Abstract
Background
A novel corona virus called SARS-CoV-2 was identified at the end of December 2019, and the illness induced by it was designated as coronavirus disease 2019 (COVID-19). Severity of the disease could vary significantly since most of the infected individuals experience mild to moderate respiratory symptoms and recover without specialized care. Genetic polymorphisms have implications in influencing the varying degrees of COVID-19 severity. This study aims to assess the potential association between the CXCL12 rs2839693 polymorphism and the severity of COVID-19 in Assiut University Quarantine Hospital during the period from May 2022 to August 2022.
Methods
The present study is a cross-sectional study and is applied to 300 COVID-19 patients confirmed by RT-PCR admitted to Assiut University Quarantine Hospital from May 2022 to August 2022. Based on the clinical symptoms, the recruited participants had been divided into two groups. Group I involved mild or moderate cases; Group II involved severe or critical conditions. The rs2839693 polymorphism was detected by real time PCR using TaqMan assay probe.
Results
The frequency of the T allele and the TT genotype was significantly higher in the severe or critical group compared with the mild or moderate group (p value < 0.001). C-reactive protein (CRP) and D-dimers are significantly elevated in the combined variants (CT + TT) and the TT compared with the CC (P value 0.006 and 0.017 respectively) and the CC,CT genotypes (p value 0.019 and 0.002 respectively). The combined variants (CT + TT) of CXCL12 were found to be independent predictors to severe or critical COVID-19 risk with P value = < 0.001, OR = 3.034& 95% CI = 1.805–5.098.
Conclusion
Our findings revealed that CXCL12 rs2839693 had a role in the development and seriousness of COVID-19. Patients with the TT genotype or the T allele at increased risk developed severe or critical rather than mild or moderate disease.
Similar content being viewed by others
Introduction
A novel corona virus called severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) was identified at the end of December 2019, and the illness induced by it was designated as coronavirus disease 2019 (COVID-19) [1].
Most patients infected with SARS-CoV-2 do not exhibit any symptoms, yet occasionally mild or moderate symptoms may appear [2].
Genetic variations in SARS-CoV-2 may develop mutant forms that are distinct from the original strains. Only just few variants in SARS-CoV-2 were considered as "variants of concern" (VOCs) by the World health Organization (WHO). According to the WHO's most current epidemiological report, five SARS-CoV-2 VOCs (Alpha, Beta, Gamma, Delta, and Omicron) have just been detected since the epidemic began on December 11, 2019 [3].
Under the guidance of the WHO, Egypt has developed a persuasive care strategy to address the COVID-19 pandemic. The country's comparatively lower infection rates, including factors like high temperatures, high levels of humidity, early Bacille Calmette-Guérin (BCG) vaccine usage, may be a distinct virus strain. In addition, it describes the situation and the preventative steps the nation has made to deal with the pandemic [4].
Vulnerability to SARS-CoV-2, depends on many factors such as genetic polymorphisms which studied in the following: transmembrane protease serine 2 (TMPRSS2), tumor necrosis factor-alpha (TNF-α), interferon-gamma (IFN-γ), the ABO blood type, and angiotensin-converting enzyme II (ACE2) [5].
Chemokines, belonging to cytokine superfamily, are proteins with low-molecular-weight. They stimulate the movement of immune cell by attaching to immune cells surface receptors. Chemokines can be categorized into four subfamilies: CC, CXC, XC, and CX3C [6].
Numerous chemokines are involved in various viral diseases including hepatitis B virus, influenza virus, human immunodeficiency virus, respiratory syncytial virus, and hepatitis C virus. Besides, coronaviruses comprises SARS-CoV-2 [7].
Chemokine synthesis during viral infection is a crucial step in guiding immune cells to the infection site where the virus is present. However, excessive immune cell targeting results in severe inflammation trigger the acute respiratory distress syndrome (ARDS), a frequent COVID-19 consequence. Chemokine control is a crucial part in managing viruses. Increasing understanding of the chemokine profile in COVID-19 could improve our knowledge of the immune-pathological pathways of SARS-CoV-2 infection [8].
The CXCL12, also known as stromal cell-derived factor-1 (SDF-1), rs2839693 variant is reported in many diseases including HIV-1 [9], Pulmonary tuberculosis [10], breast cancer [11], and coronary artery disease [12].
A variety of immune cells, fibroblasts, and epithelial cells produce CXCL12 are found on human chromosome 10q11.1 [11]. As opposed to the exon that codes for the functional protein, the rs2839693 SNPs are intron_variants [13].
This study aimed to assess the potential association between the CXCL12 rs2839693 polymorphism and the severity of COVID-19 in Assiut University Quarantine Hospital in the period from May 2022 to August 2022.
Materials and methods
Study design and participants
Our current research is a cross-sectional investigation administered on 300 adult Egyptian patients diagnosed with COVID-19. These patients incorporated to Assiut University Quarantine Hospital outpatient clinics, inpatient departments and intensive care units (ICU) during the period from May 2022 to August 2022.The diagnosis of COVID-19 depended on reverse transcription polymerase chain reaction (RT-PCR) of nasal or pharyngeal swabs positive result, according to the guidelines of WHO [14]. The participants were subjected to a full history taking, appropriate clinical examination and laboratory investigations which included complete blood count, arterial blood gases, ferritin, C-reactive protein (CRP) and D-dimer. The incorporated patients were classified into 2 groups depending on clinical signs: group I with mild or moderate individuals; Group II with severe or critical individuals [15]. Patients who encountered exclusion criteria were isolated from our study: HIV-1 2, Systemic lupus erythematosus, autoimmune disease, Celiac disease, Cancer, Neurological disorders, chronic obstructive pulmonary disease (COPD), and Asthma.
Study variables
The onset time was defined as the day on which individuals developed any symptoms. The degree of COVID-19 severity was estimated by using the guidelines of WHO for SARS-CoV-2 diagnosis and treatment. Mild or moderate patients without dyspnea showed SpO2 ≥ 94%. The presence of one or more of the following characteristics was considered as a severe or critical case: (a) a SpO2 of less than 93% at rest; (b) a respiratory rate of more than 30 breaths per minute; and (c) an oxygenation index of less than 300 mm Hg (artery partial pressure of oxygen/inspired oxygen fraction, PaO2/FiO2) [15].
All individuals underwent chest computed tomography (CT) scans since pulmonary lesions cannot be ruled out by a normal chest X-ray, particularly in patients with no symptoms and moderate instances.
Sample size calculation
According to Takazawa & Morita, 2020 the sample size could be calculated from the following equation [16].
n = sample size, Z a/2 (The critical value that divides the central 95% of the Z distribution), ZB (The critical value that divides the central 20% of the Z distribution), p1 = Level in group I, p2 = Level in group II, q = 1-p.
This study is based on the work of Belperio et al., 2004. The sample size was calculated using Epi Info STATCALC using the following assumptions:—95% two-sided confidence level, with an 80% power. With a 5% margin of error, the odds ratio estimated was 1.115. The ultimate sample size calculated from the Epi- Info output was 140 [17].
Specimen collection
Two ml of venous blood were obtained from all COVID-19 participants by a sterile venipuncture in a vacutainer tube containing EDTA as an anticoagulant for real-time PCR investigation of rs2839693 polymorphism in the CXCL12 gene; sample was kept frozen at -20 °C until DNA extraction.
Genotyping assay
DNA extraction
Patients with COVID-19 had their genomic DNA extracted from EDTA peripheral blood by using the Genomic DNA Purification Kit supplied by Thermo Fisher Scientific according to Whole Blood Genomic DNA Purification Main Protocol. Catalog number: K0512.
Genotyping of CXCL12 rs2839693
DNA was amplified using the Genotyping TaqPath 1-Step Multiplex Master Mix from Thermo Fisher (Cat. No. A28521). The steps in the amplification process were as follows: Enzyme activation for 10 min at 95 degrees, followed by 35 cycles of denaturation for 15 s at 95 degrees, annealing for 1 min at 60 degrees, and elongation for 1 min at 72 degrees. The context sequence [VIC/FAM]: GAAGGGGACGACAGGATGCTCTAGG[C/T]ACCTGGGGAGGGGAGAATGGAGAGC was utilised using the TaqMan ready-made SNP assay (Thermo Fisher; Catalogue no. 4351379). A 20 μL PCR mixture was comprised of 3μL extracted DNA, 0.5μL SNP assay, 5μL Master Mix, and 11.5μLdistilled water was carried out. The Applied Biosystems 7500 real-time polymerase chain reaction (real time PCR) apparatus was used.
Statistical analyses
With the use of the IBM SPSS software package version 20.0, data were inputted into the computer and analyzed [18]. Numbers and percentage were used to describe qualitative data. The normality of the distribution was examined using the Kolmogorov–Smirnov test. Utilizing range (minimum and maximum), mean, and standard deviation, quantitative data were reported. At the 5% level, significance of the results was determined. The first test, the Chi-square test, was employed to compare various groups for categorical variables. The second test, Student t-test, was employed to compare two examined groups for typical quantitative variables. The third test, Mann Whitney test, was employed to compare two investigated groups in order to compare unusual quantitative variables. The risk factors for clinical course in patients were determined using multivariable logistic regression analysis and presented as odds ratios and 95% Cis.
Results
Demographic and clinical characteristics of COVID-19 patients
Table 1 shows the demographic and clinical features of COVID-19 patients. In this cross-sectional study, we included 300 COVID-19 patients. Their ages ranged between 36 and 85 years, with a median age of 66 years. The patients' gender ratio was 56.3% male and 43.7% female. Most of patients were non-smokers and vaccinated. Hypertension was the most frequent comorbid disease while fatigue and dry cough were the most frequent symptom.
Physical examination, laboratory evaluation, and CT findings of COVID-19 patients
Our data showed that lymphocyte count in most cases was within the normal values, while lymphopenia was detected in 84 (28.0%) of COVID-19 patients. Ferritin, cell reactive protein (CRP), and D-dimers were elevated in most cases. Regarding CT findings, our results revealed that bilateral ground glass opacity (GGO) was the most frequent CT abnormality (Table 2).
Treatment and outcomes of COVID-19 patients
According to Table 3, most patients received antibiotic and antiviral treatment. A large proportion of patients did not need oxygen therapy while, mask oxygen was needed in half of the patients. Outcomes showed that the percentage of patients who needed home management was equal to those needed hospitalization without intensive care unit (ICU); while around half of the patients admitted to ICU, and 39 (13.0%) patients died. Duration of ICU stay ranged between 1.0–13.0 days with a median value 7.0 days. The median duration of in-hospital stay was 7.0 days and a range (1.0–15.0) days. Duration of recovery ranged between 2.0–48.0 days with median value 15.0 days.
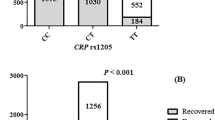
Genetic findings of CXCL12 rs2839693 for COVID-19 patients
Table 4 shows a highly statistical significant difference between mild or moderate and severe or critical groups regarding allelic and genotyping frequencies (p value < 0.001). The frequency of the TT genotype and the T allele were higher in the severe or critical group than in the mild or moderate group. Regarding genotypes, patients with the CT + TT genotype had 3.08 higher risks to develop severe or critical COVID-19 than the CC genotype. Regarding alleles, patients with the T allele had 2.91 higher risks to develop severe or critical COVID-19 than the C allele.
Multivariate logistic regression analysis showed that the combined variants (CT + TT) of CXCL12 were found to be independent predictors to severe or critical COVID-19 risk with P value = < 0.001, OR = 3.034& 95% CI = 1.805–5.098 (Table 5).
Patient demographic data, comorbidity, and symptoms according to CXCL12 rs2839693 genotypes
Subsequently, we compared demographic data, comorbidity, and symptoms between CXCL12 genotypes (CC vs. CT + TT and CC vs. CT vs. TT) as presented in Table 6. Significant associations of genotypic distributions with dyspnea, vomiting, and dysarthria of COVID-19 patients were detected (P value < 0.001, 0.015, and < 0.001 respectively). Dyspnea was more prevalent in the combined CT + TT and the TT genotypes compared with the CC and the CT, CC genotypes, respectively. Vomiting and Dysarthria were significantly prevalent in the TT genotype compared with the CT, CC genotypes. Regarding clinical course of the disease, we found that severe or critical illness was associated with the combined CT + TT and the TT genotypes where it was more prevalent in the combined CT + TT, and the TT genotypes was compared with the CC and the CT, CC genotypes, respectively.
Laboratory evaluation and CT findings according to CXCL12 rs2839693 genotypes
Table 7 shows statistical significant differences between genotypes, regarding CRP, D-dimers, and ferritin. Where CRP and D-dimers were significantly elevated in the combined CT + TT, and the TT was compared with the CC (P value 0.006 and 0.017 respectively) and the CC, CT genotypes (p value 0.019 and 0.002 respectively); while Ferritin was significantly elevated in the TT compared with the CC, CT genotypes (P value 0.050).
Treatment and outcomes according to CXCL12 rs2839693 genotypes
As indicated in Table 8, a significant difference between genotypes regarding clexane as a treatment was detected (P value 0.022). Clexane was more prevalent in the TT genotype than the CC and CT genotype. The number of patients without any demand for oxygen therapy was significantly different between the genotypes (P value < 0.001) where it was more prevalent in the CC genotype compared with the combined CT + CC and the TT genotypes. Nasal cannula and invasive mechanical ventilation were more prevalent in the TT and the combined CT + TT genotypes compared with the combined CC, CT and the CC genotypes, respectively, (P value < 0.001 and 0.002 for nasal cannula, 0.025 and 0.031 for invasive mechanical ventilation). Mask oxygen was used more prevalently in patients of the CT + TT genotypes than those of the CC genotype (P value 0.044).
The number of patients needed home management was significantly higher in the CC genotype compared with the combined CT + TT and the TT genotypes (P value 0.002 and 0.006 respectively). The need for ICU stay was significantly higher in patients with the combined CT + TT and the TT genotype compared with CC and CC, CT, respectively, (P value < 0.001 and < 0.001 respectively). Regarding mortality rates, our results revealed that they were significantly higher in the combined CT + TT and the TT genotype compared with the CC and the CC, CT, respectively (P value 0.026 and < 0.001 respectively).Patients with the TT genotype had a longer duration of in-hospital stay than patients with the CC genotype (median, 12.0 days, as compared with 7.5 days; P value 0.035).
Discussion
Numerous investigations have been carried out since the COVID-19 tragedy first emerged in order to comprehend the disease's mechanics and determine the cause of the variation in symptoms across patients. Because of their importance in the cytokine storm and the onset of ARDS, chemokines and their receptors were among the most significant elements that were researched in this context. Therefore, it may be possible to forecast the results of COVID-19 by fully comprehending the signature of chemokines and their receptors. Therefore, we proposed that CXCL12 could influence the results and severity of COVID-19.
Our present research examined 156 mild or moderate and 144 severe or critical COVID-19 patients at Assiut University Quarantine Hospital from a cross-sectional perspective view.
Most of our participants were vaccinated (69.3% compared with 30.7% non-vaccinated patients) and non-smokers (60.7% compared with 39.3% smokers). Hypertension and DM were the most common co-morbid diseases found in 35.7% and 26.0% patients respectively; while renal disease, heart disease, and thyroid disease were less frequent. These findings agree with a study by Petrakis et al., who reported that the most frequent comorbid diseases were hypertension in 38.4% patients and DM in 20.9% patients [19].
Additionally, regarding clinical manifestations of the studied groups, The principal COVID-19's clinical complaints were fatigue (55.0%), dry cough (53.7%), and dyspnea (48.0%).These findings are similar to those by Rodriguez-Morales et al., who reported that the principal COVID-19's clinical complaints were cough(57.6), and dyspnea (45.6); in contrast to our results fatigue (29.4%) [20].
Regarding laboratory assessment, lymphocytes values in most cases 185 (61.7%) were typically within the normal values between (1.0–4.0 × 109/L), while lymphopenia was observed in 84 (28.0%) patient. Ferritin and CRP were elevated in most cases 200 (66.7%) and 250 (83.3%), respectively. Moreover, D-dimers were elevated in 180 (60.0%) of our cases. Our results in agree with Kadhim et al., and Smail et al., who observed lymphopenia, elevated CRP, ferritin, and D-dimers among COVID-19 patients [21, 22].
Bilateral GGO was the most frequent CT abnormality 205 (68.3%). Pneumonic consolidation was another prevalent CT characteristic in COVID-19 patients 107 (35.7%). These findings are similar to a meta-analysis research conducted on 13 previous studies and concluded that GGO was the principal CT findings followed by consolidation in COVID-19 patients [23].
Most of our participants received antibiotic as a treatment 288 (96.0%) patients; while 323 (77.3%) and 176 (58.7) patients received antiviral and Glucocorticoids, respectively. Oxygen therapy was needed in 227 (75.7%) patients: nasal cannula in 78 (26.0%), Mask oxygen in 150 (50.0%), and Invasive mechanical ventilation in 18 (6.0%). A meta-analysis study by Langford et al., on the use of antibiotic therapy on COVID-19 found that the frequency of antibiotic therapy was 74.6% [24].
The average length of hospitalization was 7.0 days. These findings agree with Alwafi et al., who indicated that the average length of hospitalization was 6.0 days [25]. While the median duration of ICU stay was 7.0 days. In contrast to our results, López-Cheda et al., indicated that the median duration of ICU stay was 14.0 days [26].
The median duration of recovery was 15.0 days. Our data agree with SeyedAlinaghi et al., who found that the median length of recovery was 13.5 days [27]. Regarding mortality rate, our data revealed that 39 (13.0%) died. These results agree with data collected from 20 regions in Italy by Immovilli et al., and revealed that the mortality rate ranged between 3.1% and 16.7% [28].
The frequency of the TT genotype and the T allele of CXCL12 rs2839693 was significantly different between mild or moderate and severe or critical patients. The frequency of the TT genotype and the T allele was higher in the severe or critical group than in the mild or moderate which may indicate the role of CXCL12 rs2839693 in the pathogenesis and severity of COVID-19. Patients with the TT genotype or the T allele at increased risk developed severe or critical rather than mild or moderate one. Our result agree with Mohamed et al., who reported no differences in the frequency of the TT genotype or the T allele of CXCL12 rs2839693 among ITP patients and controls, and that there is no correlation between this SNP and disease severity [13].
Normal CXCL12 is the only ligand that could bind to CXCR4 receptor. SARS-CoV-2 acts as a competitor for CXCL12 on CXCR4 receptor. The reason for why patients with TT genotype possess a severe form of the disease may be due to the impact of the polymorphisms on CXCL12 that makes it works dysfunctionaly. So, it keeps the way clear for SARS-CoV-2 to bind CXCR4 as a co-receptor leading to increase viral load and disease severity.
CXCL12 has a function in inflammation resolution, for example, by increasing angiogenesis and tissue repair. Prolonged CXCL12 activity may not only improve leukocyte chemotaxis, which is advantageous, but it may also worsen the chronic inflammation identified in COVID-19 [29]. CXCL12 expression rises with autoimmune disorders. CXCL12 levels are raised in individuals with a range of inflammatory illnesses, indicating that CXCL12 plays a role in autoimmunity [30].
The expression of CXCL12 is elevated in the Fibroblasts from severe COVID-19 patients which may help to attract immune cells with the CXCR4 receptor, such as macrophages, T cells, and NK cells [31]. Previous studies have found higher levels of CXCL12 in the blood of severe COVID-19 patients hospitalized in critical care units when compared to hospitalized patients with mild to moderate illness and/or healthy controls [32].
CXCL12 gene polymorphisms might influence the regulation of ACE2, the receptor used by the SARS-CoV-2 virus to enter human cells. Altered ACE2 expression or function could impact viral entry and disease progression. Patients with severe COVID-19 have much higher levels of ACE2 expression, which allows more viral invasiveness [33].
Gene polymorphisms in CXCL12 might lead to differences in immune cell recruitment and activation, which could affect the immune response to the virus and the development of severe COVID-19. Effective hematopoiesis, homing of T and memory B cells to lymph nodes, and monocyte recruitment depend on CXCL12, the CXCR4 ligand. Several viruses employ the inhibition of this axis to reduce the number of circulating immune cells and raise their own proliferative rate [32].
CXCL12 polymorphisms could potentially impact the ability to clear the virus from the body, affecting the duration and severity of COVID-19. Cellular clearance of the virus depends on the production of virus-specific antibodies, which block the entry of free virions into uninfected cells, opsonize the virus for inactivation by complementing proteins or elimination by phagocytic immune cells that contain CXCL12 receptor like macrophages and neutrophils. They also inactivate or start the killing of infected cells by activating the complement cascade and through antibody-mediated cytotoxicity processes, essential for [34].
Elimination of SARS-CoV-2 results in either an earlier time of recovery or a decrease in the severity of disease. According to Zheng, F. et al., the removal of viral shedding after viral clearance in patients would also aid to lessen viral transmission [35].
In agreement of our data Wang et al., found that patients with CXCL12 rs2839693 were associated with increased susceptibility to sepsis [36]. Zhang et al., conducted a study on 597 patients with coronary artery disease which revealed that CXCL12 rs2839693 TT was associated with increased risk to coronary artery disease in men [12].
The multivariate logistic regression analysis of the genotypes against clinical COVID19 revealed that the combined genotype CT + TT acts as independent predictor for the severe or critical clinical condition of COVID 19.
According to CXCL12 rs2839693 genotypes, our results revealed a non-significant difference among genotypes regarding age, gender, vaccination, and Co-morbid diseases. On the other side, regarding symptoms, our findings showed significant associations of genotypic distributions with dyspnea, vomiting, and dysarthria of COVID-19 patients. Dyspnea was more prevalent in the combined CT + TT and the TT genotypes compared with the CC and the CT, CC genotypes, respectively. Vomiting and dysarthria were significantly prevalent in the TT genotypes compared with the CT, CC genotypes. Regarding clinical course of the disease, we found that severe or critical illness associated with the combined CT + TT and the TT genotypes was more prevalent in the combined CT + TT and the TT genotypes compared with the CC and the CT, CC genotypes respectively.
According to laboratory evaluation, our results showed significant differences between genotypes as regard to CRP, D-dimers, and ferritin. CRP and D-dimers are significantly elevated in the combined CT + TT and the TT compared with the CC and the CC, CT genotypes; while ferritin was significantly elevated in the TT compared with the CC, CT genotypes. Additionally, no significant differences were found between the 3 genotypes as regarding lymphocyte count, leucocyte count, and CT findings.
Regarding treatment, a significant difference between genotypes as regarding clexane as a treatment was detected; Clexane was more prevalent in the TT genotype than the CC and the CT genotype. The number of patients without any demand for oxygen therapy was significantly different between the genotypes where it was more prevalent in the CC genotype compared with the combined CT + CC and the TT genotypes. Nasal cannula and invasive mechanical ventilation were more prevalent in the TT and the combined CT + TT genotypes compared with the combined CC, CT and the CC genotypes, respectively. Mask oxygen was used more prevalently in the patients of the CT + TT genotypes than those of the CC genotype.
The number of patients needed home management was significantly higher in the CC genotype compared with the combined CT + TT and the TT genotype. The need for ICU stay was significantly higher in patients with the combined CT + TT and the TT genotype compared with the CC and the CC, CT, respectively. Regarding the mortality rates, our results revealed that they were significantly higher in the combined CT + TT and the TT genotype compared with the CC and the CC, CT, respectively. Patients with the TT genotype had a longer duration of in-hospital stay than patients with the CC genotype.
Our findings may provide new insights on understanding the different factors affecting disease severity and mechanisms of cytokine storm syndrome which could affect COVID-19 outcomes and treatment strategies.
There are two limitations that we encountered while conducting this study. First, the number of patients was limited due to the difficulty in obtaining samples from critical cases, cases without symptoms, or cases that had recovered from the disease. Secondly, some cases were removed from the study due to negative smears or some comorbidities that are not suitable for the study.
Recommendations
The present study recommends studying other SNPs in the CXCL12 gene and their relationship with COVID-19 pathogenicity and severity. It also recommends expanding the study patient population to better understand the effect of CXCL12 gene variations on COVID-19 patients.
Conclusion
Our data indicated the signature of CXCL12 rs2839693 in the pathogenesis and severity of COVID-19. Patients with the TT genotype or the T allele at increased risk developed severe or critical rather than mild or moderate disease. Also, patients' admission circumstances, such as vaccination, comorbidities, and symptoms may indicate disease severity. These variables require additional exploration and should be taken into account for risk categorization.
Availability of data and materials
The datasets generated and/or analysed during the current study are available at biosample depository, SubmissionID: SUB13604667 https:// ncbi.nlm.nih.gov /subs/biosample/SUB13604667.
Abbreviations
- C:
-
Degree Celsius
- ACE 2:
-
Angiotensin-converting enzyme II
- ARDS:
-
Acute respiratory distress syndrome
- BCG:
-
Bacille Calmette-Guérin
- COPD:
-
Chronic obstructive pulmonary disease
- COVID-19:
-
Coronavirus disease 2019
- CT:
-
Computed tomography
- ICU:
-
Intensive care unit
- IFN-γ:
-
Interferon-gamma
- PCR:
-
L: liter
- mL:
-
Millileter, mg/L: milligram/Liter, μg/L: microgram/Liter, Polymerase chain reaction
- RT-PCR:
-
Reverse transcription polymerase chain reaction, SARS-CoV-2: Severe acute respiratory syndrome coronavirus 2
- SpO2:
-
Oxygen saturation
- TMPRSS2:
-
Transmembrane protease serine 2
- TNF-α:
-
Tumor necrosis factor-alpha
- VOCs:
-
Variants of concern
- WHO:
-
World Health Organization
References
Gambichler T, et al. Cutaneous findings following COVID-19 vaccination: review of world literature and own experience. J Eur Acad Dermatology Venereol. 2022;36(2):172–80.
Guan W, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382(18):1708–20.
Tian D, Sun Y, Xu H, Ye Q. The emergence and epidemic characteristics of the highly mutated SARS-CoV-2 Omicron variant. J Med Virol. 2022;94(6):2376–83.
Medhat MA, El Kassas M. COVID-19 in Egypt: Uncovered figures or a different situation? J Glob Health. 2020;10(1):010368.
Smail SW, Babaei E, Amin K. Demographic, clinical and genetic factors associated with COVID-19 disease susceptibility and mortality in a Kurdish population. Ann Saudi Med. 2023;43(3):125–42.
Wu C, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Intern Med. 2020;180(7):934–43.
Khalil BA, Elemam NM, Maghazachi AA. Chemokines and chemokine receptors during COVID-19 infection. Comput Struct Biotechnol J. 2021;19:976–88.
Hue S, et al. Uncontrolled innate and impaired adaptive immune responses in patients with COVID-19 acute respiratory distress syndrome. Am J Respir Crit Care Med. 2020;202(11):1509–19.
Modi WS, et al. Haplotype analysis of the SDF-1 (CXCL12) gene in a longitudinal HIV-1/AIDS cohort study. Genes Immun. 2005;6(8):691–8.
Selvaraj P, Alagarasu K, Singh B. Stromal cell-derived factor-1 (SDF-1/CXCL12) gene polymorphisms in pulmonary tuberculosis patients of south India. Int J Immunogenet. 2012;39(1):26–31.
Lin S, et al. Associations of CXCL12 polymorphisms with clinicopathological features in breast cancer: a case-control study. Mol Biol Rep. 2022;49(3):2255–63.
Zhang J, Ma H, Gao J, Kong S, You J, Sheng Y. Variants in the CXCL12 gene was associated with coronary artery disease susceptibility in Chinese Han population. Oncotarget. 2017;8(33):54518.
Mohamed YA, et al. Stromal derived factor-1 gene polymorphism in pediatric immune thrombocytopenia. J Pediatr Hematol Oncol. 2022;44(2):e319–23.
W. H. Organization. WHO COVID-19: case definitions: updated in public health surveillance for COVID-19, published 16 December 2020. World Health Organization; 2020.
Gui-Qiang W, Lei Z, Xia W, Yan-Mei J, Fu-Sheng W. Diagnosis and treatment protocol for COVID-19 patients (tentative 8th edition): interpretation of updated key points. Infect Dis Immun. 2021;1(01):17–9.
Takazawa A, Morita S. Optimal decision criteria for the study design and sample size of a biomarker-driven phase III trial. Ther Innov Regul Sci. 2020;54:1018–34.
Belperio JA, Phillips RJ, Burdick MD, Lutz M, Keane M, Strieter R. The SDF-1/CXCL 12/CXCR4 biological axis in non-small cell lung cancer metastases. Chest. 2004;125(5):156S.
Kirkpatrick LA. A simple guide to IBM SPSS Statistics-Version 23.0. Cengage Learning. 2015.
Petrakis V, Panagopoulos P, Papazoglou D, Papanas N. Diabetes mellitus and hypertension as major risk factors of mortality from Covid-19 pneumonia. Exp Clin Endocrinol Diabetes. 2022;130(03):205–6.
Rodriguez-Morales AJ, et al. Clinical, laboratory and imaging features of COVID-19: a systematic review and meta-analysis. Travel Med Infect Dis. 2020;34:101623.
Kadhim AS, Abdullah YJ. Serum levels of interleukin-6, ferritin, C-reactive protein, lactate dehydrogenase, D-dimer, and count of lymphocytes and neutrophils in COVID-19 patients: Its correlation to the disease severity. Biomed Biotechnol Res J. 2021;5(1):69.
Smail SW, Babaei E, Amin K. Hematological, inflammatory, coagulation, and oxidative/antioxidant biomarkers as predictors for severity and mortality in COVID-19: a prospective cohort-study. Int J Gen Med. 2023;16:565–80.
Bao C, Liu X, Zhang H, Li Y, Liu J. Coronavirus disease 2019 (COVID-19) CT findings: a systematic review and meta-analysis. J Am Coll Radiol. 2020;17(6):701–9.
Langford BJ, et al. Antibiotic prescribing in patients with COVID-19: rapid review and meta-analysis. Clin Microbiol Infect. 2021;27(4):520–31.
Alwafi H, et al. Predictors of length of hospital stay, mortality, and outcomes among hospitalised COVID-19 patients in Saudi Arabia: a cross-sectional study. J Multidiscip Healthc. 2021;14:839–52.
López-Cheda A, Jácome M-A, Cao R, De Salazar PM. Estimating lengths-of-stay of hospitalised COVID-19 patients using a non-parametric model: a case study in Galicia (Spain). Epidemiol Infect. 2021;149:e102.
SeyedAlinaghi S, et al. Predictors of the prolonged recovery period in COVID-19 patients: a cross-sectional study. Eur J Med Res. 2021;26(1):1–10.
Immovilli P, Morelli N, Antonucci E, Radaelli G, Barbera M, Guidetti D. COVID-19 mortality and ICU admission: the Italian experience. Crit Care. 2020;24(1):1–2.
Cambier S, et al. Proteolytic inactivation of CXCL12 in the lungs and circulation of COVID-19 patients. Cell Mol Life Sci. 2023;80(8):234.
McCandless EE, Piccio L, Woerner BM, et al. Pathological expression of CXCL12 at the blood-brain barrier correlates with severity of multiple sclerosis. Am J Pathol. 2008;172(3):799–808.
Xu G, et al. Persistent viral activity, cytokine storm, and lung fibrosis in a case of severe COVID-19. Clin Transl Med. 2020;10(7):e224.
Martínez-Fleta P, et al. A differential signature of circulating miRNAs and cytokines between COVID-19 and community-acquired pneumonia uncovers novel physiopathological mechanisms of COVID-19. Front Immunol. 2022;12:815651.
Gheware A, et al. ACE2 protein expression in lung tissues of severe COVID-19 infection. Sci Rep. 2022;12(1):4058.
Masiá M, et al. SARS-CoV-2 seroconversion and viral clearance in patients hospitalized with COVID-19: viral load predicts antibody response. Open Forum Infect Dis. 2021;8(2):ofab005.
Zheng F, et al. SARS-CoV-2 clearance in COVID-19 patients with Novaferon treatment: a randomized, open-label, parallel-group trial. Int J Infect Dis. 2020;99:84–91.
Wang X, et al. Clinical relevance of single nucleotide polymorphisms in the CXCL1 and CXCL12 genes in patients with major trauma. J Trauma Acute Care Surg. 2019;86(3):440–7.
Acknowledgements
Not applicable.
Funding
Open access funding provided by The Science, Technology & Innovation Funding Authority (STDF) in cooperation with The Egyptian Knowledge Bank (EKB).
Author information
Authors and Affiliations
Contributions
OK and AA. wrote the manuscript text and data analysis. OK and DM: data collection from patients, blood specimens collection. OK and WA: manuscript revision, the practical work. MM: revising the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All participants were registered after they donated cheerfully appreciative agreement to contribute to our study. Protocol was authorized by the Institutional review board of the Faculty of Medicine, at Asyut University, Assiut, Egypt, and was conducted in concordance with Declaration of Helsinki (ethical principles for medical research involving human subjects). Institutional review board local approval number: 17200716. Date of approval from the ethics committee 24/04/2022.
Informed consent was obtained from all subjects and/or their legal guardians to contribute to our study.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Korayem, O.H., Ahmed, A.E., Meabed, M.H. et al. Genetic clues to COVID-19 severity: exploring the stromal cell-derived factor-1/CXCL12 rs2839693 polymorphism in adult Egyptians. BMC Infect Dis 23, 702 (2023). https://doi.org/10.1186/s12879-023-08691-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-023-08691-1