCDI episodes in hospital settings were identified using diagnostic codes. In community settings, these were identified using two consecutive prescriptions of antibiotics indicated for CDI (i.e., non-topical metronidazole, or vancomycin, or fidaxomicin) where the second prescription was considered as the rCDI start date. In case of the same antibiotic, the two prescriptions should have been prescribed within a 30–60-day interval.
A CDI episode occurring beyond 60 days from the previous episode (index or rCDI) was considered a new CDI occurrence. Only the first occurrence of a new CDI was considered in the study. New CDI episodes were identified either by an ICD-10 diagnosis, or a second prescription of CDI-related antibiotics, if occurring beyond 60 days from the previous episode.
For hospitalised CDI, hospital entry dates were considered the start dates of episodes, unless CDI was reported as a secondary diagnosis and the hospital stay was > 14 days, in which the episode start date was approximated either by the median length of hospital stays with a reported CDI diagnosis or discharge date, whichever occurred first. For community-treated CDI episodes, prescriptions of CDI-related antibiotics were used to approximate the episode start date. Records of biological tests ordered for identification of bacterial toxin A or B were used if prescriptions were missing.
Data analysis
Analyses were conducted using SAS® version 9.4 and graphs were generated using R software version 4.0.5. Absolute numbers and percentages were computed for categorical variables while descriptive statistics (mean, standard deviation [SD], median, 25th and 75th percentiles, and minimum and maximum) were displayed for quantitative variables. A significance level of 5% was considered (P < 0.05 for two-tailed test) for all statistical comparisons.
Annual incidence of CDI episodes was calculated per 100,000 inhabitants using the respective adult population of BKK insurants per year as the denominator. Charlson Comorbidity Index (CCI) comorbidities were identified using algorithms (Table S1) and the age-adjusted CCI score was categorized into 0–6, 7–10 or ≥ 11 points [18].
Longitudinal analyses were restricted to the subpopulation of patients diagnosed before December 31, 2018 without any CDI episode within 6 months prior to the index CDI episode. Time in days between index CDI episode and first rCDI, and from the previous rCDI to the subsequent episode was described using the Kaplan-Meier (KM) estimator (median and interquartile range), and survival curves with corresponding 95% confidence intervals (95% CIs). The rate of first complication was calculated at 3, 6 and 12-months of follow-up, overall (i.e., for ‘any complication’) and for each complication. The KM method was used to estimate the cumulative incidence of complications over follow-up. The risk of developing any complication at 12-month follow-up was estimated using Cox regression models where the number of rCDIs was treated as a time-dependent covariate, adjusting for potential confounders. Covariates that met the significance level of < 0.05 were added into the multivariate model using backward selection.
Results
Study participants
Following the screening of 12,330 patients with ≥ 1 CDI diagnosis recorded between January 1, 2015 and December 31, 2019, a total of 11,884 (96.4%) patients (Table S2) were included in the study. At the index CDI episode, most patients (88.3%; n = 10,491) were treated in hospital settings.
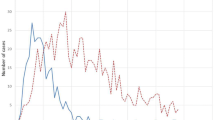
Incidence and incidence rate of index CDI, rCDI, and new CDI episodes
A total of 15,402 CDI episodes (of any type) were observed in the cross-sectional cohort (Table 1). A decline of approximately 38% in the IR of CDI episodes (of any type) was observed between 2015 and 2019 (123.88 and 77.06 episodes per 100,000 insurants, respectively). A similar decrease was observed for index CDI (from 96.56 to 59.79 per 100,000 insurants) and first rCDI (from 17.8 to 10.61 per 100,000 insurants) episodes.
When accounting for CDI patients in community settings that might be false positives (sensitivity analysis), the opposite was observed, with the total number of CDI episodes increasing from 15,402 to 19,575 over the study period. However, a similar IR decline of approximately 36% was observed from 156.22 to 100.13 CDI episodes per 100,000 insurants in 2015 and 2019, respectively.
Table 2 characterises patients according to the number of rCDIs (1, 2, ≥ 3) over the study period. Overall, 17.86% (n = 2,122) patients experienced ≥ 1 rCDI; 13.54% (n = 1,609) 1 rCDI, 3.03% (n = 360) 2 rCDIs, and 1.29% (n = 153) ≥ 3 rCDIs. Among those with ≥ 1 rCDI (n = 2,122 patients), 24.18% (n = 513) experienced a second rCDI, of whom 29.82% (n = 153) had at least a third rCDI (data not shown).
Demographic and clinical characteristics of CDI and rCDI patients
Table 3 presents patients’ demographic and clinical characteristics. The mean age of CDI patients was 73.23 years (median [Q1; Q3]: 78 [66.00; 84.00]). Most CDI patients were aged ≥ 65 years (76.79%; n = 9,126). This proportion increased to 81.86% (n = 1,737) among patients with ≥ 1 rCDI. A slightly higher proportion of women (52.29%) was observed, which increased to 57.52% in patients with ≥ 3 rCDIs. The median age-adjusted CCI registered at index date ranged from 8 to 9 across the different subgroups and was higher among patients with two or more rCDIs. Most patients (92.69%, n = 11,015) had pre-existing comorbidities, with chronic kidney disease and renal failure (49.35%, n = 5,865), heart failure (43.70%, n = 5,193), and ischaemic heart disease (37.62%, n = 4,471) being the most reported. The proportion of patients with comorbidities increased with the number of rCDIs. During the pre-index period, a high proportion of CDI patients were treated with antibiotics (48.76%; n = 5,795) and PPIs (58.74%; n = 6,981). A gastrointestinal procedure was recorded among 11.91% (n = 1,415) of patients.
Of the 56.32% (n = 6,693) of patients with a known setting of infection, 67.52% (n = 4,519) were classified as having a community-associated index CDI episode and 32.48% (n = 2,174) as having a healthcare-associated index CDI episode. The setting of infection was unknown in 43.68% of patients (n = 5,191).
Time between CDI and rCDI episodes
Table 4 shows the time from the index CDI episode to the first rCDI, and the time from the previous rCDI to the next rCDI. In the subset of patients for longitudinal analysis (n = 9,977), 18.06% (n = 1,802) experienced ≥ 1 rCDI event after a median time of 20 days from the index CDI episode. The time to the subsequent recurrent event was consistent until the fourth episode of rCDI, ranging between a median of 20 and 22 days (Table 4, Fig. S2).
Rate of complications among CDI and rCDI patients
Table 5 presents the rates of complications among the subpopulation of patients for longitudinal analysis (n = 9,977) at 3-, 6- and 12-months of follow-up. The most common complication at 12-months of follow-up was sepsis (7.57%, n = 755), followed by colectomy (3.20%, n = 319), and ulcerative colitis (1.13%, n = 113). All other complications were observed in < 1% of patients. The rate of complications increased over the follow-up time. Among CDI patients, 8.40% (n = 838) had a complication (any type) at 3-months of follow-up, which increased to 10.34% (n = 1,032) and 12.43% (n = 1,240) at 6- and 12-months of follow-up, respectively. The rate of complications was higher among patients with rCDIs and increased at each subsequent episode (any complication at 12-months of follow-up observed in 14.75%, 13.78%, and 23.13% of patients with 1, 2 and ≥ 3 rCDIs, respectively).
The risk of developing any complication increased by 1.31 times with each subsequent rCDI (adjusted hazard ratio [HR]: 1.31, 95% CI: 1.17; 1.46) (Table 6). Patients treated in hospital settings had two times higher risk of developing complications in comparison to those treated in community settings (adjusted HR: 2.18, 95% CI: 1.72; 2.77). Males, patients with pre-index comorbidities, with pre-index medications, gastrointestinal procedures, hospitalisations, and outpatient consultations, and intensive care unit (ICU) admissions were also at higher risk of complications.
Discussion
A total of 15,402 CDI episodes were captured in 11,884 patients between 2015 and 2019. A decline in the annual IR of CDI and rCDI of approximately 38% was observed during the study period from 124 to 77 episodes per 100,000 insurants. Nearly a fifth of patients experienced a rCDI and the proportion of patients with a subsequent episode increased at each episode. Among patients with at least 1 rCDI, 24% experienced a second rCDI, of whom 30% experienced ≥ 3 rCDIs. Around 12% of CDI patients developed clinical complications within 12 months of follow-up, with sepsis being the most frequently observed. Complications were more common in patients with multiple rCDIs, being observed in 23% of patients with ≥ 3 rCDIs. The risk of any complication at 12-month of follow-up increased by 31% with each rCDI. To ensure specificity of CDI episodes and avoid false positives, patients with a diagnosis recorded in community settings with concurrent gastrointestinal conditions that could have been treated with antibiotics with a CDI indication were excluded from the main analysis, along with patients with no record of relevant antibiotic prescriptions or biological tests. When these patients were included in the sensitivity analysis, an additional 4,173 (27%) CDI episodes were added.
Overall, the results are aligned with recent data on the burden of hospitalised CDI from publicly available sources in Germany between 2010 and 2019, which has shown a steady decline from 2015 onwards, with 81 cases per 100,000 population observed in 2019 [17]. A study on hospital coding practices for CDI in Germany showed a decline of 52% in the number of cases recorded as a primary diagnosis (i.e., CDI as the reason for admission) and 49% of cases recorded as a secondary diagnosis (i.e., occurrence during the hospital stay or pre-existing condition), from 2015 to 2019 [16]. Several factors are likely to have contributed to the downward trend of CDI incidence in Germany over the study period, including hospital hygiene campaigns, implementation of antibiotic stewardship programs, among others.
Similar trends have been reported in other countries. In the United States (US), a decline from 149 to 121 cases per 100,000 persons was reported between 2015 and 2019 [19,20,21,22,23,24]. This has been attributed to a decrease in healthcare-associated CDI cases (as community-associated CDI remained stable) and explained by more judicious antibiotic use, especially fluoroquinolones [19,20,21,22,23,24,25]. Similar trends were also observed in France and Canada [26, 27]. However, a recent systematic review on the epidemiology of CDI and rCDI in 11 countries revealed no clear trends for incidence with time, with variations across countries [11]. Furthermore, the ECDC has emphasised the lack of a standardised CDI surveillance, which limits the identification of epidemiological changes in the region and consequently hinders CDI prevention and control [28].
In line with prior studies [2, 11, 29,30,31,32], CDI and rCDI were more frequently observed among older patients and in those with pre-existing comorbidities, such as chronic kidney disease, among others. Several factors contribute to the increased susceptibility to CDI and rCDI among the elderly, including immunosenescence, age-related alterations in the gut microbiome, overall poor health, increased hospitalisations/nursing home stays, and frequent use of antibiotics and PPIs [33]. Several studies established the role of antibiotics, PPIs, and gastrointestinal procedures as risk factors for CDI [3, 34, 35]. In the current study, a high proportion of CDI patients were prescribed antibiotics (49%) and PPIs (59%) during the pre-index period, and around 12% patients underwent a gastrointestinal procedure. However, the use of antibiotics is likely underestimated since hospital-dispensed treatments are not recorded in the BKK database. Like other studies, there was a higher proportion of female patients in our study [5, 36,37,38]. So far, no association has however been found between gender and susceptibility to CDI.
Almost 90% of CDI patients were treated in hospital settings, likely reflecting the management of the disease in Germany as well as patient characteristics such as older age, health status, or severity of disease. The substantially low proportion of patients treated in community settings could be partially explained by the exclusion of patients with concomitant gastrointestinal conditions, but misdiagnosis and misclassification can’t be ruled out either. Aligned with a previous study in the country, around 18% of patients experienced a recurrence a median 20 days after the index CDI episode. In that study, the risk of developing a second and third episode increased to 28.4% and 30.2%, respectively [30]. A 25% probability of developing a first rCDI after an initial infection has also been reported [37]. A more recent study found lower rates of rCDI rates probably due to the use of sub-codes to specify recurrences, which were not applied in this study.
Sepsis and colectomy were the most frequently recorded clinical complications with complications being higher in those with recurrences. Sepsis occurred in 7.6% of CDI patients vs. 17.16% in patients with ≥ 3 rCDIs. A real-world study in the US reported a similar pattern but with even higher rates of complications. Sepsis was observed in 16.5% of CDI patients without rCDIs at 12-months of follow-up, increasing to 27.3%, 33.1%, and 43.3% in patients with 1, 2, and 3 + rCDIs, respectively. Likewise, subtotal colectomy or diverting loop ileostomy occurred in 4.6% of patients with a first CDI episode, increasing with the number of recurrences to 7.3%. 8.9%, and 10.5% of patients with 1, 2, and 3 + rCDIs, respectively [36].
When estimating the risk of any complication at 12-months, the current study showed an increased risk of 31% with each subsequent rCDI. Complications were twice as likely to occur among patients treated in hospitals during the index episode compared to those treated in community settings, suggesting a more severe and frail patient population. Although the outcome of interest included any complication, the results were likely driven by sepsis, the most frequently reported complication. However, it should be noted that whether there is a causative relationship between CDI or rCDI and the incidence of complications remains unclear. Furthermore, complications may not necessarily develop after CDI diagnosis but could also be the relapse or exacerbation of previous complications.
The use of claims data from the German BKK database proved to be useful in capturing CDI and rCDI cases, and to provide further insights on the disease at the community level, which is not captured in the traditional hospital-based surveillance system. However, despite the development of an algorithm to ascertain the setting of infection, 43% of CDI episodes were classified as unknown, which limited the interpretation of the results. Like other studies relying on existing data, the primary intention of collecting claims data is not research, and some data may not be recorded or may be misclassified or miscoded, leading to bias. Further, diagnostic data are available in the BKK database only on a quarterly basis. Thus, patients with other gastrointestinal conditions and those who were not prescribed any antibiotic indicated for CDI, nor a test for identification of bacterial toxin A or B were excluded. This methodological choice probably led to an underestimation of the cases in the country.
Conclusions
This real-world study provided an overview on the epidemiology and clinical complications of CDI and rCDI in Germany. Frequent rCDIs represent a particular concern, being associated with an increased risk of clinical complications. The findings demonstrate not only the urgent need to break the cycle of CDI and rCDI through the development of effective and innovative therapies but also to improve current surveillance systems to include community-treated cases.
Data availability
The data that support the findings of this study are available from statutory sickness funds but restrictions apply to the availability of these data, which were used under license for the current study, and are not publicly available. Data are available from the authors upon reasonable request, and with permission of data-providing sickness funds.
Abbreviations
- BKK:
-
Betriebskrankenkassen
- CCI:
-
Charlson Comorbidity Index
- CDI:
-
Clostridioides difficile infection
- CI:
-
Confidence interval
- ECDC:
-
European Centre for Disease Prevention and Control
- ICD-10:
-
International Classification of Diseases version 10
- IR:
-
Incidence rate
- KM:
-
Kaplan-Meier
- rCDI:
-
Recurrent Clostridioides difficile infection
- SD:
-
Standard deviation
- SHI:
-
Statutory Health Insurance
- HR:
-
Hazard ratio
- ICU:
-
Intensive care unit
- PPI:
-
Proton-pump inhibitor
- US:
-
United States
References
Magill SS, Edwards JR, Bamberg W, Beldavs ZG, Dumyati G, Kainer MA, et al. Multistate point-prevalence survey of health care-associated infections. N Engl J Med. 2014;370(13):1198–208.
Czepiel J, Drozdz M, Pituch H, Kuijper EJ, Perucki W, Mielimonka A, et al. Clostridium difficile infection: review. Eur J Clin Microbiol Infect Dis. 2019;38(7):1211–21.
Eze P, Balsells E, Kyaw MH, Nair H. Risk factors for Clostridium difficile infections - an overview of the evidence base and challenges in data synthesis. J Glob Health. 2017;7(1):010417.
Schaffler H, Breitruck A. Clostridium difficile - from colonization to infection. Front Microbiol. 2018;9:646.
Czepiel J, Krutova M, Mizrahi A, Khanafer N, Enoch DA, Patyi M, et al. Mortality following Clostridioides difficile infection in Europe: a retrospective Multicenter Case-Control Study. Antibiot (Basel). 2021;10(3):299.
Smits WK, Lyras D, Lacy DB, Wilcox MH, Kuijper EJ. Clostridium difficile infection. Nat Rev Dis Primers. 2016;2:16020.
Lurienne L, Bandinelli PA, Galvain T, Coursel CA, Oneto C, Feuerstadt P. Perception of quality of life in people experiencing or having experienced a Clostridioides difficile infection: a US population survey. J Patient Rep Outcomes. 2020;4(1):14.
Barbut F, Galperine T, Vanhems P, Le Monnier A, Durand-Gasselin B, Canis F, et al. Quality of life and utility decrement associated with Clostridium difficile infection in a French hospital setting. Health Qual Life Outcomes. 2019;17(1):6.
Heinrich K, Harnett J, Vietri J, Chambers R, Yu H, Zilberberg M. Impaired quality of Life, Work, and activities among adults with Clostridium difficile infection: a multinational survey. Dig Dis Sci. 2018;63(11):2864–73.
Olsen MA, Yan Y, Reske KA, Zilberberg MD, Dubberke ER. Recurrent Clostridium difficile infection is associated with increased mortality. Clin Microbiol Infect. 2015;21(2):164–70.
Finn E, Andersson FL, Madin-Warburton M. Burden of Clostridioides difficile infection (CDI) - a systematic review of the epidemiology of primary and recurrent CDI. BMC Infect Dis. 2021;21(1):456.
Fitzpatrick F, Skally M, Brady M, Burns K, Rooney C, Wilcox MH. European practice for CDI Treatment. Adv Exp Med Biol. 2018;1050:117–35.
van Prehn J, Reigadas E, Vogelzang EH, Bouza E, Hristea A, Guery B, et al. European Society of Clinical Microbiology and Infectious diseases: 2021 update on the treatment guidance document for Clostridioides difficile infection in adults. Clin Microbiol Infect. 2021;27(Suppl 2):S1–21.
European Centre for Disease Prevention and Control. Clostridioides (Clostridium) difficile infections Annual Epidemiological Report for 2016–2017. https://www.ecdc.europa.eu/en/publications-data/clostridium-difficile-infections-annual-epidemiological-report-2016-2017. Accessed 1 Dec 2022.
Balsells E, Shi T, Leese C, Lyell I, Burrows J, Wiuff C, Campbell H, Kyaw MH, Nair H. Global burden of Clostridium difficile infections: a systematic review and meta-analysis. J Glob Health. 2019;9(1):010407.
Vehreschild M, Schreiber S, von Muller L, Epple HJ, Weinke T, Manthey C, Oh J, Wahler S, Stallmach A. Trends in the epidemiology of Clostridioides difficile infection in Germany. Infection. 2023:1–8.
Brestrich G, Angulo FJ, Berger FK, Brosamle C, Hagel S, Leischker A, et al. Epidemiology of Clostridioides difficile infections in Germany, 2010–2019: a review from four public databases. Infect Dis Ther. 2023;12(4):1057–72.
Quan H, Sundararajan V, Halfon P, Fong A, Burnand B, Luthi JC, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130–9.
Centers for Disease Control and Prevention. 2014 Annual Report for the Emerging Infections Program for Clostridium difficile Infection. https://www.cdc.gov/hai/eip/pdf/cdiff/2014-Annual-CDI-Report.pdf. Accessed 1 Dec 2022.
Centers for Disease Control and Prevention. 2015 Annual Report for the Emerging Infections Program for Clostridium difficile Infection. https://www.cdc.gov/hai/eip/pdf/cdiff/2015-CDI-Report.pdf. Accessed 1 Dec 2022.
Centers for Disease Control and Prevention. 2016 Annual Report for the Emerging Infections Program for Clostridium difficile Infection. https://www.cdc.gov/hai/eip/pdf/cdiff/2016-CDI-Report-H.pdf. Accessed 1 Dec 2022.
Centers for Disease Control and Prevention. 2017 Annual Report for the Emerging Infections Program for Clostridioides difficile Infection. https://www.cdc.gov/hai/eip/pdf/cdiff/2017-CDI-Report-H.pdf. Accessed 1 Dec 2022.
Centers for Disease Control and Prevention. Emerging Infections Program Healthcare-Associated Infections–Community Interface Report Clostridioides difficile infection. 2018. https://www.cdc.gov/hai/eip/pdf/cdiff/2018-CDI-Report-H.pdf. Accessed 1 Dec 2022.
Centers for Disease Control and Prevention. Emerging Infections Program Healthcare-Associated Infections–Community Interface Report Clostridioides difficile infection, 2019 https://www.cdc.gov/hai/eip/Annual-CDI-Report-2019.html. Accessed 1 Dec 2022.
Guh AY, Mu Y, Winston LG, Johnston H, Olson D, Farley MM, et al. Trends in U.S. Burden of Clostridioides difficile infection and outcomes. N Engl J Med. 2020;382(14):1320–30.
Xia Y, Tunis MC, Frenette C, Katz K, Amaratunga K, Rose SR, House A, Quach C. Epidemiology of Clostridioides difficile infection in Canada: a six-year review to support vaccine decision-making. Can Commun Dis Rep. 2019;45(7–8):191–211.
Colomb-Cotinat M, Assouvie L, Durand J, Daniau C, Leon L, Maugat S, et al. Epidemiology of Clostridioides difficile infections, France, 2010 to 2017. Euro Surveill. 2019;24(35):1800638.
European Centre for Disease Prevention and Control. European Surveillance of Clostridioides (Clostridium) difficile infections Surveillance protocol version 2.4 https://www.ecdc.europa.eu/sites/default/files/documents/clostridium-difficile-infections-EU-surveillance-protocol-vers2.4.pdf. Accessed 1 Dec 2022.
Burckhardt F, Friedrich A, Beier D, Eckmanns T. Clostridium difficile surveillance trends, Saxony, Germany. Emerg Infect Dis. 2008;14(4):691–2.
Lubbert C, Zimmermann L, Borchert J, Horner B, Mutters R, Rodloff AC. Epidemiology and recurrence rates of Clostridium difficile infections in Germany: a Secondary Data Analysis. Infect Dis Ther. 2016;5(4):545–54.
Bauer MP, Notermans DW, van Benthem BH, Brazier JS, Wilcox MH, Rupnik M, et al. Clostridium difficile infection in Europe: a hospital-based survey. Lancet. 2011;377(9759):63–73.
Furuya-Kanamori L, Stone JC, Clark J, McKenzie SJ, Yakob L, Paterson DL, Riley TV, Doi SA, Clements AC, Comorbidities. Exposure to medications, and the risk of Community-Acquired Clostridium difficile infection: a systematic review and meta-analysis. Infect Control Hosp Epidemiol. 2015;36(2):132–41.
Pechal A, Lin K, Allen S, Reveles K. National age group trends in Clostridium difficile infection incidence and health outcomes in United States Community hospitals. BMC Infect Dis. 2016;16(1):682.
Hensgens MP, Goorhuis A, Dekkers OM, Kuijper EJ. Time interval of increased risk for Clostridium difficile infection after exposure to antibiotics. J Antimicrob Chemother. 2012;67(3):742–8.
Janarthanan S, Ditah I, Adler DG, Ehrinpreis MN. Clostridium difficile-associated diarrhea and proton pump inhibitor therapy: a meta-analysis. Am J Gastroenterol. 2012;107(7):1001–10.
Feuerstadt P, Boules M, Stong L, Dahdal DN, Sacks NC, Lang K, Nelson WW. Clinical complications in patients with primary and recurrent Clostridioides difficile infection: a real-world data analysis. SAGE Open Med. 2021;9:2050312120986733.
Sheitoyan-Pesant C, Abou Chakra CN, Pepin J, Marcil-Heguy A, Nault V, Valiquette L. Clinical and Healthcare Burden of Multiple Recurrences of Clostridium difficile infection. Clin Infect Dis. 2016;62(5):574–80.
Weinke T, Beier D, Brestrich G, von Eiff C, Hackl D, Heinrich K, Moisi J, Schley K. Epidemiology and risk factors of Clostridioides difficile infections in Germany: A Health Claims Data Analysis. Infect Dis Ther. 2023;12(5):1299–317.
Acknowledgements
Medical writing and editorial assistance were provided by Adivitiya Bihagara, Kasturi Chatterjee, and Shlok Kumar from IQVIA. We would also like to acknowledge Sandra Guedes and Margarita Landeira (Ferring Pharmaceuticals A/S) for their support in reviewing the final manuscript.
Funding
This work was supported by Ferring Pharmaceuticals A/S.
Author information
Authors and Affiliations
Contributions
FLA and SG conceptualized the study design. AT, AA, AW, HRK, SD contributed to study design and interpretation of results. AW performed the data analysis. AT and AA drafted the manuscript which was critically reviewed and approved by all authors.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study used administrative claims data that fulfils all necessary requirements of data protection in Germany. Consent to participate is not applicable. According to the Good Practice in Secondary Data Analysis, published by the Working Group for the Survey and Utilization of Secondary Data (AGENS) with representatives from the German Society for Social Medicine and Prevention (DGSMP) and the German Society for Epidemiology (DGEpi), no clearance by ethics committee is necessary for studies using anonymized secondary data.
Consent for publication
Not applicable.
Competing interests
FLA was at the time of the study employed by Ferring Pharmaceuticals A/S. AT, AA, SD, and HRK are employed by IQVIA. AW is employed by Team Gesundheit. SG is a member of steering committees for Janssen, Bristol Myers Squibb and Abbvie, participates in drug monitoring committees for Janssen, has speaker commitments for Abbvie, Takeda, Janssen, Pfizer, Gilead, Galapagos, Ferring Pharmaceuticals A/S, Eli-Lilly, Celltrion, and is a member of advisory committees for Janssen, Abbvie, Takeda, Gilead, Galapagos, Eli-Lilly, Pfizer, Celltrion, and Ferring Pharmaceuticals.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Tricotel, A., Antunes, A., Wilk, A. et al. Epidemiological and clinical burden of Clostridioides difficile infections and recurrences between 2015 − 2019: the RECUR Germany study. BMC Infect Dis 24, 357 (2024). https://doi.org/10.1186/s12879-024-09218-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-024-09218-y