Abstract
Background
Healthcare workers (HCWs) have a higher risk of contracting coronavirus disease 2019 (COVID-19) compared to the general population due to their frontline role and direct contact with the infected patients. Accordingly, they were among the first groups to receive vaccination against COVID-19. A higher risk of COVID-19 infection may also exist among hospital staff members other than HCWs. In this study, we assessed the seroprevalence of anti-severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) IgG pre- and post-COVID-19 vaccination in hospital staff members.
Methods
This cross-sectional study included 228 staff members of Bandar Abbas Children’s Hospital, Bandar Abbas, Iran, who were recruited from 2020 to 2021. Staff members were vaccinated with vector and inactivated vaccines. Anti-SARS-CoV-2 spike protein IgG was measured in their blood samples pre- and post-COVID-19 vaccination.
Results
Of the 228 hospital staff members evaluated in this study (mean age: 37.59 ± 8.70 years), 204 (89.5%) were female and 210 (92.1%) were HCWs. Only one staff member was not vaccinated, the rest received one dose (99.6%), and 224 (98.7%) two doses. Vector vaccines were administered to 71.4% of staff members and 72.9% of HCWs. Anti-SARS-CoV-2 IgG antibody was positive in 8.8% of staff members before vaccination, 9.3% after the first dose, and 50% after the second dose. The corresponding percentages were 9.5%, 9.5%, and 48.8% in HCWs. Being a HCW was not associated with the seroprevalence of anti-SARS-CoV-2 IgG after the second dose; however, multivariable binary logistic regression analysis revealed that the interval between two vaccine doses (adjusted odds ratio [aOR] = 0.595, 95% confidence interval [CI] 0.434; 0.816, P = 0.001) and age (aOR = 1.062, 95% CI 1.021; 1.105, P = 0.003) were associated with seroprevalence.
Conclusions
After receiving a second dose of vector or inactive virus vaccines, our hospital’s staff members and HCWs had a seroprevalence of anti-SARS-CoV-2 IgG antibodies of around 50%. Seroprevalence increased with increasing age and shorter intervals between doses.
Similar content being viewed by others
Introduction
The coronavirus disease 2019 (COVID-19) outbreak initially emerged as a local epidemic in Wuhan, China in December of 2019. However, its swift spread resulted in a worldwide pandemic that affected nearly all nations and led to substantial fatalities [1, 2]. Healthcare professionals, commonly referred to as healthcare workers (HCWs), are the primary workforce responsible for providing clinical care. It is widely believed that they are at a greater risk of contracting the disease compared to the general population, given their frontline role in healthcare provision. In the event of infection, HCWs not only present a potential hazard to susceptible patients but also to their colleagues in the healthcare profession [3, 4]. Moreover, the infection’s morbidity and associated stress can result in the disturbance of patient care [5].
Vaccination is considered the most effective measure for preventing COVID-19 infection [6]. Currently, there are four main types of COVID-19 vaccines, namely mRNA vaccines (Pfizer-BioNTech, Moderna), vector vaccines (AstraZeneca, Sputnik V, Johnson & Johnson), protein subunit vaccines (Novavax), and inactivated virus vaccines (Sinopharm, Bharat, Barekat) [7].
Despite the initiation of vaccination for Iranian HCWs in March 2021, there exist a dearth of scholarly literature pertaining to the seroprevalence of anti-severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) antibodies in HCWs subsequent to vaccination. Moreover, hospital staff members other than HCWs may also be at higher risk of COVID-19 infection than the general population.The investigation of the impact of protective measures, such as vaccination, on the production of antibodies can be effectively carried out by studying HCWs. This population is particularly suitable for such research as they were among the first to receive vaccinations and are in direct contact with patients infected with SARS-CoV-2.
we aimed to investigate the seroprevalence after the second round of vaccination of administrative and non-administrative personnel in order to investigate the effect of the second round of vaccine injection on the IgG antibody level against SARS-CoV-2. We measured the seroprevalence of IgG antibody against SARS-CoV-2 in the personnel of Bandar Abbas Children’s Hospital to reduce the lack of information about the effectiveness of the vaccine in hospital personnel.
Methods
Trial design and oversight
A descriptive-cross sectional study was conducted at the Children’s Hospital in Bandar Abbas (located in Hormozgan province in southern Iran) to investigate the seroprevalence of anti-SARS-CoV-2 antibodies among hospital staff. For this purpose, we obtained ethical approval from the ethics committee of the Hormozgan University of Medical Sciences. Hospital staff at the Children’s Hospital in Bandar Abbas who were employed between March 2020 and March 2021 were included in the study, and samples were sent to the hospital’s own laboratory center. Seroprevalence of IgG antibodies before and after vaccination was measured along with demographic information.
Trial participants
All Healthcare workers (HCWs), service and administrative staffs (non- HCWs) that employed at the Children’s Hospital in Bandar Abbas between 2020 and 2021 were eligible to participate in the study. Each individual was reviewed after obtaining written consent to participate in the study. Totally, 228 personnel were investigated. General information including age, gender, occupation, history of contact with a COVID-19 patient in the family, underlying diseases, and history of COVID-19 vaccination was obtained using a checklist developed under the supervision of infectious disease experts at the Children’s Hospital. Written consent was obtained from each individual prior to their review. A venous blood sample was taken from each person to measure their IgG antibody titers against SARS-CoV-2.
The following variables were also evaluated and recorded for all subjects:
-
Occupation (HCW, non-HCW);
-
Workplace (COVID wards, non-COVID wards).
-
Underlying diseases (chronic pulmonary disease, cardiovascular disease, hypertension, diabetes, immunosuppression);
-
Vaccine type and number of doses;
-
The interval between the two vaccine doses;
-
History of previous COVID-19 infection.
Trial procedures and outcomes
A 3 cc blood sample was taken from each individual according to clinical and laboratory standards. The samples were transferred to a laboratory located in the hospital using a specialized container with ice. The samples were kept in a refrigerator for a maximum of 48 h before measuring their IgG antibody titers using the enzyme-linked immunosorbent assay (ELISA) method with the Euroimmune kit. Prior to receiving the vaccine and two weeks after receiving the first and second doses, each individual was evaluated for IgG antibodies.
The interval between the two vaccine doses depended on the type of vaccine, which is why the hospital staff were followed up through the vaccination program. After receiving the first dose, they were contacted, and then two weeks later, samples were taken. When receiving the second dose, confirmation was obtained via telephone. Finally, all staff received their second dose by March 2021, and two weeks after second dose, their IgG were assessed.
Statistical analysis
Sampling method was census and descriptive statistics methods were used. The data analysis was conducted using the SPSS software (version 26.0). The statistical measures of mean and standard deviation were employed to describe continuous variables. Categorical variables were described using frequencies and percentages. Binary logistic regression analysis was applied to determine the factors associated with the seroprevalence of anti-SARS-CoV-2 IgG antibody. Accordingly, crude odds ratio (cOR), adjusted OR (aOR), and 95% confidence intervals (Cis) were reported. Statistical significance was determined by considering P-values less than 0.05.
Results
Of the 228 hospital staff members evaluated in this study (mean age: 37.59 ± 8.70 years), 204 (89.5%) were female and 24 (10.5%) were male. Table 1 represents the general characteristics of the study participants. The majority of staff members were HCWs (92.1%) and worked in non-COVID wards (88.2%).
Only one staff member was not vaccinated, the rest received one dose (99.6%), and 224 (98.7%) received two doses. Vector vaccines were administered to 162/227 staff members (71.4%) as the first dose and to 160/224 (71.4%) as the second dose. All the 210 HCWs received vaccination, but only 207 (98.6%) received the second dose. Vector vaccines were administered to 153/210 HCWs (72.9%) as the first dose and to 151/207 (72.9%) as the second dose.
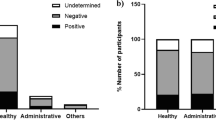
The mean interval between the two vaccine doses was 1.60 ± 1.11 month. Anti-SARS-CoV-2 IgG antibody was positive in 8.8% (20/228) staff members before vaccination, in 9.3% (21/227) after the first dose, and in 50% (112/224) after the second dose (Fig. 1a). On the other hand, Anti-SARS-CoV-2 IgG antibody was positive in 9.5% (20/210) HCWs before vaccination, in 9.5% (20/210) after the first dose, and in 48.8% (101/207) after the second dose (Fig. 1b).
After the first dose, Seroconversion rates were highest with seroprevalence in AstraZeneca, while in the second stage, more seroprevalence was allocated to the Barekat (an Inactivated Iran-made vaccine that was available in the second dose of the vaccination program). Sinopharm shows a 63% increase in the second dose compared to the first dose. The difference between the seroconversion rates of the AstraZeneca vaccine between the first and second doses has significantly decreased, with the lowest amount of seroprevalence in the second dose. Bharat vaccine shows a tenfold growth in the second dose. Although Sputnik has grown compared to the first dose, it is less than the growth rate of Bharat vaccine. (Fig. 2).
Multivariable binary logistic regression analysis revealed that with every one-month increase in the interval between the two vaccine doses, the odds of positive anti-SARS-CoV-2 IgG (compared to negative IgG) decreased by almost 40% (aOR = 0.595, 95% CI 0.434; 0.816, p < 0.05). Also, every one-year increase in age increased the odds of positive anti-SARS-CoV-2 IgG by 6% (aOR = 1.062, 95% CI 1.021; 1.105, p < 0.05). However, being a HCW was not associated with the seroprevalence of anti-SARS-CoV-2 IgG (Table 2).
Discussion
We assessed the seroprevalence of anti-SARS-CoV-2 spike protein IgG antibodies among the staff members of a children’s hospital and found that pre-vaccination, seroprevalence was 8.8% in all staff members and 9.5% in HCWs. After receiving the first vaccine dose, seroprevalence increased to 9.3% in all staff members but remained unchanged in HCWs (9.5%). After the second vaccine dose, seroprevalence considerably increased to 50% in all staff members and 48.8% in HCWs.
Assaid et al. reported a seroprevalence of 65.9% by Euroimmun ELISA five months after the second dose of vector or inactivated virus vaccines in HCWs. The antibody response did not differ significantly between HCWs who received either vaccine type [8], which is consistent with our results, showing no relationship between vaccine type and seroprevalence by adjusted logistic regression analysis. The higher seroprevalence in Assaid et al.’s study can be justified by demographic and anthropometric differences and history of prior COVID-19 infection as none of the HCWs in Assaid et al.’s study had a history of COVID-19 infection [8]. A small group of our subjects were previously infected with COVID-19, but we found no association between such history and anti-SARS-CoV-2 IgG seroprevalence. Nonetheless, a single dose of the vaccine may be sufficient to induce an effective response in previously infected individuals, suggested by Gobbi et al. [9]
Interestingly, the seroprevalence of anti-SARS-CoV-2 after two doses of vector vaccines was 91.7% in HCWs of the study by Elangovan in India. They also observed a significant increase in antibody levels of HCWs who had a history of COVID-19 infection within six months prior to vaccination [10]. The much lower seroprevalence in our study might be due to almost one-third of subjects receiving inactivated virus vaccines, the interval between two doses of vaccines, as well as demographic differences and work settings. More importantly, the accuracy of measurements is always a matter of concern when evaluating laboratory parameters
Another explanation for the higher seroprevalence in Assaid et al.’s study [8] can be the time of antibody assessment. We evaluated anti-SARS-CoV-2 antibodies at least two weeks after the second vaccine dose while their measurements were done five months after the second dose. The two-week interval was chosen in our study because according to previous investigations, individuals vaccinated at least 14 days before antibody measurements were presumed to be seronegative [11]. However, Costa et al. reported higher antibody values with shorter time lapse around two to eight weeks between vaccination and serology [12]
Another finding of the present study was the positive correlation of age with anti-SARS-CoV-2 IgG seroprevalence after the second dose of vaccination as every one-year increase in age increased the odds of positive anti-SARS-CoV-2 IgG by 6%. Yet, the oldest subject in our study was 60 years old. Contrary to our findings, by studying antibody responses in 212,102 individuals, Ward et al. showed a decrease in antibody response with age, but this reduction was most prominent at ages 75 years and above [13]. On the other hand, we found no association between sex and seroprevalence. Conversely, Costa et al. reported lower serological levels in males [12]. A lower antibody response to mRNA vaccines has been demonstrated in men compared to women in other studies [14, 15]. Of note, although vaccine type did not influence seroprevalence in our study, none of the subjects received mRNA vaccines
We found that a longer interval between the two doses of vaccines was associated with a lower seroprevalence of anti-SARS-CoV-2 IgG antibodies. On the contrary, it has been demonstrated that a three-month interval between the primary vaccine dose and the booster might result in a better immune response compared to a short dose interval, when vector vaccines were concerned [16]
In the current study, neither univariable nor multivariable binary logistic regression analysis showed an association between BMI and seroprevalence of anti-SARS-CoV-2 IgG antibodies after the second dose of vaccination. Obesity can negatively affect the immune system, and vaccine uptake may differ based on BMI. However, in line with our findings, the current COVID-19 trials have shown no difference between groups with normal and obese BMIs in terms of vaccine efficacy [17]. Similarly, no association between BMI and serological response has been reported in cohorts and cross-sectional studies [12, 18, 19]. Contrarily, Pellini et al. have reported that immunogenicity of SARS-CoV-2 vaccine may be impaired by obesity [20]. Consequently, it is necessary to conduct further studies to better understand whether the long-term effectiveness of COVID-19 vaccination depends on individuals’ BMI.
Understanding the immunological reaction that generates a protective immunization to SARS-CoV-2 is crucial [21]. In comparison to the membrane, envelope, and nucleocapsid proteins, antibody responses to the spike protein are considered to be the predominant focus of neutralizing activity during viral infection [22, 23]. However, it is important to note that only a proportion of anti-SARS-CoV-2 spike protein IgG antibodies have neutralizing capacity, and no neutralization assays were performed in the current study. Therefore, the seroprevalence of anti-SARS-CoV-2 spike protein IgG antibodies may not accurately reflect the neutralizing effects of vaccines. It has been demonstrated that declining levels of neutralizing antibodies are associated with an increased risk of symptomatic infection, although the relationship is less clear for severe infections [24]
The current investigation had some limitations. The association between seroprevalence and the number of vaccine doses could not be evaluated since only those staff members who received the second vaccine dose were tested again for anti-SARS-CoV-2 IgG. Moreover, although we took prior COVID-19 infection into account, it is not clear how long ago the infection occurred. This is important because IgG titer attenuates over time. Also, we did not assess neutralizing antibodies and cell-mediated immune responses
Conclusions
The seroprevalence of anti-SARS-CoV-2 IgG was around 50% in our children’s hospital staff members and HCWs after the second vaccination with vector or inactive virus vaccines. Contrary to previous studies, higher age and lower between-dose intervals led to increased seroprevalence. Despite the results of several studies in this regard, there is a need for further investigations to determine the seroprevalence of anti-SARS-CoV-2 IgG, especially in Iran, because the employed vaccine types are quite different from many other countries
Data Availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Cucinotta D, Vanelli M. WHO declares COVID-19 a pandemic. Acta Bio Medica: Atenei parmensis. 2020;91(1):157.
Ciotti M, Ciccozzi M, Terrinoni A, Jiang W-C, Wang C-B, Bernardini S. The COVID-19 pandemic. Crit Rev Clin Lab Sci. 2020;57(6):365–88.
Sim MR. The COVID-19 pandemic: major risks to healthcare and other workers on the front line. BMJ Publishing Group Ltd; 2020. pp. 281–2.
Pittet LF, Messina NL, Orsini F, Moore CL, Abruzzo V, Barry S, et al. Randomized Trial of BCG Vaccine to protect against Covid-19 in Health Care workers. N Engl J Med. 2023;388(17):1582–96.
Gupta N, Dhamija S, Patil J, Chaudhari B. Impact of COVID-19 pandemic on healthcare workers. Ind Psychiatry J. 2021;30(Suppl 1):282–s4.
Soleimanpour S, Yaghoubi A. COVID-19 vaccine: where are we now and where should we go? Expert Rev Vaccines. 2021;20(1):23–44.
Barouch DH. Covid-19 vaccines—immunity, variants, boosters. N Engl J Med. 2022;387(11):1011–20.
Assaid N, Arich S, Charoute H, Akarid K, Ezzikouri S, Maaroufi A, Sarih M. Anti-SARS-CoV-2 antibody responses 5 Months Post Complete Vaccination of Moroccan Healthcare Workers. Vaccines. 2022;10(3):465.
Gobbi F, Buonfrate D, Moro L, Rodari P, Piubelli C, Caldrer S, et al. Antibody response to the BNT162b2 mRNA COVID-19 vaccine in subjects with prior SARS-CoV-2 Infection. Viruses. 2021;13(3):422.
Elangovan D, Hussain SMS, Virudhunagar Muthuprakash S, Devi Periadurai N, Viswanath Nalankilli A, Volvoikar H, et al. Impact of COVID-19 vaccination on Seroprevalence of SARS-CoV-2 among the Health Care Workers in a Tertiary Care Centre, South India. Vaccines. 2022;10(11):1967.
Soeorg H, Jõgi P, Naaber P, Ottas A, Toompere K, Lutsar I. Seroprevalence and levels of IgG antibodies after COVID-19 Infection or vaccination. Infect Dis. 2022;54(1):63–71.
Costa C, Migliore E, Galassi C, Scozzari G, Ciccone G, Coggiola M, et al. Factors influencing level and persistence of anti SARS-CoV-2 IgG after BNT162b2 vaccine: evidence from a large cohort of healthcare workers. Vaccines. 2022;10(3):474.
Ward H, Whitaker M, Flower B, Tang SN, Atchison C, Darzi A, et al. Population antibody responses following COVID-19 vaccination in 212,102 individuals. Nat Commun. 2022;13(1):907.
Nomura Y, Sawahata M, Nakamura Y, Kurihara M, Koike R, Katsube O, et al. Age and Smoking predict antibody titres at 3 months after the second dose of the BNT162b2 COVID-19 vaccine. Vaccines. 2021;9(9):1042.
Salvagno GL, Henry BM, Di Piazza G, Pighi L, De Nitto S, Bragantini D, et al. Anti-SARS-CoV-2 receptor-binding domain total antibodies response in seropositive and seronegative healthcare workers undergoing COVID-19 mRNA BNT162b2 vaccination. Diagnostics. 2021;11(5):832.
Voysey M, Clemens SAC, Madhi SA, Weckx LY, Folegatti PM, Aley PK, et al. Single-dose administration and the influence of the timing of the booster dose on immunogenicity and efficacy of ChAdOx1 nCoV-19 (AZD1222) vaccine: a pooled analysis of four randomised trials. The Lancet. 2021;397(10277):881–91.
Kipshidze N, Kipshidze N, Fried M. COVID-19 vaccines: special considerations for the obese population. Obes Surg. 2021;31(8):3854–6.
Pellini R, Venuti A, Pimpinelli F, Abril E, Blandino G, Campo F, et al. Initial observations on age, gender, BMI and Hypertension in antibody responses to SARS-CoV-2 BNT162b2 vaccine. EClinicalMedicine. 2021;36:100928.
Watanabe M, Balena A, Tuccinardi D, Tozzi R, Risi R, Masi D, et al. Central obesity, smoking habit, and Hypertension are associated with lower antibody titres in response to COVID-19 mRNA vaccine. Diab/Metab Res Rev. 2022;38(1):e3465.
Pellini R, Venuti A, Pimpinelli F, Abril E, Blandino G, Campo F et al. Obesity may hamper SARS-CoV-2 vaccine immunogenicity. MedRXiv. 2021:2021–02.
Suthar MS, Zimmerman MG, Kauffman RC, Mantus G, Linderman SL, Hudson WH, et al. Rapid generation of neutralizing antibody responses in COVID-19 patients. Cell Rep Med. 2020;1(3):100040.
Bolles M, Donaldson E, Baric R. SARS-CoV and emergent coronaviruses: viral determinants of interspecies transmission. Curr Opin Virol. 2011;1(6):624–34.
Deming D, Sheahan T, Heise M, Yount B, Davis N, Sims A, et al. Vaccine efficacy in senescent mice challenged with recombinant SARS-CoV bearing epidemic and zoonotic spike variants. PLoS Med. 2006;3(12):e525.
Khoury DS, Cromer D, Reynaldi A, Schlub TE, Wheatley AK, Juno JA, et al. Neutralizing antibody levels are highly predictive of immune protection from symptomatic SARS-CoV-2 Infection. Nat Med. 2021;27(7):1205–11.
Acknowledgements
Our sincere gratitude goes out to the Clinical Research Development Center of Children’s Hospital, Bandar Abbas, Iran for all their assistance.
Funding
No funding was received.
Author information
Authors and Affiliations
Contributions
Conceptualization and study validation: M.T and H.M. Implementation: F.H and M.T.d. Supervision: M.T. Data analysis and interpretation: H.M and M.T.D. Writing and reviewing: M.T and F.H. All authors have read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The research obtained ethical clearance from the Ethics Committee of Hormozgan University of Medical Sciences (IR.HUMS.REC.1401.109) and conforms to the principles outlined in the Declaration of Helsinki. All participants provided written informed consent prior to their involvement in the study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Tariverdi, M., Mohammadi, H., Hassanzadeh, F. et al. Seroprevalence of anti-SARS-CoV-2 IgG antibodies pre- and post-COVID-19 vaccination in staff members of Bandar Abbas Children’s Hospital. BMC Infect Dis 24, 253 (2024). https://doi.org/10.1186/s12879-023-08863-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-023-08863-z