Abstract
Background
Weeksella virosa pneumonia is an infection that has been described as a healthcare-associated infection. This is a rare gram-negative anaerobic bacterium associated with the use of mechanical ventilation for a long period of time and is more frequent in immunosuppressed patients. This is the first case reported in the state of Veracruz and the second in Mexico.
Case presentation
We present the case of a 64-year-old female from Veracruz, Mexico who developed an infectious process in the right pelvic limb after a transcatheter aortic valve replacement procedure and subsequently developed sudden cardiorespiratory arrest requiring mechanical ventilation, with subsequent imaging studies demonstrating a pneumonic process associated with a nosocomial infection.
Discussion and Conclusions
We should take into consideration that this pathogen affects not only adults with multiple comorbidities but also children with renal, hepatic, or oncological pathologies, as well as immunocompromised patients, who should be considered high-risk populations for W. virosa infection.
Similar content being viewed by others
Introduction
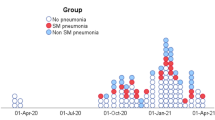
Health Care Associated Infections (HCAIs), also known as nosocomial or in-hospital infections, are defined as infections acquired by a patient during treatment in a hospital or other health facility, excluding the possibility that the patient had or was incubating the pathogen at the time of admission. This definition also includes patients who have been discharged and occupational infections contracted by health personnel. (Fig. 1) [1].
The risk of acquiring such an infection is 5 to 10%, with a higher risk in Intensive Care Unit (ICU) personnel, reaching up to 20–40% [2]. The prevalence of mechanical ventilation-associated pneumonia is 5–50% in patients who require mechanical ventilation for more than 48 h, with an average time of development of 5–9 days of mechanical ventilation [3, 4].
Among the most frequent agents are gram-positive bacteria such as methicillin-resistant Staphylococcus aureus and Streptococcus pneumoniae and gram-negative bacteria such as Pseudomonas aeruginosa, Acinetobacter baumanni, Enterobacteria (Escherichia coli and Klebsiella pneumoniae) and Haemophilus influenzae, although new microorganisms such as W. virosa have recently been reported as etiologic agents [1, 4].
Weeksella virosa is an uncommon gram-negative aerobic bacterium, first described in 1970 by Pickett and Manclark as a nonsaccharolytic flavobacteria and identified according to Gram staining as negative in the form of bacillus, which can be grown in chocolate agar and blood agar after 48 h incubation at 22, 35 and 42 °C [5,6,7]. It must not be confused with Bergeyella zoohelcum (formerly part of the genus Weeksella), which is associated with infection from animal bites [8]. The difference between the two species is that B. zoohelcum is urease positive and has an innate resistance to polymyxin [8,9,10,11].
This microorganism is usually detected and isolated when susceptibility tests are performed in the group of other non-Enterobacteriaceae gram-negative bacilli [5]. It is clinically associated with bacteremia, peritonitis and urinary infections in immunocompromised patients and nosocomial infections [12]. It is more prevalent in female patients and patients with comorbidities such as kidney disease, obesity, hepatopathy and diabetes, as well as those in intensive care units [13, 14].
The few occasions in which this organism has been isolated have been in urine samples (43%), cervical exudates (14%) and vaginal exudates (16%) [12, 13, 15, 16]. However, it has been isolated twice from blood and spinal fluid samples. Mardy et al. reported that of the vaginal exudate samples, a 2% incidence was found in asymptomatic patients or those presenting some symptom of vaginal infection [16]. Interestingly, a group in an English prison reported an incidence of 15% in patients who had a high risk of sexually transmitted diseases [16].
It is important to consider this bacteria if a gram-negative aerobic bacillus grows after 36 to 48 h of incubation in cultures of blood, sputum, urine, or peritoneal fluid [12, 16, 14, 17,18,19,20]. Once the pathogen is isolated, the empirical use of piperacillin, aztreonam or a carbapenem antibiotic is recommended. TMP-SMX, ciprofloxacin and aminoglycosides should not be used unless an antibiogram showing susceptibility is available [16, 21].
This organism has the particularity of not growing in MacConkey agar, and the culture usually has an extremely mucous and cream color with an orange/yellowish pigment [6, 7, 9, 10]. Biochemically, the organism is positive for oxidase, indole and catalase (Fig. 2) [6, 7]. In vitro susceptibility studies report the effectiveness of the following antibiotics against this microorganism: piperacillin, monobactam, cephalosporins, fluoroquinolones and carbapenems [5]. Resistance has been noted in vitro with the use of aminoglycosides, nalidixic acid and nitrofurantoin.
Case presentation
We present the case of a 64-year-old female patient from Soledad de Doblado, Veracruz, who was referred to our hospital in a coma on mechanical ventilation without sedation with broad-spectrum antimicrobial treatment. Seven days before her arrival, in another hospital, a transcatheter aortic valve implantation (TAVI) procedure was performed due to a history of aortic stenosis, severe aortic insufficiency, and KDIGO III renal chronic disease. During the postoperative period, she presented cardiac arrest, requiring advanced resuscitation maneuvers with airway management, and three cycles of cardiopulmonary resuscitation were given before returning to spontaneous circulation. She was then admitted to the ICU under sedation, invasive mechanical ventilation, antibiotics and thromboprophylaxis. Upon admission to our hospital, a skull CT scan was performed with no evidence of injury. An electroencephalogram was also performed, which was reported as compatible with ischemic encephalopathy, considered probable brain death.
At physical examination, the patient was dependent on vasoactive amines, with a temporary pacemaker, on mechanical ventilation, and without sedation. The pupils were myotic and unresponsive to luminous or external stimuli, and a 3-point Glasgow Coma Scale at pulmonary auscultation showed bilateral crackling rales on both lung bases.
Paraclinics performed at admission are reported: gasometry values suggesting metabolic acidosis with added respiratory alkalosis and leukocytosis of 17,000 with predominance of polymorphonuclear cells. A chest radiograph was obtained and demonstrated the presence of a pneumonic process with basal pulmonary consolidations. A subsequent simple chest CT was performed, which demonstrated bilateral pleural effusion (Fig. 3). Bronchoalveolar lavage was performed, and collected samples were placed on blood agar, chocolate agar and MacConkey agar. Gram-negative bacilli were isolated on blood agar, which were later identified using the VITEK technique and PCR sequencing as oxidase and catalase positive and determined by results such as Weeksella virosa.
When this culture was subjected to the Kirby-Bauer method and MIC bacterial susceptibility test using a Mueller-Hinton agar plate, the presence of extended-spectrum beta-lactamase (ESBL) negativity, sensitivity to ciprofloxacin, intermediate sensitivity to tigecycline and resistance to ampicillin/sulbactam, piperacillin/tazobactam, cephalosporins (cefoxitin, ceftazidime, ceftriaxone and cefepime), carbapenems (meropenem, imipenem, ertapenem and doripenem) and aminoglycosides (amikacin and gentamicin) were reported.
The results of these tests were as follows:
Antibiotics | MIC | Sensitivity |
|---|---|---|
Ampicillin/Sulbactam | >=32 | Resistant |
Piperacillin/Tazobactam | >=128 | Resistant |
Cefoxitin | >=64 | Resistant |
Ceftazidime | 32 | Resistant |
Ceftriaxone | >=64 | Resistant |
Cefepime | >=64 | Resistant |
Meropenem | >=16 | Resistant |
Imipenem | 4 | Resistant |
Ertapenem | >=8 | Resistant |
Doripenem | >=8 | Resistant |
Amikacin | >=64 | Resistant |
Gentamicin | >=16 | Resistant |
Tigecycline | 4 | Intermediate sensitivity |
Ciprofloxacin | 0.5 | Sensitive |
We then decided to start treatment with ciprofloxacin for 10 days with a favorable response, with resolution of the pneumonic process after 10 days of antibiotics.
Discussion
This case presents an opportunity to report emerging microorganisms in our country and represents an opportunity to detect new agents in the field of infections associated with healthcare. Compared to the reviewed bibliographies, our case resembles the reports of other countries and agrees with the characteristics referred by them; therefore, we would improve the information available about this etiological agent and the treatments used to eradicate these infections.
Our case closely resembles the clinical presentation reported in the literature, with the patient being a female, with multiple comorbidities that, after requiring mechanical ventilation, develop ventilator-associated pneumonia. It is also important to point out that the incidence in hospitals in our region is 0, and this case represents the first appearance of a new microorganism in our region, so it is important to report its clinical and microbiological characteristics to start considering it as a causative agent of intrahospital pneumonia. Within its microbiological characteristics, our case perfectly agrees with the appearance in Blood Agar of an extremely mucous bacterial culture after the reported incubation time and requiring a nonempirical treatment in this case ciprofloxacin as in those reported in the literature that this antibiotic was used after having an antibiogram that showed susceptibility to it.
Conclusion
We must start to consider new etiological agents associated with nosocomial infections, which are identified thanks to new technologies, such as molecular techniques, allowing us to update the treatment guidelines and learn which are the most frequent bacteria in our country. This is the first case reported in the state of Veracruz and the second in Mexico. We should consider that this pathogen affects not only adults with multiple comorbidities but also children with renal, hepatic, or oncological pathologies, as well as immunocompromised patients, who should be considered high-risk populations for W. virosa infection. The identification of new pathogens by using molecular techniques is a great opportunity to expand epidemiological surveillance and establish new guidelines for empirical antibiotic therapies.
More clinical information, diagnosis and treatment of this rare pathogen is needed. A review of the literature from 1990 to 2022 found only 13 cases with Weeksella virosa infections.(Table 1). We found that these cases presented with the following clinical syndromes: pneumonia (2/13), spontaneous bacterial peritonitis (2/13), sepsis (3/13), urinary tract infection (2/9), pneumonia (2/13), infection of a surgical head wound with ventriculitis (1/13), chorioamnionitis (1/13) and surgical wound infection (1/13). Nine of the 13 cases, including ours, have been found in the last 10 years, which interestingly shows an increase in the incidence of infection by this bacterium in humans. Currently, no risk factor directly involved has been established, but all patients who presented with this infection presented at least one comorbidity, such as diabetes mellitus (3/13), end-stage renal disease (5/13), hepatitis C virus infection (1/13), ischemic heart disease (1/13), lymphoma (1/13) or anaplastic meningioma (1/13) [16].
Data availability
The data sets generated and/or analyzed during this study are not publicly available because they are owned by a federal public hospital but are available from the corresponding author upon reasonable request.
References
BUAP, HU de Puebla. Iinfecciones asociadas a la atenciÓn de la salud (IAAS). [Internet]. 2017. Available from http://cmas.siu.buap.mx/portal_pprd/work/sites/hup/resources/LocalContent/247/2/PRESENTACION INFECCIONES ASOCIADAS A LA ATENCION DE LA SALUD.pdf.
León-Gutiérrez MA, García-Peniche C, Loza-Jalil S, Serrano-Cuevas L, Romero-Gutiérrez L, Tanus-Hajj J, Flores-Cima R. Infecciones asociadas a la atención De La Salud: tratamiento antibiótico empírico apropiado. Revista médica Del Instituto Mexicano Del Seguro Social. 2017;55(Suppl 4):383–S388. http://www.ncbi.nlm.nih.gov/pubmed/29792794.
Miller F. Ventilator associated pneumonia. Anesthesia Tutorial of The Week 2018;382:1–6. https://www.wfsahq.org/components/com_virtual_library/media/5e63c8f14e8a46c186bb0f73eafa2950-atow-382-00-01.pdf.
Papazian L, Klompas M, Luyt CE. Ventilator-associated Pneumonia in adults: a narrative review. Intensive Care Med. 2020;46(5):888–906. https://doi.org/10.1007/s00134-020-05980-0.
Cagle SD, Hutcherson BL, Wiley AT. Health care–associated infections: best practices for prevention. Am Family Phys. 2022;105(3):262–70.
Fass RJ, Barnishan J. In vitro susceptibilities of nonfermentative gram-negative bacilli other than Pseudomonas aeruginosa to 32 antimicrobial agents. Rev Infect Dis. 1980;2(6):841–53. https://doi.org/10.1093/clinids/2.6.841.
Reina J, Gil J, Salva F, Gomez J, Alomar P. Microbiological characteristics of Weeksella virosa (formerly CDC group IIf) isolated from the human genitourinary tract. J Clin Microbiol. 1990;28(10):2357–9. https://doi.org/10.1128/jcm.28.10.2357-2359.1990.
María A, Martínez T, Alfredo Ovalle S. Weeksella virosa. Revista Chil De Infectología. 2011;28(5):429–30. https://doi.org/10.4067/S0716-10182011000600007.
Faber MD, del Busto R, Cruz C, Mezger E. (1991). Response of Weeksella virosa peritonitis to imipenem/cilastin. Advances in peritoneal dialysis. Conference on Peritoneal Dialysis, 7, 133–134.
Boixeda D, de Luis DA, Meseguer MA, Aller R. A case of spontaneous Peritonitis caused by Weeksella virosa. Eur J Gastroenterol Hepatol. 1998;10(10):897–8. de.
Meharwal SK, Taneja N, Sharma S, Sharma M. Complicated nosocomial UTI caused by nonfermenters. Indian J Urol. 2002;18:123.
Manogaran M, Marnejon T, Sarac E. Pneumonia and sepsis due to Weeksella virosa in an immunocompromised patient. Infect Dis Clin Pract. 2004;12(5):286–7. https://doi.org/10.1097/01.idc.0000138937.36791.ae.
Lang E, Teshima H, Lucas S, Lapidus A, Hammon N, Deshpande S, Nolan M, Cheng JF, Pitluck S, Liolios K, Pagani I, Mikhailova N, Ivanova N, Mavromatis K, Pati A, Tapia R, Han C, Goodwin L, Chen A, Kyrpides NC. Complete genome sequence of Weeksella virosa type strain (9751 T). Stand Genomic Sci. 2011;4(1):81–90. https://doi.org/10.4056/sigs.1603927.
Slenker AK, Hess BD, Jungkind DL, DeSimone JA. Fatal case of Weeksella virosa Sepsis. J Clin Microbiol. 2012;50(12):4166–7. https://doi.org/10.1128/JCM.01761-12.
Toescu SM, Lacey S, Low HL. First report of postoperative intracranial Weeksella virosa Infection. Acta Neurochir. 2017;159(11):2235–8. https://doi.org/10.1007/s00701-017-3307-9.
Vaquera-Aparicio DN, Mascareñas-De Los Santos AH, Casillas-Vega N, Riojas-Hernández P, Llaca-Díaz J, Herrera-Benavente I, Castillo-Bejarano JI. Bacteremia due to weeksella virosa in a pediatric patient with embryonal rhabdomyosarcoma. Boletín Médico Del Hospital Infantil De Mexico. 2020;77(3):149–52. https://doi.org/10.24875/BMHIM.19000205.
Unalan T, Karagoz A, Bayhan C, Ozsurekci Y, Hazirolan G. An unusual case of peritoneal dialysis- associated bacterial Peritonitis caused by Weeksella virosa. Acta Microbiológica et Inmunológica Hungarica. 2019;68(1):62–4. https://doi.org/10.1556/030.66.2019.027.
Campbell IM, Congdon M, Capucilli PS, Fox WW. A not so common Infection in an extremely low-birth-weight infant. Clin Pediatr. 2020;59(11):1040–2. https://doi.org/10.1177/0009922820927031.
Holmes B, Steigerwalt AG, Weaver RE, Brenner DJ. Weeksella virosa gen. no v., sp. nov. (formerly group IIf), found in human clinical specimens. Syst Appl Microbiol. 1986;8(3):185–90. https://doi.org/10.1016/S0723-2020(86)80075-3.
Steinberg JP, Burd EM. (2014). Other Gram-Negative and Gram-Variable Bacilli. In Mandell, Douglas, and Bennett’s Principles and Practice of Infectious Diseases (Eighth Edition, Vol. 2). Elsevier Inc. https://doi.org/10.1016/B978-1-4557-4801-3.00238-1.
Mardy C, Holmes B. Incidence of vaginal Weeksella virosa (formerly group IIf). J Clin Pathol. 1988;41(2):211–4.
Funding
The authors do not have sources of financing.
Author information
Authors and Affiliations
Contributions
LAdFGP: Conception, design of the work and acquisition of data. AUMG: Translated the work to English. JEVD: Drafted the work and substantively revised it. FGMC: Analysis and interpretation of data. HAV: Substantively revised it. KAD: Drafted the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This work had the approval of the research ethics committee of the “Regional Hospital of High Specialty B, ISSSTE” from Veracruz, Mexico.
Consent for publication
Informed consent to publish this manuscript was obtained from a direct relative of the patient involved.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
de la Fuente García Peña, L., Mendoza García, A.U., Villegas-Dominguez, J.E. et al. Ventilator-associated pneumonia by Weeksella virosa: case report. BMC Infect Dis 24, 6 (2024). https://doi.org/10.1186/s12879-023-08927-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-023-08927-0