Abstract
Background
Candida bloodstream infection (BSI) causes appreciable mortality in neonates and children. There are few studies describing the epidemiology of Candida BSI in children living in sub-Saharan Africa.
Methods
A retrospective descriptive study was conducted at three public sector hospitals in Cape Town, South Africa. Demographic and clinical details, antifungal management and patient outcome data were obtained by medical record review. Candida species distribution and antifungal susceptibility testing results were obtained from the National Health Laboratory Service database.
Results
Of the 97 Candida BSI episodes identified during a five-year period, 48/97 (49%) were Candida albicans (C. albicans), and 49/97 (51%) were non-C. albicans species. The overall incidence risk was 0.8 Candida BSI episodes per 1000 admissions at Red Cross War Memorial Children’s Hospital. Of the 77/97 (79%) Candida BSI episodes with available clinical information, the median age (interquartile range) at the time of BSI was 7 (1–25) months, 36/77 (47%) were associated with moderate or severe underweight-for-age and vasopressor therapy was administered to 22/77 (29%) study participants. Most of the Candida BSI episodes were healthcare-associated infections, 63/77 (82%). Fluconazole resistance was documented among 17%, 0% and 0% of C. parapsilosis, C. tropicalis and C. albicans isolates, respectively. All Candida isolates tested were susceptible to amphotericin B and the echinocandins. The mortality rate within 30 days of Candida BSI diagnosis was 13/75 (17%). On multivariable analysis, factors associated with mortality within 30 days of Candida BSI diagnosis included vasopressor therapy requirement during Candida BSI, adjusted Odds ratio (aOR) 53 (95% confidence interval 2–1029); hepatic dysfunction, aOR 13 (95% CI 1–146); and concomitant bacterial BSI, aOR 10 (95% CI 2–60).
Conclusion
The study adds to the limited number of studies describing paediatric Candida BSI in sub-Saharan Africa. Non-C. Albicans BSI episodes occurred more frequently than C. albicans episodes, and vasopressor therapy requirement, hepatic dysfunction and concomitant bacterial BSI were associated with an increase in 30-day mortality.
Similar content being viewed by others
Background
The reported candidaemia incidence in paediatric patients ranges between 0.2 and 10.5 cases per 1000 admissions [1, 2]. In multicentre, laboratory-based surveillance among hospitalized children in South Africa from 2012 to 2017, the overall incidence risk of paediatric candidaemia at tertiary-level, public-sector hospitals was 5.3 cases per 1000 admissions and ranged from 0.4 to 119.1 per 1000 admissions [3]. A retrospective study on BSI at Red Cross War Memorial Children’s Hospital (RCWMCH), Cape Town, in 2011 and 2012, identified candidaemia in 6.1% of all BSIs [4]. An Egyptian study documented a higher prevalence of 17.3% among all paediatric BSIs [5].
Risk factors for candidaemia in paediatric patients include antibiotic exposure, corticosteroid therapy, the presence of a central venous catheter (CVC), neutropaenia, prior fungal colonisation, and intensive care unit (ICU) admission [6, 7]. Additional risk factors are present during the neonatal period including prematurity, low birth weight (LBW), and related co-morbidities, including total parenteral nutrition (TPN), respiratory disease and mechanical ventilation [6, 8, 9].
Globally, the most prevalent cause of candidaemia has shifted from Candida albicans (C. albicans) to non-C. albicans spp. The frequency of non-C. albicans spp. infections varies according to geographical location, patient characteristics and age. In paediatric populations, C. parapsilosis is the common non-C, albicans sp. associated with candidaemia [10,11,12,13]. Recent paediatric studies from Egypt and China reported that non-C. albicans spp. collectively accounted for the greatest number of cases, although C. albicans was the most common species [5, 14]. In contrast, studies from South Africa showed that C. parapsilosis was the most prevalent species causing Candida BSI followed by C. albicans [3, 15].
The shift to non-C. albicans candidaemia is associated with reduced susceptibility to fluconazole, a first-line antifungal agent in many settings. Several context-specific reasons may underly this shift such as the selection of non-C. albicans spp. under antifungal pressure that are intrinsically resistant to fluconazole e. g. C. krusei, or the selection of resistant non-C. albicans clones during healthcare-associated outbreaks. In one paediatric study conducted in Turkey, fluconazole resistance was lower among C. albicans isolates than non-C. albicans isolates, 4.3% versus 16.6%. In this study, the fluconazole-resistant non-C. albicans isolates were C. krusei isolates [16]. An Egyptian study found that while fluconazole resistance to C. albicans and non-C. albicans spp. accounted for 38.9% and 44% of the total number of Candida spp. tested, respectively, susceptibility to caspofungin, amphotericin B and itraconazole was 99%, 97%, and 73%, respectively against all Candida isolates tested [5]. A neonatal study from Johannesburg reported higher fluconazole resistance among C. parapsilosis isolates compared to C. albicans isolates. The authors of this study suggested that widespread empiric carbapenem usage due to increasing multiresistant bacterial infection may be driving the selection of fluconazole-resistant C. parapsilosis isolates [15]. Similarly, in a South African multicentre study, 35% of all Candida isolates were resistant to fluconazole. Fluconazole resistance was higher among C. parapsilosis isolates than other Candida spp. By contrast, only three of 3061 isolates tested were resistant to echinocandins and all Candida isolates were susceptible to amphotericin B [3].
High mortality has been associated with Candida BSI. A South African study of neonates with fungal BSI (97% of the 59 episodes were caused by Candida spp.) recorded an overall mortality rate of 45.8%. In that study death was significantly associated with LBW and necrotizing enterocolitis [15]. An Egyptian study reported mortality of 64% among children diagnosed with Candida BSI, most deaths were associated with non-C. albicans BSI [5]. As with previous studies, a recent South African study showed that the overall crude 30-day inpatient mortality for patients with Candida BSI is high (38%) and even higher among neonates (43%) and adolescents (43%) [3]. In the Turkish study, treatment in an ICU, the presence of an indwelling CVC, failure to remove an indwelling CVC, and mechanical ventilation during invasive Candida infection were associated with mortality [16].
A limited number of studies have described the epidemiology of candidaemia in children in sub-Saharan Africa. The results of a large multicentre laboratory-based surveillance study of culture-confirmed candidaemia in children in South Africa were recently published. Sixty-four percent of the isolates included in that study were from Gauteng province. Furthermore, risk factor analysis for 30-day mortality among neonates with candidaemia, showed that C. parapsilosis BSI was associated with lower mortality [3]. The present study was undertaken to describe the recent burden of Candida BSI, the clinical presentation, species distribution, antifungal susceptibility, and outcome of Candida BSI among children less than 15 years of age admitted to three public sector hospitals in Cape Town, providing contemporary information about this important infection in the Western Cape province of South Africa.
Methods
Study design, setting and inclusion criteria
This retrospective descriptive study was conducted at RCWMCH, Groote Schuur Hospital (GSH), and Mowbray Maternity Hospital (MMH). The RCWMCH serves as a tertiary referral centre for children in the Western Cape province and surrounding provinces. GSH is a major tertiary referral centre for adult patients but also provided tertiary neonatal and secondary paediatric inpatient services during the study period. MMH is a dedicated maternal and neonatal regional hospital with limited tertiary service. The study was done in children with culture-confirmed Candida BSI, diagnosed between 1 January 2015 and 31 December 2019. All Candida BSI episodes diagnosed at RCWMCH were used in the incidence risk calculations for that hospital. Study participants with available clinical records were used to complete the clinical and microbiology descriptions.
Data collection
The National Health Laboratory Service (NHLS) Central Data Warehouse (CDW) extracted a line list of children admitted to RCWMCH, GSH and MMH with culture-confirmed Candida BSI for the period January 2015 to December 2019. This line list included species identification and antifungal susceptibility testing results.
Where available, paper-based medical records of patients with Candida BSI episodes were reviewed at RCWMCH, GSH and MMH, and relevant data extracted and manually transferred to standardised data collection forms. The microbiology results obtained from the NHLS CDW were added to the data collection forms.
Microbiological procedures
Blood culture specimens from the three hospitals were sent to the GSH NHLS microbiology laboratory for processing. The laboratory uses the BacT/ALERT automated blood culture system (BioMérieux, Marcy-l’Etoile, France). Signal-positive blood culture broth was Gram-stained. Broth with yeasts observed using light microscopy, was inoculated onto 2% horse blood agar and Sabouraud Dextrose agar and incubated aerobically at 37 °C. Yeasts cultured between 24 and 48 h were identified with susceptibility testing performed using the Vitek 2 automated system (BioMérieux, Marcy-l’Etoile, France) YST identification and AST-YS08 cards, respectively. Susceptibility test results were interpreted according to published Clinical and Laboratory Standards Institute guidelines [17].
Study definitions
Candida BSI was defined as isolation of any Candida spp. from blood culture either collected peripherally or via a central venous catheter (CVC).
Candida BSI was classified as (1) infection present on admission (IPOA) if the Candida sp. was cultured from a blood culture obtained on the day of admission (calendar day 1), 2 days before admission or the calendar day after admission (calendar day 2), or (2) healthcare-associated infection (HAI) if the Candida sp. was isolated from a blood culture obtained on or after the 3rd calendar day of admission [18].
Pre-term birth: a gestational age (GA) < 37 completed weeks at birth.
Concomitant bacteraemia: Isolation of a bacterial isolate from the blood culture specimen in which the Candida sp. was isolated.
Human immunodeficiency virus (HIV) status was defined as follows: (1) HIV-infected: a child < 18 months old with a positive HIV deoxyribonucleic acid (DNA) polymerase chain reaction (PCR) result confirmed by either a quantitative HIV ribonucleic acid (RNA) PCR or repeat HIV DNA PCR test, or a child ≥ 18 months old with 2 positive serological test results (HIV enzyme-linked immunosorbent assay or HIV Rapid test) or a positive HIV DNA PCR result confirmed by either a quantitative HIV RNA PCR or repeat HIV DNA PCR test, (2) HIV-uninfected: a child with a negative HIV serological or HIV DNA PCR result and (3) unknown HIV status: a child with unknown maternal HIV status and who was not tested for HIV infection [19].
Moderate and severe underweight for age (UWFA) were defined as weight-for-age z score (WAZ) between − 2 and − 3 standard deviations (SD) of the World Health Organisation (WHO) growth reference standards, and a WAZ < − 3 SD, respectively [20].
The urinary tract was regarded as the site of infection if one of the following criteria was fulfilled: a urine culture yielding a single organism with > 1000 colony-forming units/mL from a suprapubic aspiration or > 10,000 colony-forming units/mL via urethral catheterization [21].
Disseminated intravascular coagulopathy (DIC): A prothrombin time of ≥ 2 s, an activated partial thromboplastin time of ≥ 60 s or a fibrinogen level of < 2 μmol/L [22].
Renal dysfunction: a serum creatinine concentration above the normal age-related range [23, 24].
Liver dysfunction: a ≥ twofold increase of serum aspartate aminotransferase and/or serum alanine aminotransferase concentration and/or a total bilirubin in a child more than 28 days old of > 70 μmol/L [24, 25].
Statistical analysis
The data were analysed using STATA/IC version 14.2 (College Stata, TX, USA). The incidence risk of Candida BSI was calculated per 1000 hospital admissions for RCWMCH. Continuous variables were expressed as medians (interquartile range, IQR) since the continuous data were skewed. Proportions and percentages were used to describe categorical variables.
The Wilcoxon rank-sum test for independent variables was used to compare the continuous data stratified by type of Candida BSI. The association between categorical variables was done using Pearson’s Chi-square test (χ2) or Fisher’s Exact test as appropriate. Two-tailed p-values ≤ 0.05 were considered statistically significant.
Univariable and multivariable logistic regression were used to identify factors independently associated with mortality within 30 days of the date of the blood culture from which Candida sp. was isolated. The multivariable logistic regression model was built by incorporating all variables utilised in the univariable analysis. The multivariable logistic regression model results were expressed as adjusted odds ratios (aORs) and 95% confidence intervals (95% CIs). Mortality associated with C. albicans versus non-C. albicans BSI was analysed using Kaplan–Meier survival estimates and compared between the two using the log rank test.
Results
Study participants
During the study period, there were 97 Candida BSI episodes in 97 participants, 85 episodes at RCWMCH, 11 at GSH and one at MMH. The 85 Candida BSI episodes at RCWMCH were used to estimate the risk of Candida BSI at that hospital. There was insufficient clinical information on twenty episodes of Candida BSI thus 77 (79%) Candida BSI episodes were used in all subsequent analyses (Fig. 1).
Risk of Candida bloodstream infection at RCWMCH
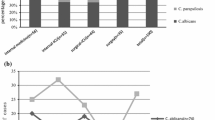
The overall incidence risk throughout the study period was 0.8 episodes/1000 hospital admissions for all Candida BSI episodes, 0.4 episodes/1000 hospital admissions for all C. albicans BSI episodes, 0.5 episodes/1000 hospital admissions for all non-C. albicans BSI episodes, and 0.3 episodes/1000 hospital admissions for all C. parapsilosis BSI episodes; C. parapsilosis being the main contributor to non-C. albicans BSI episodes. With exception of 2018, the overall annual incidence risk increased progressively throughout the study period (Fig. 2). This increase as well as the decline in 2018 were mainly attributed to changes in the incidence risk of non-C. albicans over time (Fig. 2; Additional file 1: Table S1).
Baseline characteristics
Table 1 describes demographic and clinical characteristics of 77 Candida BSI episodes in 77 study participants. The median age at the time of Candida BSI was 6.8 months, IQR 1–25. Close to 50% of the episodes occurred in participants who were moderately or severely underweight for age. Of the 52 participants (68%) whose HIV status was known at the time of their Candida BSI events, only two were HIV-infected. The proportion of participants who were admitted in ICU during the Candida BSI was higher among those with C. albicans BSI episodes compared to those with non-C. albicans BSI episodes, 79% (30/38) vs. 49% (19/39), p = 0.01. Furthermore, a higher proportion of non-C. albicans than C. albicans BSI episodes occurred in participants with haematological conditions or cancer on immunosuppressive treatment 28% (11/39) vs. 5% (2/38), p = 0.01.
Classification and clinical manifestations
Of the 77 Candida BSI episodes, 63 (82%) episodes were HAIs and 14 (18%) were IPOA. The median time between admission and the development of Candida BSI in study participants who experienced HAI was 12 days, IQR 7.0–21.0. A clinical site of infection was identified in 44% of the Candida BSI episodes. Urinary tract as a focus of infection (37% vs. 3%) and renal dysfunction (37% vs. 23%) as a complication were more common in C. albicans BSI than non-C. albicans BSI, p < 0.001. Vasopressor therapy was administered in 22 (29%) episodes and concomitant bacterial BSI was documented in 30% of episodes (Table 2).
Species distribution and antifungal susceptibility of the Candida isolates
During the study period, a total of 77 Candida species were isolated from the 77 children with complete and available clinical information. Of these, 38 (49%) were C. albicans and all were susceptible to fluconazole. Among the non-C. albicans isolates, the most frequent species isolated were C. parapsilosis (31%), C. tropicalis (8%), and C. glabrata (5%). Fluconazole resistance was documented in 13% of C. parapsilosis isolates and 4% categorised as susceptible-dose dependant. All Candida isolates tested were susceptible to amphotericin B and the echinocandins (Table 3).
Antifungal therapy
Of the 77 BSI episodes, 69 (90%) were treated with an antifungal agent. Of the eight episodes (10%) that were not treated at RCWMCH, MMH or GSH, two patients died, two were transferred to another hospital before the diagnosis of Candida BSI was established, and four remained well despite not receiving antifungal therapy. Antifungal therapy was initiated a median of 1 day (IQR, 1–2) after the first diagnostic blood culture was performed. The median duration of all antifungal therapy per episode was 14 days (IQR, 13–20). In 58 of the 69 treated episodes (84%), at least one repeat blood culture was performed during the BSI episode. The median time (IQR) between initial blood culture and repeat blood culture was 2 (2–4) days. The repeat cultures were negative in 56 of these 58 episodes (97%). Thus, a negative blood culture was documented in 56/69 (81%) of the treated BSI episodes. A negative blood culture result was not documented in the two episodes in which single repeat cultures were still positive as no further blood cultures were performed. The median time (IQR) until repeat negative blood culture from initiation of treatment was 4 (2–7) days. The median duration (IQR) of antifungal therapy from negative repeat culture was 13 (10–15) days. After the antifungal susceptibility results became available, the initial antifungal agent was continued in 49 (71%) episodes and changed in 20 (29%) episodes due to resistance (2) or de-escalation (18) to agents with narrower spectrum of antifungal activity. In 5 of the 49 episodes (10%) in which initial antifungal therapy was continued, the susceptibility results indicated that de-escalation was possible but not implemented. Fluconazole was the most frequently used initial antifungal agent, 43/69 (62%), followed by amphotericin B, 21/69 (30%), and caspofungin, 5/69 (7%). After adjustments were made in response to the antifungal susceptibility results, the final treatment regimens were fluconazole, 51/69 (74%), amphotericin B 13/69 (19%) and caspofungin, 5/69 (7%).
Outcome
74% (57/77) of Candida BSI episodes were successfully treated and the children were discharged from hospital after these episodes. During the study period, 14 (18%) children died during or after the Candida BSI episode but prior to hospital discharge (Table 4). Thirteen of these deaths occurred within 30 days of Candida BSI diagnosis and were included in the survival analysis. The median time (IQR) to death of these 13 children was 9 (3–16) days. Table 5 describes risk factors associated with mortality within 30 days of Candida BSI diagnosis in children with Candida BSI. On multivariable analysis, vasopressor therapy requirement, hepatic dysfunction, and concomitant bacterial BSI during Candida BSI were significantly associated with mortality within 30 days of Candida BSI diagnosis. Furthermore, Kaplan–Meier survival analysis showed that there was no significant difference in the survival of patients with C. albicans compared to non-C. albicans BSI episodes, p = 0.3 (Fig. 3).
Discussion
The exact incidence of Candida BSI in children in sub-Saharan Africa is not known due to a lack of systematic epidemiological data. In multicentre laboratory-based surveillance among hospitalized children at public-sector hospitals in South Africa, the overall incidence was 5.3 Candida BSI episodes per 1000 admissions and ranged from 0.4 to 119.1 per 1000 admissions [3]. The incidence risk in our study of 0.8 per 1000 hospital admissions is consistent with this report, although at the lower end of the range. It is also at the lower end of the range of incidence estimates reported by non-South African studies of 0.2–10.5 Candida BSI episodes per 1000 admissions [1, 2]. Good infection prevention practice, less crowded wards, better infrastructure and staffing resources, and presence of antifungal stewardship programmes are possible factors that contribute to lower incidence [26, 27].
Many of the children in our study had interventions and underlying medical conditions that are likely to have predisposed them to Candida BSI. These included prior exposure to antibiotics, the presence of CVCs, parenteral nutrition, treatment in the ICU, and malignancy, and in neonates and infants, preterm birth and necrotising enterocolitis. Similar risk factors have been reported in other studies, including the recent South African multicentre laboratory-based surveillance report [3, 6,7,8,9].
In our study, non-C. albicans spp. collectively accounted for the greater number of cases, although C. albicans was the most common single species accounting for nearly half of all Candida BSI episodes. Similarly, recent paediatric studies from Egypt and China showing a shift to non-C. albicans, reported that C. albicans was still the predominant species [5, 14]. A multicentre paediatric Candida BSI study showed that between 2016 and 2017, C. parapsilosis was the most prevalent species in South Africa although C. albicans remained predominant in less populous provinces [3]. In our study, C. parapsilosis was the most common non-albicans Candida sp. accounting for 31.2% of all Candida isolates. A retrospective cohort study showed that in adult haematological patients with neutropaenia, non-C. albicans species were detected much more frequently than in non-neutropaenic patients. Furthermore, patients with CVCs in situ were at high risk for C. parapsilosis BSI and fluconazole prophylaxis was a risk factor for both C. glabrata and C. krusei BSI. [28]. Similarly, in our study, more than half (55%) of the haematologic patients with non-C. albicans had severe neutropaenia (polymorphonuclear neutrophil count < 500 cells/µL). Additionally, all children in our study who developed C. parapsilosis BSI had CVCs, but none with haematological conditions or cancer were receiving fluconazole prophylaxis.
Unlike previous studies, we found that all C. albicans and C. tropicalis isolates and 83% of C. parapsilosis isolates were susceptible to fluconazole [3, 5]. In a South African multicentre study, over half of the C. parapsilosis isolates were resistant to fluconazole [3]. This contrasts with our finding that only 17% of C. parapsilosis isolates were either resistant or susceptible-dose dependant to fluconazole. The lower fluconazole resistance rate might be due to differences in infection prevention and control practices and hospital antifungal stewardship. In our study, all Candida isolates tested were susceptible to amphotericin B and echinocandins. This is consistent with a large South African study, in which only three of 3061 Candida isolates tested were resistant to echinocandins and all isolates were susceptible to amphotericin B [3]. A study from Egypt published in 2019 also reported very high caspofungin and amphotericin B susceptibilities among Candida BSI isolates tested [5].
In our study, mortality within 30 days of Candida BSI diagnosis was 17% of 75 patients with known outcomes. This is lower than that reported in an Egyptian study of children with Candida BSI (64%), a South African study of neonates with fungal BSI (46%) and a large multicentre study of hospitalised children with Candida BSI (38%) [3, 5, 15]. The lower mortality documented in our study may be related to low fluconazole resistance, early initiation of antifungal therapy, the duration of antifungal therapy administered to our patients, and the availability of support services such as ICU care. In the Egyptian study, most deaths were associated with non-C. albicans BSI [5]. Although more children who died in our study had non-C. albicans BSI compared to those who survived, this difference was not statistically significant.
After adjusting for possible confounding, vasopressor therapy requirement, hepatic dysfunction and concomitant bacterial BSI during Candida BSI were significant risk factors associated with mortality within 30 days of Candida BSI diagnosis. To our knowledge, previous paediatric studies have not identified concomitant bacterial BSI as a risk factor. However, given that bacterial BSI itself is associated with appreciable mortality, concomitant bacterial BSI is likely to significantly increase the mortality risk during Candida BSI as suggested by our findings.
Study strengths and limitations
The results underline an important antimicrobial stewardship principle, namely that low fluconazole resistance in Candida BSI at our institutions implies that fluconazole should still be used for the empiric treatment of Candida BSI, thus preserving the echinocandins for the treatment of fluconazole-resistant isolates.
Due to the retrospective study design, bias was unavoidable due to limitations in the completeness and availability of laboratory and clinical data. The gestational ages of preterm infants were not available; thus, it was not possible to determine whether the incidence of Candida BSI was higher in extremely premature infants. Matrix assisted laser desorption ionization time of flight mass spectrometry (MALDI-ToF–MS) and reference microdilution methods were not available during the study period, limiting the characterisation of the fungal isolates. Additionally, because of few Candida BSI episodes at GSH & MMH our incidence risk calculations were confined to RCWMCH. Furthermore, the sample size was small and underpowered to fully explore risk factors associated with mortality within 30 days of Candida BSI diagnosis. Differences between our 30-day post-Candida BSI diagnosis mortality rate and higher rates documented in other sub-Saharan African studies suggest that our results may not be generalizable to other hospitals. Despite these limitations, our findings provide important insights into the epidemiology and clinical manifestations of paediatric Candida BSI at our institutions.
Conclusion
Our study provides a description of Candida BSI in children in the Western Cape province of South Africa, indicating low incidence, low fluconazole resistance and relatively low mortality. Vasopressor therapy requirement, hepatic dysfunction, and concomitant bacterial BSI were independent risk factors associated with mortality within 30 days of Candida BSI diagnosis. Further research, particularly prospective studies, is required to provide a complete understanding of the impact of Candida BSI on the childhood population in sub-Saharan Africa, including detailed molecular characterisation of the Candida isolates.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- aOR:
-
Adjusted odds ratio
- BSI:
-
Bloodstream infection
- CDW:
-
Central Data Warehouse
- CI:
-
Confidence interval
- CLSI:
-
Clinical and Laboratory Standards Institute
- CVC:
-
Central venous catheter
- GSH:
-
Groote Schuur Hospital
- GA:
-
Gestational age
- HAI:
-
Healthcare-associated infection
- HIV:
-
Human Immunodeficiency Virus
- HREC:
-
Human Research Ethics Committee
- ICU:
-
Intensive care unit
- IQR:
-
Interquartile range
- IPOA:
-
Infection present on admission
- LBW:
-
Low birth weight
- MMH:
-
Mowbray Maternity Hospital
- NHLS:
-
National Health Laboratory Service
- OR:
-
Odds ratio
- RCWMCH:
-
Red Cross War Memorial Children’s Hospital
- SA:
-
South Africa
- SD:
-
Standard deviation
- SAJID:
-
Southern African Journal of Infectious Diseases
- Sp.:
-
Species (singular tense)
- Spp.:
-
Species (pleural tense)
- TPN:
-
Total parenteral nutrition
- VLBW:
-
Very low birth weight
- WAZ:
-
Weight-for-age Z score
- WHO:
-
World Health Organization
References
Blyth CC, Chen SC, Slavin MA, Serena C, Nguyen Q, Marriott D, et al. Not just little adults: candidemia epidemiology, molecular characterization, and antifungal susceptibility in neonatal and pediatric patients. Pediatr. 2009;123(5):1360–8. https://doi.org/10.1542/peds.2008-2055.
Vogiatzi L, Ilia S, Sideri G, Vagelakoudi E, Vassilopoulou M, Sdougka M, et al. Invasive candidiasis in pediatric intensive care in Greece: a nationwide study. Intensive Care Med. 2013;39(12):2188–95. https://doi.org/10.1007/s00134-013-3057-y.
Shuping L, Mpembe R, Mhlanga M, Naicker SD, Maphanga TG, Tsotetsi E, et al. Epidemiology of culture-confirmed candidemia among hospitalized children in South Africa, 2012–2017. Pediatr Infect Dis J. 2021;40(8):730–7. https://doi.org/10.1097/INF.0000000000003151.
Lochan H, Pillay V, Bamford C, Nuttall J, Eley B. Bloodstream infections at a tertiary level paediatric hospital in South Africa. BMC Infect Dis. 2017;17:750. https://doi.org/10.1186/s12879-017-2862-2.
Khairat SM, Sayed AM, Nabih M, Soliman NS, Hassan YM. Prevalence of Candida blood stream infections among children in tertiary care hospital: detection of species and antifungal susceptibility. Infect Drug Resist. 2019;12:2409–16. https://doi.org/10.2147/IDR.S196972.
Richardson MD. Changing patterns and trends in systemic fungal infections. J Antimicrob Chemother. 2005;56(Suppl 1):i5–11. https://doi.org/10.1093/jac/dki218.
Krcmery V, Laho L, Huttova M, Ondrusova A, Kralinsky K, Pevalova L, et al. Aetiology, antifungal susceptibility, risk factors and outcome in 201 fungaemic children: data from a 12-year prospective national study from Slovakia. J Med Microbiol. 2002;51(2):110–6. https://doi.org/10.1099/0022-1317-51-2-110.
Santolaya ME, Alvarado T, Queiroz-Telles F, Colombo AL, Zurita J, Tiraboschi IN, et al. Active surveillance of candidemia in children from Latin America: a key requirement for improving disease outcome. Pediatr Infect Dis J. 2014;33(2):e40–4. https://doi.org/10.1097/INF.0000000000000039.
Hsu JF, Lai MY, Lee CW, Chu SM, Wu IH, Huang HR, et al. Comparison of the incidence, clinical features and outcomes of invasive candidiasis in children and neonates. BMC Infect Dis. 2018;18:194. https://doi.org/10.1186/s12879-018-3100-2.
Ding X, Yan D, Sun W, Zeng Z, Su R, Su J. Epidemiology, and risk factors for nosocomial non-Candida albicans candidemia in adult patients at a tertiary care hospital in North China. Med Mycol. 2015;53(7):684–90. https://doi.org/10.1093/mmy/myv060.
Wu Z, Liu Y, Feng X, Liu Y, Wang S, Zhu X, et al. Candidemia: incidence rates, type of species, and risk factors at a tertiary care academic hospital in China. Int J Infect Dis. 2014;22:4–8. https://doi.org/10.1016/j.ijid.2013.11.011.
Messer SA, Jones RN, Fritsche TR. International surveillance of Candida spp. and Aspergillus spp.: report from the SENTRY Antimicrobial Surveillance Program (2003). J Clin Microbiol. 2006;44(5):1782–7. https://doi.org/10.1128/JCM.44.5.1782-1787.2006.
Pfaller MA, Diekema DJ. Epidemiology of invasive candidiasis: a persistent public health problem. Clin Microbiol Rev. 2007;20(1):133–63. https://doi.org/10.1128/CMR.00029-06.
Fu J, Wang X, Wei B, Jiang Y, Chen J. Risk factors and clinical analysis of candidemia in very-low-birth-weight neonates. Am J Infect Control. 2016;44(11):1321–5. https://doi.org/10.1016/j.ajic.2016.03.026.
Ballot DE, Bosman N, Nana T, Ramdin T, Cooper PA. Background changing patterns of neonatal fungal sepsis in a developing country. J Trop Pediatr. 2013;59(6):460–4. https://doi.org/10.1093/tropej/fmt053.
Belet N, Ciftçi E, Aysev D, Guriz H, Uysal Z, Tacyildiz N, et al. Invasive Candida infections in children: the clinical characteristics and species distribution and antifungal susceptibility of Candida spp. Turk J Pediatr. 2011;53(5):489–98.
Clinical and Laboratory Standards Institute (CSLI). Reference Method for Broth Dilution Antifungal Susceptibility Testing of Yeasts; Fourth Informational Supplement. CLSI document M27-S4. (ISBN 1-56238-860-0 [Print]; ISSN 1-56238-864-9 [Electronic]). Clinical and Laboratory Standards Institute, 950 West Valley Road, Suite 2500, Wayne, Pennsylvania. 19087 USA, 2012.
National Healthcare Safety Newtwork. Identifying Healthcare-associated Infections (HAI) for NHSN Surveillance. 2022:2.1-2.29. https://www.cdc.gov/nhsn/pdfs/pscmanual/2psc_identifyinghais_nhsncurrent.pdf.
Schneider E, Whitmore S, Glynn MK, Dominguez K, Mitsch A, McKenna MT, et al. Revised surveillance case definitions for HIV infection among adults, adolescents, and children aged <18 months and for HIV infection and AIDS among children aged 18 months to <13 years—United States, 2008. MMWR Recomm Rep. 2008;57(RR10):1–12.
World Health Organization. Child growth standards, 2006. https://www.who.int/tools/child-growth-standards. Accessed 7 July 2019.
Phillips JR, Karlowitz MG. Prevalence of Candida species in hospital-acquired urinary tract infections in a neonatal intensive care unit. Pediatr Infect Dis J. 1997;16(2):190–4.
Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opel SM, et al. Surviving Sepsis Campaign Guidelines Committee including The Pediatric Subgroup. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock. Intensive Care Med. 2013;39(2):165–228. doi: https://doi.org/10.1007/s00134-012-2769-8.
Boer DP, de Rijke YB, Hop WC, Cransberg K, Dorresteijn EM. Reference values for serum creatinine in children younger than 1 year of age. Pediatr Nephrol. 2010;25(10):2107–13. https://doi.org/10.1007/s00467-010-1533-y.
Pottel H, Vrydags N, Mahieu B, Vandewynckele E, Croes K, Martens F. Establishing age/sex related serum creatinine reference intervals from hospital laboratory data based on different statistical methods. Clin Chim Acta. 2008;396(1–2):49–55. https://doi.org/10.1016/j.cca.2008.06.017.
Goldstein B, Giroir B, Randolph A. International Consensus Conference on Pediatric Sepsis. International pediatric sepsis consensus conference: definitions for sepsis and organ dysfunction in pediatrics. Pediatr Crit Care Med. 2005;6(1):2–8. https://doi.org/10.1097/01.PCC.0000149131.
Kaur H, Chakrabarti A. Strategies to reduce mortality in adult and neonatal candidemia in developing countries. J Fungi (Basel). 2017;3(3):41. https://doi.org/10.3390/jof3030041.
van Schalkwyk E, Iyaloo S, Naicker SD, Maphanga TG, Mbembe RS, Zulu TG, et al. Large outbreaks of fungal and bacterial bloodstream infections in a Neonatal Unit, South Africa, 2012–2016. Emerg Infect Dis. 2018;24(7):1204–12. https://doi.org/10.3201/eid2407.171087.
Hachem R, Hanna H, Kontoyiannis D, Jiang Y, Raad I. The changing epidemiology of invasive candidiasis: Candida glabrata and Candida krusei as the leading causes of candidemia in hematologic malignancy. Cancer. 2008;112(11):2493–9. https://doi.org/10.1002/cncr.23466.
Acknowledgements
We acknowledge Ms. Simone Twaku and the records department of RCWMCH, GSH & MMH for the provision of the medical files needed for retrospective review. We thank the NHLS and the CDW, housed in the information technology department of the NHLS in Johannesburg, for providing data on blood cultures and antimicrobial susceptibilities of patients from RCWMCH, GSH & MMH. We also acknowledge Mr. Ebrahim Jacobs, RCWMCH for providing denominator data for RCWMCH annual admissions
Funding
This research project received no specific grant from any funding agency in the public, commercial or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
MNG wrote the study protocol, extracted the clinical data from the medical files at RCWMCH, GSH and MMH, and the microbiology data from the NHLS database for microbiology, analysed the data, interpreted the results and wrote the initial draft of the manuscript. BE developed the concept and provided guidance on the title, objectives and the development of the protocol of the study and the study literature review, data analysis, and manuscript development. JN assisted with the study protocol and manuscript development. WB provided guidance on the statistical analysis, assisted with the regression and Kaplan–Meier analyses and manuscript writing. HT and AK helped describe the microbiology methods and retrieval of patient list and microbiology results from the CDW and the NHLS microbiology database, LT, SS, RM and NR helped with the protocol development and retrieval of the clinical records of patients in their respective units. All authors reviewed and approved the final draft.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Human Research Ethics Committee (HREC), Faculty of Health Sciences, University of Cape Town, reference number: HREC REF 159/2020 and the RCWMCH research committee. Furthermore, the study was completed in accordance with the Declaration of Helsinki. Since the data was collected retrospectively, the HREC waived the need for informed consent. Patient details were anonymised before data analysis.
Consent for publication
Not applicable in this section.
Competing interests
Authors declare that they have no financial or personal relationships that may have inappropriately influenced them in writing this article.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Annual change in incidence risk per 1000 hospital admissions of Candida bloodstream infection episodes at Red Cross War Memorial Children’s Hospital, 2015-2019.
Additional file 2: Table S2.
Spectrum of bacterial isolates causing concomitant bacterial BSI and their antibiotic susceptibility patterns during Candida BSI.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Gebremicael, M.N., Nuttall, J.J.C., Tootla, H.D. et al. Candida bloodstream infection among children hospitalised in three public-sector hospitals in the Metro West region of Cape Town, South Africa. BMC Infect Dis 23, 67 (2023). https://doi.org/10.1186/s12879-023-08027-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-023-08027-z