Abstract
Background
Bacterial infections are considered a leading cause of hospitalization and death globally. There is still a need for a rapid and feasible biomarker for bacterial infections. Heparin-binding protein (HBP) was shown to be related to bacterial infections. The objective of the study is to investigate the diagnostic accuracy of HBP in bacterial infections.
Methods
Articles were screened in PubMed, SCOPUS, Web of Science, and Cochrane to recognize eligible studies. We included studies investigating the diagnostic accuracy of HBP and reported the necessary data to construct 2 × 2 tables. A univariate analysis was conducted to determine the pooled sensitivity and specificity, and a bivariate diagnostic random-effects model was used to calculate the optimal cut-off point.
Results
The analysis comprised sixteen studies in total. Plasma HBP showed a sensitivity of 0.90 (95% CI: [0.79, 0.96]) and a specificity of 0.87 (95% CI: [0.66, 0.96]) in diagnosing bacterial infections using blood samples. Pooling data from seven studies revealed that HBP in cerebrospinal fluid (CSF) has sensitivity and specificity of 96% (95% CI: [0.85, 0.99]), and 95% (95% CI: [0.89, 0.97]), respectively, for the diagnosis of bacterial meningitis. In urinary tract infections (UTI), urine-HBP was revealed to have a high diagnostic value in discriminating bacterial from non-bacterial UTI infection at a cut-off value of 32.868 ng/ml with sensitivity and specificity of 87%.
Conclusion
HBP has shown a high diagnostic accuracy of bacterial infections, including UTI and meningitis. Further studies are needed to determine its prognostic value and whether it could guide antibiotic therapy.
Similar content being viewed by others
Introduction
Bacterial infections are considered among the leading causes of hospitalization and death globally. Additionally, respiratory, urinary, and central nervous system bacterial infections are among the most common and serious bacterial infections in clinical settings [1].
Diagnosing bacterial infections is often challenging due to the similarities in the clinical picture of different infectious diseases [2]. Therefore, there is still a need for rapid, cheap, and feasible diagnostic techniques to tackle this issue, especially in low-income countries [3].
Moreover, using accurate diagnostic techniques is critical to avoid misdiagnosis, ineffective medications or antibiotics, and overprescribing antibiotics, which contribute to the development of antimicrobial resistance [2]. Previous observational studies have shown that up to 50% of prescribed antibiotics in clinics could be classified as unnecessary or inappropriate [4,5,6,7]. Therefore, developing rapid diagnostic tests and markers with sufficient accuracy would be necessary to improve clinical decision-making in antibiotic prescription and to limit the spread of antimicrobial resistance.
Various inflammatory markers, including procalcitonin (PCT), C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), and interleukin-6 (IL-6), have been investigated for diagnosing bacterial infections [8]. Recently, Heparin-binding protein (HBP) was reported as a promising biomarker for the diagnosis of several infectious diseases.
HBP, also known as azurocidin, is a positively charged protein of 37 kDa that is stored in secretory and azurophilic granules and is rapidly mobilized upon stimulation of neutrophils in response to bacterial infection at early stages of inflammation. It plays a critical role in vascular leakage, extravasation of neutrophils, chemo-attraction, and activation of monocytes [9].
Recent findings showed that HBP is closely related to bacterial infections. Elevated levels of HBP in cerebrospinal fluid (CSF) were significantly associated with bacterial meningitis and proved to be a useful indicator for distinguishing between bacterial and non-bacterial forms of meningitis [10, 11].
Moreover, elevated urinary HBP was significantly associated with the presence of urinary tract infections (UTI) in adults and children [12, 13]. It was also reported to be of diagnostic value in respiratory tract infections (RTI) [14].
Thus, it is a promising rapid diagnostic marker for various bacterial infections for differentiating them from non-bacterial infections and aiding physicians in making appropriate treatment plans. However, the sample size in previous studies was limited, and most of the studies were single-center studies, so their findings may not be generalizable, and the diagnostic accuracy of HBP remains uncertain.
The objective of this study is to combine the existing evidence and examine the diagnostic value of HBP in different bacterial infections.
Materials and method
Literature search
The systematic review and meta-analysis were performed in accordance with the guidelines of the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [15]. We searched PubMed, Scopus, Web of Science, and Cochrane for relevant studies. The Medical Subject Headings (MeSH) terms and keyword search terms used were ("heparin-binding protein," OR "Heparin binding protein" OR "azurocidin”). All studies retrieved from these databases were assessed without limitations.
Inclusion and exclusion criteria
Studies were included in the analysis if they evaluated the ability of HBP to diagnose bacterial vs. non-bacterial infections in adults accurately. The studies needed to provide enough data to construct a 2*2 table and to calculate true positives, true negatives, false positives, and false negatives.
Studies were excluded if they lacked the necessary data to construct a 2*2 table, did not directly compare bacterial and non-bacterial infections, were not written in English, or were reviews, correspondence, editorials, case reports, animal studies, or conference abstracts. The goal was to evaluate the diagnostic accuracy of high blood pressure in distinguishing bacterial from non-bacterial infections.
Data extraction and quality assessment
The studies were evaluated by two authors independently who followed the inclusion and exclusion criteria. Data extraction and quality assessment were also done independently by two authors. They extracted information on study characteristics such as author, publication year, study design, country, and period. Patient characteristics such as eligibility criteria, patient source, type of sample, and time of collection, as well as clinical and demographic information of the patients, were also extracted, along with diagnostic criteria, outcomes, and accuracy parameters. Quality assessment was done using the Quality Assessment of Diagnostic Accuracy Studies (QUADAS-2) tool.
Statistical analysis
Data were extracted and verified, then fed to R statistical software version 4.2.2 "Innocent and Trusting". A univariate analysis was done to determine the pooled sensitivity, specificity, and diagnostic odds ratio (DOR) using random effect models [16]. Additionally, a bivariate diagnostic random-effects meta-analysis was used to calculate the optimal cut-off point and the pooled area under the Summary Receiver Operating Characteristic (SROC) curve using the common random intercept method (CI) [17]. Mixed-effects models were conducted to examine the potential moderators explaining the heterogeneity in effect size between studies. The publication bias was also tested via a funnel plot Deek's test, after which the potential publication bias was adjusted using trim-and-fill methods, imputing studies that had been missed and then re-estimating the effect size after adjustment. Cochran's Q test was utilized to examine heterogeneity, and it was based on a chi-square distribution, and a p-value < 0.05 was considered statistically significant. The degree of heterogeneity was measured using the I2 index, and an I2 value of less than 40% indicated that the heterogeneity may not be significant. A value between 30% and 60% was considered moderate, between 50% and 90% indicated substantial heterogeneity, and an I2 value exceeding 75% was considered considerable heterogeneity [18].
Results
Summary of eligible studies
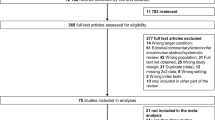
After searching the literature, we identified 5170 studies, and two studies were retrieved by manual search. Among these studies, 3068 duplicates were removed, and 1931 were excluded by screening their titles and abstract, and the remaining 171 underwent further evaluation. After reading the full text of these articles, 155 studies were excluded. Thus, 16 studies met the inclusion criteria and were incorporated in the meta-analysis. The study selection process and causes of exclusion are shown in Fig. 1.
Characteristics of included studies
Tables 1 and 2 list the characteristics of 16 included studies and patients. Fourteen studies included adult patients aged ≥ 18 years old (87.5%). Among the included studies, seven studies enrolled patients with central nervous system (CNS) infections, and four enrolled patients with urinary tract infections (UTI). In contrast, two studies enrolled patients with both bacterial and viral infections. The type of samples was either blood in eight studies [10, 11, 19,20,21,22,23], CSF in seven studies [10, 11, 21, 24,25,26,27], and urine in four studies [12,13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29]. HBP was assessed in different samples in all included studies.
Assessment of risk of bias
Figure 2 displays the risk of bias assessment details. In the patient selection domain, ten studies (62.5%) had high-risk patient selection bias, primarily due to the use of a case-control study design [12, 21,22,23,24,25, 27,28,29], or inappropriate patient selection [11, 12, 21,22,23,24,25, 27,28,29]. In the index test domain, ten studies (62.5%) had a high risk of bias as they lacked a pre-specified cut-off threshold or interpretation bias [12, 21,22,23,24, 26,27,28]. For the reference standard domain, ten studies (62.5%) had unclear risk of bias due to interpretation bias or lack of knowledge of index test results [10, 11, 19, 22,23,24,25,26,27, 29]. The risk of bias for the flow and timing domain was low in all studies. None of the studies had any concerns for applicability in any domain, whether high or unclear.
Meta-analysis of the diagnostic accuracy of hbp in the diagnosis of bacterial infections
Plasma HBP levels and the diagnosis of bacterial infections
Univariate analysis and meta-regression
The analysis involved eight individual studies investigating the diagnostic accuracy of HBP in plasma in cases of bacterial infection. The random-effects meta-analysis model showed that the pooled sensitivity was 0.90 with 95%CI: [0.79, 0.96], the between-study heterogeneity was considerable (I^2 =78%), heterogeneity variance (tau^2 = 1.4133), and there was a significant test for heterogeneity (p< 0.01) (Figure S1-a). Leave-one-out test showed that the heterogeneity would be resolved by omitting Obreja et al. 2022 study (0.92, 95% CI [0.84, 0.96], I^2 = 39%) (Fig. 3a). The pooled specificity was 0.87 with 95%CI: [0.66, 0.96], the between-study heterogeneity was considerable (I^2 =88%), a heterogeneity variance (tau^2 = 2.8576), and there was also a significant test for heterogeneity (p< 0.01) (Figure S1-b). However, the heterogeneity was not resolved by conducting the leave-one-out test (Fig. 3b).
The pooled DOR was 48.04 with 95% CI: [9.50, 242.85], the between-study heterogeneity was (I^2 = 89%), a heterogeneity variance (tau^2 = 4.6388), and the heterogeneity test was significant (p< 0.01) (Figure S2-a). The heterogeneity was not resolved by the leave-one-out test (Figure S2-b).
The age, gender, HBP at baseline, the used cut-off values, and the publication year have been considered non-statistically significant moderators for the between-studies heterogeneity in effect size (Table S1, Figure S3).
Bivariate diagnostic random effects
At the cut-off point of 32.381 ng/ml, the sensitivity and specificity were 0.7231, 95% CI [0.3166, 0.9364] and 0.7231, 95% CI [0.2794, 0.9462], respectively. The pooled AUC was 0.7853 with 95% CI [0.2642, 0.9780] (Fig. 4).
CSF HBP levels and the diagnosis of CNS infections
Univariate analysis and meta-regression
The analysis included seven studies examining the diagnostic utility of HBP in the CSF of patients with CNS infections, mostly meningitis. The random-effects meta-analysis model revealed a pooled sensitivity of 0.96 with 95% CI: [0.85, 0.99], the between-study heterogeneity was considerable (I^2= 81%), a heterogeneity variance (tau^2 = 2.2582), and a significant test for heterogeneity (p < 0.01) (Figure S4-a). The heterogeneity was not resolved by the leave-one-out test (Fig. 5a). The pooled specificity was 0.95 with 95% CI: [0.89, 0.97], the between-study heterogeneity was moderate (I^2= 56%), the heterogeneity variance was 0.7219, and the heterogeneity test was significant (p = 0.04) (Figure S4-b). Leave one out test showed that the heterogeneity resolved after omitting the Kong et al. 2022 study (0.95, 95% CI [0.87, 0.98], I^2 = 44%) (Fig. 5b).
The pooled DOR was 234.53 with 95% CI: [56.04, 981.45], the between-study heterogeneity was considerable (I^2= 80%), the heterogeneity variance was 2.7402, and there was a significant test for heterogeneity (p < 0.01) (Figure S5-b). The heterogeneity was not resolved by the leave-one-out test (Figure S5-b).
The meta-regression analysis has revealed that the HBP at baseline can be considered as a statistically significant moderator for the between-studies heterogeneity in effect size, and there was 67.21% residual heterogeneity after including the HBP at baseline as a covariate (p-value= 0. 0268) (Table S2, Figure S6).
Urinary HBP and the Diagnosis of UTI
Univariate analysis and meta-regression
The analysis involved four individual studies investigating the diagnostic accuracy of urine-HBP in cases of bacterial infection. The fixed-effects meta-analysis model showed that the pooled sensitivity was 0.91 with 95% CI: [0.87, 0.94], the between-study heterogeneity was not significant (I^2 =0%), heterogeneity variance (tau^2 = 0.0521), and there was an insignificant test for heterogeneity (p = 0.57) (Fig. 6a). The pooled specificity was 0.87 with 95%CI: [0.77, 0.93], the between-study heterogeneity was considerable (I^2 =94%), a heterogeneity variance (tau^2 = 2.6542), and there was also a significant test for heterogeneity (p< 0.01) (Figure S7). The heterogeneity was resolved by omitting the Kjolvmark et al. 2016 study (0.91, 95% CI [0.86, 0.94], I^2 = 0%) (Fig. 6b).
The pooled DOR was 63.35 with 95% CI: [17.05, 235.42], the between-study heterogeneity was moderate (I^2 = 56%), a heterogeneity variance (tau^2 = 0.9379), and the heterogeneity test was significant (p = 0.08) (Figure S8-b). The heterogeneity was resolved by leaving out Kjolvmark et al. 2016 study (83.57, 95% CI [43.60, 160.16], I^2 = 0%) (Figure S8-b).
2. Bivariate Diagnostic Random Effects
At the cut-off value of 32.868 ng/ml, the sensitivity and specificity were 0.8795, 95% CI [0.3731, 0.9889] and 0.8795, 95% CI [0.3969, 0.9878], respectively. The pooled AUC was 0.9416 with 95% CI [0.3156, 0.9972] (Fig. 7).
Discussion
Bacterial infection is recognized as a triggering cause of various complications, including hepatic encephalopathy, liver and renal failure, coagulation disorders, and death. Therefore, early detection of bacterial infections is critical but difficult due to the similarities in the clinical presentation of different infectious diseases. Also, the bacterial culture, which is the gold standard diagnostic test for bacterial infections, has poor sensitivity and delayed results.
Therefore, a rapid and more accurate laboratory biomarker is required. HBP could be considered an easy and rapid laboratory test with potential diagnostic value in bacterial infections. The results of the following meta-analysis, including 16 studies, indicated that HBP is an effective biomarker for the diagnosis of different bacterial infections, including UTI and CNS infections while discriminating them from non-bacterial infections.
CSF analysis is considered the gold standard for the confirmation of a suspected case of bacterial meningitis [30]. Pooling data from seven studies resulted in an HBP sensitivity and specificity of 96% and 95% for the diagnosis of bacterial meningitis. Additionally, the diagnostic accuracy of elevated CSF HBP appeared to be superior to blood HBP.
Several of the studies included in the analysis evaluated the diagnostic effectiveness of HBP in conjunction with other biomarkers or compared it to them in the diagnosis of CNS infections. Kong et al. showed that CSF HBP concentrations were superior to CSF PCT or lactate concentrations in the identification of nosocomial meningitis or ventriculitis, suggesting its utility in the early identification of patients with bacterial infections. The sensitivity and negative predictive value of HBP were higher than lactate. At the same time, the specificity was lower than it, indicating that CSF HBP is more valuable for confirmation of the presence of infection with a low risk of missed diagnosis [24].
Whereas lactate would be more suggestive of an active infection, with a low probability of misdiagnosis. On the contrary, CSF PCT revealed poor sensitivity among included patients, and PCT concentrations were normal in some patients despite being diagnosed with meningitis or ventriculitis, suggesting that CSF PCT values have little clinical utility and can be used for the exclusion of nosocomial infections. So, only the early and simultaneous measurement of CSF HBP and lactate biomarkers was suggested to be more clinically useful in cases suspected of nosocomial meningitis or ventriculitis [24].
The lack of diagnostic utility of CSF PCT in the diagnosis of bacterial intracranial infection was also confirmed by Zhang et al. The author revealed that the AUC of HBP was greater than that of PCT alone or in combination with HBP [27].
CSF HBP was found to be a superior diagnostic tool for bacterial meningitis than other biomarkers, such as neutrophil gelatinase-associated lipocalin (NGAL) and S100 calcium-binding protein B (S100B). CSF HBP demonstrated an exceptional ability to differentiate between bacterial and viral meningitis [10].
Moreover, serum and CSF HBP levels were higher in children with purulent meningitis than those with viral meningitis compared to other infection biomarkers, including PCT, CRP, and tumor necrosis factor (TNF)-α. Additionally, HBP showed the highest diagnostic value among those four biomarkers [26].
In UTI, we found that the urine-HBP is of high diagnostic value in discriminating bacterial from non-bacterial UTI infection at a cut-off value of 32.868 ng/ml with sensitivity and specificity and pooled AUC of 87%, 87%, and 94%, respectively.
Urine-HBP showed a higher specificity than white blood cell count and Il-6 in the diagnosis of UTI and greater sensitivity than nitrite in children [13]. However, it showed a low discriminatory value between the elderly with UTI and those with asymptomatic bacteriuria compared to IL-6 despite having a higher negative predictive value (93.5% vs. 74-76% for urine-HBP and urine IL-6, respectively).
This could be explained by the elevated urine HBP in both patients with asymptomatic bacteriuria due to the inflammatory response and excess neutrophil lysis and those with UTI due to the pro-inflammatory response and excess HBP release. At the same time, IL-6 is lower in patients with asymptomatic bacteriuria due to the absence of a pro-inflammatory IL-6 response in contrast to those with UTI. However, urine HBP could still be considered a potential biomarker for ruling out UTI [28].
Strengths and limitations of the study
Regarding the strengths, we conducted bivariate models which are significantly associated with the low influence of threshold effects [31]. Additionally, the diagnostic accuracy of HBP in various bacterial infections was reviewed for the first time through the current systematic review and meta-analysis.
One of the limitations of our study was that we restricted our search to studies published in English, which may limit the applicability of our results. Additionally, there was notable heterogeneity among the included studies that we tried to address its source by leave-one-out test. The patient population, testing interval time, and cut-off value used may have contributed to the detected heterogeneity. Some of the studies have reported their results insufficiently, thus impacting data extraction and quality assessment. Additionally, the included studies were characterized by small sample sizes and different study populations, which may impact the immune response to infections. Three out of four UTI patient studies were authored by the same researcher, raising concerns about potential duplication and over-representation. However, we conducted a thorough investigation to detect any such duplications, which were not found. This was supported by the fact that these studies were carried out in different years and with different inclusion criteria and study design. Furthermore, we performed a thorough sensitivity analysis to ensure the robustness of our findings.
Conclusion
In summary, the available data support the diagnostic utility of HBP levels in the diagnosis of bacterial infections. Our analysis supports the high diagnostic accuracy of HBP in the blood, urine, or CSF in diagnosing UTI and CNS infections. However, the diagnostic value of HBP, along with other biomarkers such as PCT, CRP, or IL-6, as well as the specific time for the test, would require further investigations. Additionally, more studies are needed to determine if HBP levels are correlated with the prognosis of bacterial infections and whether they can be used safely and effectively to guide antibiotic therapy.
Availability of data and materials
All data generated or analyzed during this study are included in this published article or the data repositories listed in References.
References
Ikuta KS, et al. Global mortality associated with 33 bacterial pathogens in 2019: a systematic analysis for the Global Burden of Disease Study 2019. Lancet. 2022;400(10369):2221–48. https://doi.org/10.1016/S0140-6736(22)02185-7.
Rentschler S, Kaiser L, Deigner HP. Emerging Options for the Diagnosis of Bacterial Infections and the Characterization of Antimicrobial Resistance. Int J Mol Sci. 2021;22(1):1–29. https://doi.org/10.3390/IJMS22010456.
Srivastava S, Singh PK, Vatsalya V, Karch RC. Developments in the diagnostic techniques of infectious diseases: rural and urban prospective. Adv Infect Dis. 2018;8(3):121. https://doi.org/10.4236/AID.2018.83012.
N. N. Hagedoorn et al., Variation in antibiotic prescription rates in febrile children presenting to emergency departments across Europe (MOFICHE): a multicentre observational study. PLoS Med. 2020; 17(8). https://doi.org/10.1371/JOURNAL.PMED.1003208.
B. Croche Santander et al. [Appropriateness of antibiotic prescribing in paediatric patients in a hospital emergency department]. An Pediatr. 2018; 88(5):259–265, https://doi.org/10.1016/J.ANPEDI.2017.06.001.
García-Moreno FJ, et al. Adecuacy of pediatric antimicrobial prescribing in the Emergency Department at discharge. An Pediatr. 2022;96(3):179–89. https://doi.org/10.1016/j.anpedi.2020.11.019.
Renati S, Linder JA. Necessity of office visits for acute respiratory infections in primary care. Fam Pract. 2016;33(3):312–7. https://doi.org/10.1093/FAMPRA/CMW019.
Qu J, Lü X, Liu Y, Wang X. Evaluation of procalcitonin, C-reactive protein, interleukin-6 & serum amyloid A as diagnostic biomarkers of bacterial infection in febrile patients. Indian J Med Res. 2015;141(3):315–21. https://doi.org/10.4103/0971-5916.156617.
Linder A, Soehnlein O, Kesson P. Roles of Heparin-Binding Protein in Bacterial Infections. J Innate Immun. 2010;2(5):431–8. https://doi.org/10.1159/000314853.
M. Obreja et al. Heparin-Binding Protein (HBP), Neutrophil Gelatinase-Associated Lipocalin (NGAL) and S100 Calcium-Binding Protein B (S100B) Can Confirm Bacterial Meningitis and Inform Adequate Antibiotic Treatment. Antibiot. (Basel, Switzerland). 2022; 11(6). https://doi.org/10.3390/ANTIBIOTICS11060824.
E. S. Namiduru, M. Namiduru, İ. Karaoğlan, and E. Erbağci. Heparin Binding Protein in Early Differential Diagnosis of Bacterial Meningitis. Indian J Clin Biochem. 2022:1–6. https://doi.org/10.1007/S12291-022-01066-4/METRICS.
C. Kjölvmark, L. I. Påhlman, P. Åkesson, and A. Linder. Heparin-Binding Protein: A Diagnostic Biomarker of Urinary Tract Infection in Adults. Open Forum Infect. Dis. 2014; 1 (1). 2014. https://doi.org/10.1093/OFID/OFU004.
Kjölvmark C, Åkesson P, Linder A. Elevated urine levels of heparin-binding protein in children with urinary tract infection. Pediatr Nephrol. 2012;27(8):1301–8. https://doi.org/10.1007/S00467-012-2132-X.
Ma J, Lu Q, Tu S, Miao X, Zhao J. A diagnostic test: combined detection of heparin-binding protein, procalcitonin, and C-reactive protein to improve the diagnostic accuracy of bacterial respiratory tract infections. J Thorac Dis. 2022;14(3):721–8. https://doi.org/10.21037/JTD-22-260/COIF).
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. BMJ. 2009;339(7716):332–6. https://doi.org/10.1136/BMJ.B2535.
Shim SR, Kim SJ, Lee J. Diagnostic test accuracy: application and practice using R software. Epidemiol Health. 2019;41:e2019007. https://doi.org/10.4178/EPIH.E2019007.
Steinhauser S, Schumacher M, Rücker G. Modelling multiple thresholds in meta-analysis of diagnostic test accuracy studies. BMC Med Res Methodol. 2016;16(1):1–15. https://doi.org/10.1186/S12874-016-0196-1/FIGURES/6.
D. G. A. (Editors) Jonathan J Deeks, Julian PT Higgins, “Chapter 10: Analysing data and undertaking meta-analyses. Cochrane handbook for systematic reviews of interventions version 6.3 (updated February 2022),” in Cochrene, 2023. [Online]. Available: https://training.cochrane.org/handbook/current/chapter-10#section-10-10-2
R. Cai, H. Li, and Z. Tao. Heparin-binding protein and procalcitonin in the diagnosis of pathogens causing community-acquired pneumonia in adult patients: A retrospective study. PeerJ, 2021; 9. https://doi.org/10.7717/PEERJ.11056/SUPP-2.
Chalupa P, Beran O, Herwald H, Kaspříková N, Holub M. Evaluation of potential biomarkers for the discrimination of bacterial and viral infections. Infection. 2011;39(5):411–7. https://doi.org/10.1007/S15010-011-0126-4.
Kandil M, Khalil G, El-Attar E, Shehata G, Hassan S. Accuracy of heparin binding protein: as a new marker in prediction of acute bacterial meningitis. Brazilian J Microbiol. 2018;49(Suppl 1):213. https://doi.org/10.1016/J.BJM.2018.05.007.
Niu T, Liu Y, Zhu F, Ma J, Gao J. Time-resolved fluorescent immunoassay-based combined detection of procalcitonin, C-reactive protein, heparin binding protein, and serum amyloid A1 to improve the diagnostic accuracy of early infection. J Clin Lab Anal. 2019;33(2):e22694. https://doi.org/10.1002/jcla.22694.
X. Yang, Y. Zhang, H. Lin, H. Zhong, and Z. Wu. Diagnostic Value of the Triple Combination of Serum Heparin-Binding Protein, Procalcitonin, and C-Reactive Protein in Children with Acute Bacterial Upper Respiratory Tract Infection,” J Healthc Eng. 2022; 2022. https://doi.org/10.1155/2022/1877960.
Kong Y, Ye Y, Ma J, Shi G. Accuracy of heparin-binding protein for the diagnosis of nosocomial meningitis and ventriculitis. Crit Care. 2022;26(1):1–10. https://doi.org/10.1186/S13054-022-03929-X/TABLES/4.
Linder A, Åkesson P, Brink M, Studahl M, Björck L, Christensson B. Heparin-binding protein: a diagnostic marker of acute bacterial meningitis. Crit Care Med. 2011;39(4):812–7. https://doi.org/10.1097/CCM.0B013E318206C396.
D. Ren, D. Wu, F. Liu, S. Jiao, and Y. Wu, “Diagnostic value of heparin-binding protein in the cerebrospinal fluid for purulent meningitis in children,” Brazilian J. Med. Biol. Res. = Rev Bras Pesqui Medicas e Biol. 2021; 54(11). https://doi.org/10.1590/1414-431X2021E11295.
Zhang S, et al. Evaluation of heparin-binding protein and / or procalcitonin levels in the diagnosis of bacterial intracranial infection using receiver operating characteristic ( ROC ) curve value. Int J Clin Exp Med. 2019;12(6):7778–82.
Kjölvmark C, Tschernij E, Öberg J, Påhlman LI, Linder A, Åkesson P. Distinguishing asymptomatic bacteriuria from urinary tract infection in the elderly - the use of urine levels of heparin-binding protein and interleukin-6. Diagn Microbiol Infect Dis. 2016;85(2):243–8. https://doi.org/10.1016/J.DIAGMICROBIO.2016.03.005.
Lertdumrongluk K, Thongmee T, Kerr SJ, Theamboonlers A, Poovorawan Y, Rianthavorn P. Diagnostic accuracy of urine heparin binding protein for pediatric acute pyelonephritis. Eur J Pediatr. 2015;174(1):43–8. https://doi.org/10.1007/S00431-014-2362-Y.
Li Y, et al. The diagnostic value of cerebrospinal fluids procalcitonin and lactate for the differential diagnosis of post-neurosurgical bacterial meningitis and aseptic meningitis. Clin Biochem. 2015;48(1–2):50–4. https://doi.org/10.1016/J.CLINBIOCHEM.2014.10.007.
Reitsma JB, Glas AS, Rutjes AWS, Scholten RJPM, Bossuyt PM, Zwinderman AH. Bivariate analysis of sensitivity and specificity produces informative summary measures in diagnostic reviews. J Clin Epidemiol. 2005;58(10):982–90. https://doi.org/10.1016/J.JCLINEPI.2005.02.022.
Acknowledgments
None.
Code availability
Not applicable.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB). No funding to report.
Author information
Authors and Affiliations
Contributions
Amira Mohamed Taha: Study conception and design, literature search, data collection, manuscript review and editing. Khaled Abouelmagd, Mohamed Mosad Omar, Qasi Najah: Screening, data extraction, quality assessment. Mohammed Ali: data extraction, quality assessment. Mohammed Tarek Hasan: Meta-analysis. Sahar A. Allam: Manuscript writing. Omar El Sayed Rageh& Roua Arian: Data extraction. Mohamed Abd-ElGawad: Supervision and manuscript peer-review.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Figure S1. The Univariate Analysis for Plasma HBP in Diagnosing Bacterial Infections Before Leave-one-out Test; (a) Forest Plot of Pooled Sensitivity; (b) Forest Plot of Pooled Specificity.Figure S2. (a) Forest Plot of the Diagnostic Odds Ratio (DOR) of Plasma HBP for the Diagnosis of Bacterial Infections; (b) Forest Plot of the DOR of Plasma HBP for the Diagnosis of Bacterial Infections After the Leave-one-out Test. Table S1. Results of Meta-regression Analysis of Studies Investigating Plasma HBP. Figure S3. Deek's Funnel Plot Showing the Effect of HBP Cut-off values on the Effect Size in Studies Investigating Plasma HBP. Figure S4. The Univariate Analysis for CSF HBP in Diagnosing CNS Infections Before Leave-one-out Test; (a) Forest Plot of Pooled Sensitivity; (b) Forest Plot of Pooled Specificity. Figure S5. (a) Forest Plot of the diagnostic Odds Ratio (DOR) of CSF HBP for the Diagnosis of CNS Infections; (b) Forest Plot of the DOR of CSF HBP for the Diagnosis of CNS Infections After the Leave-one-out Test. Table S2. Results of Meta-regression Analysis of Studies Investigating CSF HBP. Figure S6. Deek's Funnel Plot Showing the Effect of HBP at Baseline on the Effect Size in Studies Investigating CSF HBP. Figure S7. Forest Plot of Pooled Specificty of Urinary HBP in Diagnosing Urinary Tract Infections Before Leave-one-out Test. Figure S8. (a) Forest Plot of the diagnostic Odds Ratio (DOR) of Urinary HBP for the Diagnosis of Urinary Tract Infections; (b) Forest Plot of DOR of Urinary HBP for the Diagnosis of Urinary Tract Infections After the Leave-one-out Test.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Taha, A.M., Abouelmagd, K., Omar, M.M. et al. The diagnostic utility of heparin-binding protein among patients with bacterial infections: a systematic review and meta-analysis. BMC Infect Dis 24, 150 (2024). https://doi.org/10.1186/s12879-024-09004-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-024-09004-w