Abstract
Background and aim
Epstein-Barr virus-associated hemophagocytic lymphohistiocytosis (EBV-HLH) and infectious mononucleosis (EBV-IM) share mimic symptoms in the early stages of childhood development. We aimed to examine the clinical features and laboratory indices of these two diseases in children and uncover unique indicators to assist pediatricians in identifying these diseases early.
Methods
We collected clinical data from 791 pediatric patients diagnosed with EBV-IM or EBV-HLH, compared the clinical traits and laboratory biomarkers presented in the two groups, and constructed predictive models based on them.
Results
Patients with EBV-IM had greater ratios of cervical lymphadenopathy, eyelid edema, and tonsillitis, whereas individuals with EBV-HLH were more likely to have hepatomegaly and splenomegaly. When using the criteria of interleukin (IL)-10 > 89.6 pg/mL, interferon (IFN)-γ > 45.6 pg/mL, ferritin > 429 μg/L, D-dimer > 3.15 mg/L and triglycerides > 2.1 mmol/L, the sensitivity was 87.9%, 90.7%, 98.1%, 91.1% and 81.5% to predict EBV-HLH, while the specificity was 98.4%, 96.3%, 96.5%, 94.1% and 80.6%, respectively. A logistic regression model based on four parameters (IL-10, ferritin, D-dimer, and triglycerides) was established to distinguish EBV-HLH patients from EBV-IM patients, with a sensitivity of 98.0% and a specificity of 98.2%.
Conclusions
IL-10, IFN-γ, ferritin and D-dimer levels are significantly different between EBV-HLH and EBV-IM. Predictive models based on clinical signs and laboratory findings provide simple tools to distinguish the two situations.
Similar content being viewed by others
Introduction
Epstein-Barr virus (EBV) is a subfamily herpesvirus that over 90% of individuals have contracted and is one of eight major herpesviruses that cause human disease [1, 2]. EBV infection in humans can be asymptomatic. However, most patients develop infectious mononucleosis (IM) after infection, while other types like EBV-associated hemophagocytic lymphohistiocytosis (EBV-HLH), chronic active EBV infection (CAEBV), EBV-associated lymphoproliferative disorder (EBV-LPD) are relatively rare. In more extreme circumstances, EBV infection can also lead to the development of malignancies such as lymphoma, nasopharyngeal carcinoma, and gastric cancer [3, 4].
Fever, tonsillitis, and cervical lymph node enlargement are clinical symptoms of IM, which can affect people of all ages and appear in all populations [5]. The clinical signs and symptoms of IM vary and lack specificity. Patients do not always produce EBV-specific antibodies when infected with the virus for the first time and do not show typical clinical symptoms if they have immunosuppression or genetic abnormalities, potentially resulting in an incorrect diagnosis [6]. A set of hyperinflammatory response syndromes known as hemophagocytic lymphohistiocytosis(HLH) are characterized by overactive cytotoxic T cells (CTL) and macrophages [7]. EBV-HLH is defined as HLH with EBV infection and no gene abnormalities associated with primary HLH [8]. EBV-HLH has a higher fatality rate than EBV-IM; however, the two illnesses occasionally exhibit similar early-stage symptoms. Thus, early identifying and treating these two diseases is critical for saving lives [9]. Our team has used a cytokine profile as a supplementary instrument for rapidly evaluating HLH [10, 11], and it is essential to discover other clinical or laboratory markers that aid in the early identification of HLH in patients with childhood EBV-IM in addition to the cytokine pattern. Li et al. and Smits et al. have developed predict models to early identify HLH patients from those with acute EBV-infection or suspected HLH, which include clinical, biologic, and cytologic variables but without cytokine profile [12, 13].
Herein, a retrospective study of pediatric patients diagnosed with EBV-HLH and EBV-IM was conducted to analyze clinical characteristics and laboratory data to identify potential indices to predict EBV-HLH. In addition, we investigated whether the simultaneous detection of multiple biological indicators could improve the accuracy of the differential diagnosis.
Patients and Methods
Patients
Pediatric patients with EBV-IM at Children’s Hospital of Zhejiang University School of Medicine between January 2019 and March 2022 were included in this retrospective analysis, as were those diagnosed with EBV-HLH between June 2017 and December 2022. Clinical data included sex, age, physical signs, routine blood analysis results, serum cytokines (interleukin (IL)- 6, IL-10, interferon-gamma (IFN-γ) and tumor necrotic factor-alpha (TNF-α)), lymphocyte subsets, and EBV DNA copies. The study protocol was approved by the Ethics Committee of Children’s Hospital of Zhejiang University School of Medicine (IRB number 2023-IRB-0014-P-01) and conducted in accordance with the tenets of the Declaration of Helsinki.
Diagnostic criteria
EBV-HLH was diagnosed in patients who match the HLH-2004 criteria and show signs of active EBV infection [14]. Patients fulfilled at least five of the eight criteria were diagnosed as HLH: (1) fever; (2) splenomegaly; (3) at least two of the three lineages are affected by cytopenia (hemoglobin < 90 g/L, platelets < 100 × 109/L, and/or neutrophils < 1.0 × 109/L); (4) hypertriglyceridemia (≥ 265 mg/dL) and/or hypofibrinogenemia (≤ 150 g/dL); (5) hematophagy has been discovered in the bone marrow, spleen, liver, and lymph nodes; (6) natural killer (NK) cell activity is low or undetectable; (7) ferritin levels ≥ 500 μg/L; and (8) increased interleukin-2 receptor levels (soluble CD25). Patients who were positive for seral EBV DNA by polymerase chain reaction (PCR) were considered as active EBV infection. Patients fulfilling the definition of primary HLH were excluded. Primary HLH was defined as presence of genetic inborn errors of immunity with HLH as a main feature of the disease, including FHL and HLH caused by RAB27A, LYST, AP3B1, SH2D1A, and BIRC4 variants.
EBV-IM is diagnosed on the basis of clinical manifestation and laboratory results [15]. The clinical indices include the following: (1) fever; (2) pharyngeal tonsillitis; (3) cervical lymph node enlargement; (4) splenomegaly; (5) hepatomegaly; and (6) eyelid edema. The biological marker findings in EBV-IM are as follows: (1) Positive for anti-EBV-VCA-IgM and anti-EBV-VCA-IgG antibodies and negative for anti-EBV-NA-IgG antibodies; (2) negative for anti-EBV-VCA-IgM antibodies but positive for anti-EBV-VCA-IgG and low-affinity antibodies; (3) anti-EBV-VCA-IgG levels increased ≥ 4-fold in two serum samples; and (4) positive for EBV DNA by polymerase chain reaction. Patients who met one of the biochemical indicators and any three physical indices were diagnosed with IM.
Determination of cytokines and lymphocyte subsets
Cytokine levels were determined by flow cytometry using a cytometric bead array (CBA) human Th1/Th2 Cytokine Kit II (BD, USA) [16]. The lower and upper limits of detection for each cytokine were 1.0 and 5000 pg/mL, respectively. In the statistical analysis, 5000 pg/mL was substituted when values exceeded this number. Peripheral blood samples were examined using a Multitest TBNK kit (BD, USA) and FACSDiva software (BD, USA) on a FACSCanto II (Becton–Dickinson, USA) for the lymphocyte subset assay.
Statistical method
Proper quartiles (median, Q1, and Q3), or absolute values and percentages were used to illustrate the data. The two datasets were compared using the chi-squared test or the Mann–Whitney U test. The effectiveness of biomarkers in distinguishing EBV-HLH from EBV-IM was assessed using receiver operating characteristic (ROC) curves. The optimal cutoff values were selected using the Youden index. Logistic regression was used to build a model with four parameters to assess the diagnostic value in discriminating EBV-HLH and EBV-IM. The Hosmer–Lemeshow goodness of fit test was utilized to estimate how well the prediction model was calibrated. P > 0.05 indicated that the predictive model’s calibration level was meaningful. The data were analyzed using SPSS (20.0) and GraphPad Prism (9.4.1). P < 0.05 was considered to indicate significance.
Results
Patients’ characteristics
Of the 791 children, 108 were diagnosed with EBV-HLH and 683 with EBV-IM. The demographic characteristics for both samples are displayed in Table 1. The ratio of female patients in HLH group was higher than that in IM group (P = 0.011). Regarding symptoms, patients with EBV-HLH were more likely to present with hepatomegaly and splenomegaly, while those with EBV-IM more frequently presented with eyelid edema, cervical lymphadenopathy, and tonsillitis (all P < 0.0001).
Comparison of laboratory findings in EBV-HLH and EBV-IM patients
EBV-HLH and EBV-IM can cause multiple organ damage; thus, the hematological indices, liver and renal function parameters, serum cytokines, and lymphocyte subsets were examined. Unlike in EBV-IM patients, cytopenia, hypoalbuminemia and elevated bilirubin, liver enzymes, triglycerides, ferritin, and lactate dehydrogenase (LDH) were common in patients with EBV-HLH (Table 2). D-dimer level was significantly higher in EBV-HLH than that in EBV-IM while fibrinogen levels were much lower. The median EBV-DNA copy number in the plasma was approximately 90 times higher in EBV-HLH patients than that in EBV-IM patients.
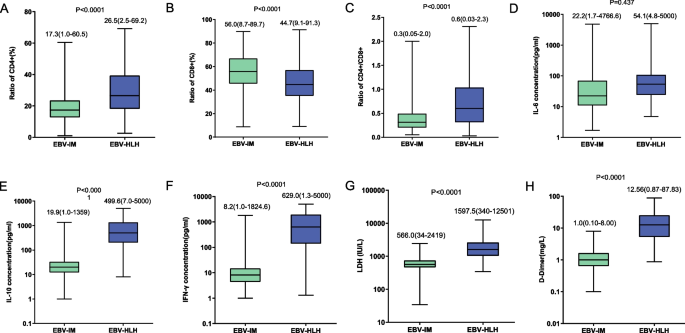
Regarding cytokines, the IL-6 level was similar, while IL-10 (median concentration: 499.6 pg/mL vs. 19.9 pg/mL, P < 0.001) and IFN-γ (median concentration: 629.0 pg/mL vs. 8.2 pg/mL, P < 0.001) levels were significantly higher in patients with EBV-HLH (Fig. 1). The CD8 + T cell ratio in the EBV-HLH group was considerably lower than that in the EBV-IM group (44.7% vs. 56.0%, P < 0.001), while the total CD3 + T cell count was comparable (84.2% vs. 85.30%, P = 0.07).
Laboratory indicators were compared between patients with EBV-HLH and those with EBV-IM, including proportion of CD4 + T cells among all T cells (A), proportion of CD8 + T cells (B), ratio of CD4 + /CD8 + T cells (C), levels of interleukin (IL)-6 (D), IL-10 (E), interferon-gamma (IFN-γ) (F), lactate dehydrogenase (LDH) (G) and D-dimer (H)
As the clinical manifestation and laboratory data can be affected by the age of patients, we then compared the above parameters in different age groups. The patients were divided into three groups: age ≤ 3 years old, > 3 years old and ≤ 6 years old, and > 6 years old. The ratios of CD4 + and CD8 + T cells were different among the three groups while other parameters were comparable. The comparison results were similar among the three age groups which were shown in Supplementary Figs. 1 and 2.
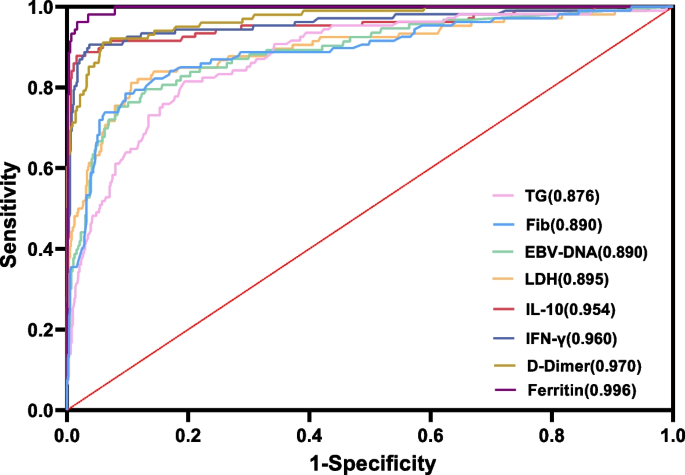
Distinguishing EBV-HLH from EBV-IM by laboratory parameters
Although the severity of EBV-HLH and EBV-IM differ greatly, it is challenging to promptly recognize and distinguish EBV-HLH from EBV-IM due to a lack of early-stage symptoms. Using ROC analysis, we compared the ability of IL-10, IFN-γ, LDH, D-dimer, EBV-DNA copy number, triglycerides, fibrinogen, and ferritin to distinguish EBV-HLH from EBV-IM (Fig. 2). The areas under the curve (AUC) for IL-10, IFN-γ, LDH, D-dimer, triglycerides and ferritin were 0.954, 0.960, 0.895, 0.970, 0.876 and 0.996, respectively, indicating that these indices showed good performance for predicting EBV-HLH. When the cutoff values for IL-10, IFN-γ, LDH, D-dimer, triglycerides and ferritin were set at 89.6 pg/mL, 45.6 pg/mL, 948.5 IU/L, 3.15 mg/L, 2.1 mmol/L and 429 μg/L, the sensitivity was 87.9%, 90.7%, 81.1%, 91.1%, 81.5%and 98.1%, and the specificity was 98.4%, 96.3%, 89.4%, 94.1%, 80.6% and 96.5%, respectively (Table 3).
Of the five univariate variables, IL-10, IFN-γ, LDH, D-dimer and EBV-DNA copy number, as the cutoff values increased, the positive predictive value (PPV) reached 100%, and the negative predictive value (NPV) reduced to approximately 86%. The ideal cutoff value may be the junction of PPV and NPV, which has reference value for clinically distinguishing EBV-HLH from EBV-IM (Fig. 3). The greatest cutoff value selected with the intersection points is higher than that in the maximum value Youden’s index (IL-10: 288.3 pg/mL vs. 89.6 pg/mL, IFN-γ: 240.7 pg/mL vs. 45.6 pg/mL, LDH: 2100 IU/L vs. 948.5 IU/L, D-dimer: 4.50 mg/L vs. 3.15 mg/L, and EBV-DNA copy number: 500000 copies/ml vs. 26400 copies/ml), and the positive predictive value is also higher (Supplementary Table 1).
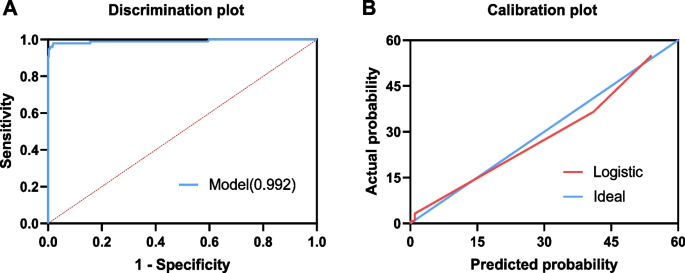
Predictive models for EBV-HLH
A single variable sometimes fails to distinguish two entities in their early stages. Thus, we developed a predictive model using multivariate logistic regression analysis to determine which factors were the most effective predictors. All the laboratory indices that were significantly different between the two groups were included, among which IL-10, ferritin, D-dimer, and triglycerides showed statistical significance in the multivariate logistic regression analysis. Then we developed a logistic regression model based on continuous variables, including IL-10, ferritin, D-dimer, and triglycerides [logit P = -9.969 + 0.057 × IL-10 + 0.006 × ferritin + 0.113 × D-dimer + 0.434 × triglycerides] (Table 4). The AUC for this model was 0.992 (Fig. 4A). The sensitivity and specificity were 97.96% (95% CI, 92.82–99.75) and 98.16% (96.40–99.20) for the diagnosis of EBV-HLH, and the PPV and NPV were 92.31% (85.79–95.98) and 99.53% (95% CI, 98.18–99.88), respectively. The positive and negative likelihood ratios were 53.14 (95% CI, 26.73–105.65) and 0.02 (95% CI, 0.01–0.08), respectively. Then, we employed the Hosmer–Lemeshow goodness-of-fit test to evaluate the calibration of the model, which indicated that the prediction model has a good capacity for calibration (χ2 = 2.077, P = 0.979) (Fig. 4B).
Considering cytokine determination is not available or the serum cytokine levels may not return with a quick turnaround time at some medical centers for emergent situations, we established another predictive model based on physical sign and frequently used laboratory indices. Based on univariate analysis, cervical lymphadenopathy, LDH, D-Dimer and triglycerides were enrolled into a logistic regression model, The AUC for this model was 0.963[logit P = -6.187 + 0.002 × LDH + 0.257 × D-dimer + 0.394 × Triglyceride -3.049 × Cervical lymphadenopathy]. The sensitivity and specificity were 86.32% (95% CI, 77.98–91.83) and 96.53% (94.57–97.79) for the diagnosis of EBV-HLH (Supplementary Fig. 3 and Supplementary Table 2).
Discussion
Most primary EBV infections present as IM in children, while a fraction of patients will progress to EBV-HLH [17]. Early management of EBV infection is related to the development of innate immune cells, such as NK (natural killer) cells and CD8 + and CD4 + T cells [17, 18]. In recent years, many studies have investigated the prognostic aspects of HLH in pediatric patients, and one of the conclusions drawn from these studies was that the lymphocyte subset was crucial for determining the disease's prognosis [19]. In addition, past research has demonstrated that the condition of children diagnosed with IM is intricately connected to the peripheral lymphocyte subsets [20]. In this study, the percentage of CD8 + T cells in EBV-HLH patients was much lower than that in EBV-IM patients, yet the levels of IFN-γ were significantly higher, indicating the complicated pathophysiology of HLH. While the percentage of CD4 + and CD8 + T cells and the ratio of CD4 + /CD8 + cells did not effectively distinguish the two entities because of their low sensitivity, similar to the findings of a previous report [21]. Immune molecular mechanisms driven by EBV infection that generate IM and HLH require further investigation.
EBV-HLH is caused primarily by EBV infection, which aberrantly activates CD8 + T and NK cells and drives their proliferation, resulting in a Th1/Th2 cell imbalance and immunological disorders with a high cytokine production [22, 23]. We previously demonstrated that the classical cytokine profile of HLH in EBV-HLH is substantially elevated IFN-γ and IL-10 and moderately elevated IL-6 [16, 24]. Here, the ROC values showed high sensitivity and specificity of the IFN-γ and IL-10 indices for recognizing EBV-HLH from EBV-IM. Therefore, it would be worthwhile to investigate the biochemical profiles of EBV-IM and EBV-HLH with different cytokine patterns following EBV infection.
Primary fibrinolysis and disseminated intravascular coagulation (DIC) can cause hypofibrinogenemia, and D-dimer is a potentially sensitive marker of intravascular fibrinolysis [25]. Patients with serious conditions such as HLH can exhibit DIC [26]. Our research revealed that patients with EBV-HLH had considerably greater D-dimer levels than those with EBV-IM, providing a valuable indicator for distinguishing the two entities. We also illustrated that the serum EBV-DNA load was significantly higher in EBV-HLH patients than in IM patients, consistent with the findings of earlier studies [6, 21, 27]; thus, if patients have a high EBV-DNA burden, the likelihood of EBV-HLH should be evaluated in depth.
In our retrospective study, some children ultimately diagnosed with HLH were misdiagnosed with IM at an earlier stage of the disease, resulting in a delay in treatment and, ultimately, death. Our results demonstrate that the PPV and NPV shift depending on the cutoff threshold used. For example, when we set the LDH cutoff value to 948.5 IU/L, the PPV is 56.2%, and the NPV is 96.6%. However, when we increased the cutoff value to 2100 IU/L, both the PPV and the NPV neared 92.0%. Thus, if a physician uses an LDH cutoff value of 948.5 IU/L as the reference, roughly 40% of children with HLH may be misdiagnosed, lowering their chances of survival. Therefore, choosing an acceptable cutoff value for clinical guidance is important.
Individuals with acute EBV infection have many clinical and biochemical characteristics of HLH, such as fever, splenomegaly, and liver dysfunction, making EBV-HLH difficult to separate from EBV-IM in some cases [28]. Although our study indicated that ferritin had good specificity and sensitivity in separating the two diseases at an early stage, some infants with HLH did not exhibit typical symptoms of elevated ferritin at that time; therefore, a comprehensive diagnosis model with multiple indicators is required. Li et al. developed an EBV-HLH score with five parameters, including hemoglobin, platelet, neutrophil, albumin, and LDH, which has a sensitivity of 89.2% and a specificity of 89.5%, to help identify EBV patients that need additional HLH screening [12]. Smits et al. discovered a minimal parameter set consisting phagocytosis, splenomegaly, cytopenia, increased ferritin, and increased triglycerides that can predict HLH with a sensitivity of 95% and a specificity of 94% [13]. However, there is no current model to distinguish EBV-HLH from IM. Based on variables (lymphadenopathy, IL-10, ferritin, D-dimer, LDH and triglycerides), we developed two predictive models for EBV-HLH in childhood with EBV infection with both specificity higher than 95%. These models may be useful to distinguish these two presentations more accurately than a single laboratory index. Interestingly, serum ferritin, which is an important parameter for the diagnosis of HLH, presented excellent ability to distinguish EBV-HLH from IM, with AUC of 0.996 (Table 3). However, considering some patients with HLH may not show significantly elevated ferritin or the result may not be quick available sometimes, other predict models still have their values in this circumstance.
Several limitations applied to this study. First, as this was a retrospective study, we could not follow up on the patients from the onset of fever to the time of EBV-HLH diagnosis. We collected the data when the diagnosis was established, thus potentially missing some biomarkers with early predictive value. Second, IL-18 is an important biomarker which is increased in infectious diseases and HLH [29]. It may have potential values for the distinguishment of HLH from IM. However, IL-18 was not included in our detection kit and we were not able to perform such analysis. Third, due to the single-center nature of this investigation, the repeatability of our results and conclusion require additional validation in other cohorts.
In conclusion, the present study showed IL-10, IFN-γ, LDH, D-dimer and ferritin were good biomarkers for distinguishing EBV-HLH from EBV-IM early. Integrating multiple biomarkers can further improve the accuracy of this model.
Availability of data and materials
The datasets analyzed during the current study available from the corresponding author on reasonable request.
Abbreviations
- EBV-HLH:
-
Epstein-Barr virus associated hemophagocytic lymphohistiocytosis
- EBV-IM:
-
Epstein-Barr virus associated infectious mononucleosis
- IL-10:
-
Interleukin-10
- IFN‐γ:
-
Interferon-gamma
- LDH:
-
Lactate dehydrogenase
- Fib:
-
Fibrinogen
References
Thompson MP, Kurzrock R. Epstein-Barr virus and cancer. Clin Cancer Res. 2004;10(3):803–21. https://doi.org/10.1158/1078-0432.ccr-0670-3.
Cohen JI. Epstein-Barr virus infection. N Engl J Med. 2000;343(7):481–92. https://doi.org/10.1056/NEJM200008173430707.
Smatti MK, Al-Sadeq DW, Ali NH, Pintus G, Abou-Saleh H, Nasrallah GK. Epstein-Barr Virus Epidemiology, Serology, and Genetic Variability of LMP-1 Oncogene Among Healthy Population: An Update. Front Oncol. 2018;8:211. https://doi.org/10.3389/fonc.2018.00211.
Dunmire SK, Verghese PS, Balfour HH. Primary Epstein-Barr virus infection. J Clin Virol. 2018;102:84–92. https://doi.org/10.1016/j.jcv.2018.03.001.
Womack J, Jimenez M. Common questions about infectious mononucleosis. Am Fam Physician. 2015;91(6):372–6.
Shi J, Ma W, Li W. Epidemiologic features of children with Epstein-Barr virus associated diseases in Hangzhou, China. J Med Virol. 2020;92(8):1277–82. https://doi.org/10.1002/jmv.25633.
Janka GE. Familial and acquired hemophagocytic lymphohistiocytosis. Ann Rev Med. 2012;63:233–46. https://doi.org/10.1146/annurev-med-041610-134208.
El-Mallawany NK, Curry CV, Allen CE. Haemophagocytic lymphohistiocytosis and Epstein-Barr virus: a complex relationship with diverse origins, expression and outcomes. Br J Haematol. 2022;196(1):31–44. https://doi.org/10.1111/bjh.17638.
Huang SC, Chen JS, Cheng CN, Yang YJ. Hypoalbuminaemia is an independent predictor for hemophagocytic lymphohistiocytosis in childhood Epstein-Barr virus-associated infectious mononucleosis. Eur J Haematol. 2012;89(5):417–22. https://doi.org/10.1111/ejh.12006.
Chen Y, Wang Z, Luo Z, Zhao N, Yang S, Tang Y. Comparison of Th1/Th2 cytokine profiles between primary and secondary haemophagocytic lymphohistiocytosis. Ital J Pediatr. 2016;42(1):50. https://doi.org/10.1186/s13052-016-0262-7.
Xu XJ, Luo ZB, Song H, Xu WQ, Henter JI, Zhao N, Wu MH, Tang YM. Simple Evaluation of Clinical Situation and Subtypes of Pediatric Hemophagocytic Lymphohistiocytosis by Cytokine Patterns. Front Immunol. 2022;13:850443. https://doi.org/10.3389/fimmu.2022.850443.
Li X, Yan H, Xiao Z, Luo T, Xie L, Yang Y, Gong L, Tang Z, Huang J, Zhang X, Zheng M, Yao Z, Zang P, Zhu D, Lu X. Development of a screening score for Hemophagocytic Lymphohistiocytosis among pediatric patients with acute infection of Epstein-Barr virus. Front Immunol. 2022;13:981251. https://doi.org/10.3389/fimmu.2022.981251.
Smits BM, van Montfrans J, Merrill SA, van de Corput L, van Gijn M, de Vries A, van den Bos C, Abbink F, van der Molen RG, Dors N, Lindemans C, Boelens JJ, Nierkens S. A Minimal Parameter Set Facilitating Early Decision-making in the Diagnosis of Hemophagocytic Lymphohistiocytosis. J Clin Immunol. 2021;41(6):1219–28. https://doi.org/10.1007/s10875-021-01005-7.
Henter JI, Horne A, Aricó M, Egeler RM, Filipovich AH, Imashuku S, Ladisch S, McClain K, Webb D, Winiarski J, Janka G. HLH-2004: Diagnostic and therapeutic guidelines for hemophagocytic lymphohistiocytosis. Pediatr Blood Cancer. 2007;48(2):124–31. https://doi.org/10.1002/pbc.21039.
t.S.o.P. The Subspecialty Group of Infectious Diseases, Chinese Medical Association, The National Group of EpsteinBarr Virus Associated Diseases in Children, Principle suggestions for diagnosis and treatment of main nontumorous EpsteinBarr virusassociated diseases in children, Zhonghua Er Ke Za Zhi. 2016;54(8):563–568.https://doi.org/10.3760/cma.j.issn.0578-1310.2016.08.002.
Tang Y, Xu X, Song H, Yang S, Shi S, Wei J, Pan B, Zhao F, Liao C, Luo C. Early diagnostic and prognostic significance of a specific Th1/Th2 cytokine pattern in children with haemophagocytic syndrome. Br J Haematol. 2008;143(1):84–91. https://doi.org/10.1111/j.1365-2141.2008.07298.x.
Taylor GS, Long HM, Brooks JM, Rickinson AB, Hislop AD. The immunology of Epstein-Barr virus-induced disease. Annu Rev Immunol. 2015;33:787–821. https://doi.org/10.1146/annurev-immunol-032414-112326.
Long HM, Meckiff BJ, Taylor GS. The T-cell Response to Epstein-Barr Virus-New Tricks From an Old Dog. Front Immunol. 2019;10:2193. https://doi.org/10.3389/fimmu.2019.02193.
An Q, Fang DH, Xuan CM, Xu SM, Jin MW, Ji Q. Lymphocyte subsets in children with hemophagocytic lymphohistiocytosis (HLH) and its clinical significance. Eur Rev Med Pharmacol Sci. 2018;22(7):2000–4. https://doi.org/10.26355/eurrev_201804_14728.
Chen L, Chen X, Yao W, Wei X, Jiang Y, Guan J, Liu X, Xie Y, Lu H, Qian J, Zhang Z, Wu L, Lin X. Dynamic Distribution and Clinical Value of Peripheral Lymphocyte Subsets in Children with Infectious Mononucleosis. Indian J Pediatr. 2021;88(2):113–9. https://doi.org/10.1007/s12098-020-03319-7.
Shi J, Chu C, Yu M, Zhang D, Li Y, Fan Y, Yu Y, Luo Y, Zhou W. Clinical warning of hemophagocytic syndrome caused by Epstein-Barr virus. Ital J Pediatr. 2021;47(1):3. https://doi.org/10.1186/s13052-020-00949-7.
Crayne CB, Albeituni S, Nichols KE, Cron RQ. The Immunology of Macrophage Activation Syndrome. Front Immunol. 2019;10:119. https://doi.org/10.3389/fimmu.2019.00119.
Griffin G, Shenoi S, Hughes GC. Hemophagocytic lymphohistiocytosis: an update on pathogenesis, diagnosis, and therapy. Best Pract Res Clin Rheumatol. 2020;34(4):101515. https://doi.org/10.1016/j.berh.2020.101515.
XJ Xu, HS Wang, XL Ju, PF Xiao, Y Xiao, HM Xue, HY Shi, YJ Gao, GC Jia, XR Li, WH Zhao, NL Wang, YM Tang, S Histiocytosis Study Group of the Chinese Pediatric. Clinical presentation and outcome of pediatric patients with hemophagocytic lymphohistiocytosis in China: a retrospective multicenter study. Pediatr Blood Cancer. 2017;64(4).https://doi.org/10.1002/pbc.26264.
JD Olson. D-dimer: an overview of hemostasis and fibrinolysis, assays, and clinical applications. Adv Clin Chem. 2015;69.https://doi.org/10.1016/bs.acc.2014.12.001.
Valade S, Joly BS, Veyradier A, Fadlallah J, Zafrani L, Lemiale V, Launois A, Stepanian A, Galicier L, Fieschi C, Mirouse A, Tudesq JJ, Lepretre A-C, Azoulay E, Darmon M, Mariotte E. Coagulation disorders in patients with severe hemophagocytic lymphohistiocytosis. PloS One. 2021;16(8):e0251216. https://doi.org/10.1371/journal.pone.0251216.
Wang K, Lyu Z, Gao Y, Jia K, Su J. Comparative analysis of Epstein-Barr virus nucleic acid loads in peripheral blood mononuclear cells and plasma. Chin J Lab Med. 2018;41(10):755–8. https://doi.org/10.3760/cma.j.issn.1009-9158.2018.10.010.
Marsh RA. Epstein-Barr Virus and Hemophagocytic Lymphohistiocytosis. Front Immunol. 2017;8:1902. https://doi.org/10.3389/fimmu.2017.01902.
Ou W, Zhao Y, Wei A, Ma H, Zhang Q, Zhang L, Lian H, Wang D, Li Z, Wang T, Zhang R. Serum cytokine pattern in children with hemophagocytic lymphohistiocytosis. Ann Hematol. 2023;102(4):729–39. https://doi.org/10.1007/s00277-023-05132-6.
Acknowledgements
All research participants whose data were used in this investigation are much appreciated.
Funding
This work was funded by grants from the National Natural Science Fund of China (No. 81970122), the Zhejiang Provincial Natural Science Foundation of China (No. LY19H080006), and the Pediatric Leukemia Diagnostic and Treatment Technology Research Center of Zhejiang Province (No. JBZX-201904).
Author information
Authors and Affiliations
Contributions
Yongmin Tang and Xiaojun Xu designed the work. Lisha Cai, Yuan Xing, and Zebin Luo participated in the data collection. Lisha Cai, Zihan Zhang, and Yahong Xia performed the data analysis. Lisha Cai wrote the manuscript draft. Yan Chen and Xiaojun Xu amended the manuscript. Each author made significant contributions and approved the final draft of the work.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the Ethics Committee of Children’s Hospital of Zhejiang University School of Medicine (IRB number 2023-IRB-0014-P-01) and conducted in accordance with the tenets of the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Figure 1. Laboratory indicators were compared between patients with EBV-HLH and those with EBV-IM in three age groups. (*P<0.05, **P<0.01, ***P<0.001, ****P<0.0001) A,CD4+% B,CD8+% C,CD4+/CD8+ D,IL-6 E,IL-10 F, IFN-γ G,LDH, lactate dehydrogenase H,D-dimer.
Additional file 2:
Figure 2. The ROC curve for EBV-HLH prediction using TG, Fib, EBV-DNA loads, LDH, IL-10, IFN-γ, the D-dimer, and ferritin among three age groups. A, age ≤ 3 years old; B, > 3 years old and ≤ 6 years old; C, > 6 years old.
Additional file 3:
Figure 3. Another logistic regression model based on cervical lymphadenopathy, LDH, D-Dimer and triglycerides were established. The AUC of ROC curve for this model reached 0.963 (A) and curves of calibration for the logistic regression model was drawn (B).
Additional file 4:
Supplementary Table 1. Comparison of two optimal cutoff values.
Additional file 5:
Supplementary Table 2. Estimated another model parameters in the selected multivariable logistic regression model.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Cai, L., Xing, Y., Xia, Y. et al. Comparative study of biomarkers for the early identification of Epstein–Barr virus-associated hemophagocytic lymphohistiocytosis in infectious mononucleosis. BMC Infect Dis 23, 728 (2023). https://doi.org/10.1186/s12879-023-08654-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-023-08654-6