Abstract
Background
Legionella-related community acquired pneumonia (CAP) is a disease with an increasing incidence and a high mortality rate, especially if empirical antibiotic therapy is inadequate. Antibiotic treatment highly relies on clinical symptoms, although proven non-specific, because currently available diagnostic techniques provide insufficient accuracy for detecting Legionella CAP on admission. This study validates a diagnostic scoring system for detection of Legionella-related CAP, based on six items on admission (Legionella prediction score).
Methods
We included patients with Legionella-related CAP admitted to five large Dutch hospitals between 2006 and 2016. Controls were non-Legionella-related CAP patients. The following six conditions were rewarded one point if present: fever > 39.4 °C; dry cough; hyponatremia (sodium) < 133 mmol/L; lactate dehydrogenase (LDH) > 225 mmol/L; C-reactive protein (CRP) > 187 mg/L and platelet count < 171 × 109/L. The accuracy of the prediction score was assessed by calculating the area under the curve (AUC) through logistic regression analysis.
Results
We included 131 cases and 160 controls. A score of 0 occurred in non-Legionella-related CAP patients only, a score of 5 and 6 in Legionella-related CAP patients only. A cut-off ≥ 4 resulted in a sensitivity of 58.8% and a specificity of 93.1%. The AUC was 0.89 (95% CI 0.86–0.93). The strongest predictors were elevated LDH, elevated CRP and hyponatremia.
Conclusions
This multi-centre study validates the Legionella prediction score, an easily applicable diagnostic scoring system, in a large group of patients and finds high diagnostic accuracy. The score shows promise for future prospective validation and could contribute to targeted antibiotic treatment of suspected Legionella CAP.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Legionella infection is an important cause of community-acquired pneumonia (CAP) with a mortality of 8–12% [1]. The average incidence of Legionella infection in CAP was reported 2.1–3.6% in a recent meta-analysis [2]. However, due to underdiagnosis, the true incidence is probably higher. In the USA, the incidence of reported Legionella cases quadrupled over the past decades [3,4,5,6]. Legionella-related pneumonia has an overall higher burden of morbidity and mortality than other causes of CAP, especially if initial empirical antibiotic therapy is inadequate [3, 5, 7, 8].
Diagnosis of Legionella-related CAP is difficult, because culturing Legionella from sputum and blood takes 3 to 10 days and has a low yield. The introduction of the urinary antigen test (UAT) for Legionella pneumophila improved diagnosis, especially in severe cases. However, the UAT can be negative in the early phase of the disease, especially in patients with mild disease. UAT detects only Legionella pneumophila serogroup 1 antigens, accounting for more than 80% of Legionella cases [9,10,11]. Over the last years several other subspecies of Legionella have been associated with significant clinical disease, especially Legionella longbeachae which is predominantly found in Australia, New Zealand and Asia, but recently has been detected in both USA and Europe [12,13,14].
To prevent overuse of macrolides and quinolones, international guidelines recommend empirical antibiotic coverage of Legionella only when this infection is suspected based on clinical signs and symptoms, or in patients with severe CAP. Clinical scoring systems were developed to predict Legionella-related pneumonia, but most have limited clinical significance because of low accuracy or the need to include follow-up data over several days [15,16,17]. As a result initial empirical coverage may be inadequate [18,19,20].
Fiumefreddo et al. [21] developed a diagnostic scoring system consisting of 6 items which are easily obtainable on admission, namely fever, dry cough, hyponatremia, elevated lactate dehydrogenase (LDH) and elevated C-reactive protein (CRP), further called: Legionella prediction score. In the derivation cohort, the diagnostic accuracy of the score was high, with an area under the curve (AUC) of 0.86 (95% confidence interval (CI) 0.81–0.90) [21]. In a previous validation study with 37 cases, the Legionella prediction score discriminated reasonably well between Legionella-related CAP and CAP caused by other pathogens (specificity 92% and sensitivity 31% at cut off ≥ 4, area under the curve 0.91) [22].
In theory this prediction score could be a useful clinical tool to limit antibiotic overuse in selected patients, especially in cases that are not detected by UAT, due to a false-negative result, when UAT takes too long or it has not been performed. Therefore, we evaluated the performance of this score through external validation in a large, Dutch cohort of hospital-admitted patients with Legionella-related CAP.
Methods
Patients and materials
In this cross-sectional, observational, retrospective study, data was collected from four large teaching hospitals and one University hospital in the Netherlands. A list of all patients tested positive with Legionella species between 2006 and 2016 was provided by the departments of microbiology. Medical records of all patients were reviewed and data was collected anonymously. Cases had at least one microbiological test positive for Legionella species, either culture, serology, PCR or UAT and consolidation(s) of the chest X-ray. UATs were performed with the BinaxNOW S. pneumoniae Antigen Card (Abbott). Our control group consisted of non-Legionella CAP-patients who required hospital admission, through random selection of participants from the REDUCE study, which was conducted in one of the previously mentioned teaching hospitals from 2013–2017 (full study protocol available via clinicaltrials.gov, NCT01964495). All patients included in the study had at least one consolidation on the chest X-ray together with clinical signs and symptoms indicative for CAP. Other inclusion criteria were a (pre-event) life expectancy of minimum 30 days and granted informed consent. Patients were excluded if they were pregnant or breastfeeding, if they had immunodeficiency (known immunodeficiency or receiving corticosteroids equivalent to 10 mg prednisolone per day), cancer, in case of obstruction, aspiration or hospital acquired pneumonia and if they were unable or unlikely to comprehend and follow the REDUCE protocol. Patients were included in the analysis if the items needed to calculate the Legionella prediction score were present. When available, causative pathogens for non-Legionella CAP were reported. Causative pathogens were defined as pathogens known to cause CAP, that were isolated from blood cultures, sputum cultures of good quality sputum (predominant leukocytes without squamous epithelial cells), urinary antigen tests and/or PCR. We retrospectively collected data from patient files which were anonymized for our study before processing the data. Therefore, in accordance to the current guidelines at that time in the Netherlands, informed consent was not required, neither was approval by a local ethics committee. This conforms to the Law regarding Medical Research involving human subjects in the Netherlands.
Data and Legionella prediction score
The collected data included vital parameters, clinical signs, laboratory findings, relevant comorbidities, smoking history and CURB-65 score. All data was obtained during the emergency care department visit (further called: on admission). The Legionella prediction score, ranging from 0–6, was calculated. For the six following conditions, if present, one point was scored: fever > 39.4 °C; dry cough; hyponatremia (sodium) < 133 mmol/L; LDH > 225 mmol/L; high CRP > 187 mg/L and low platelet count < 171 × 109/L [21].
Outcomes
The primary outcome was the diagnostic accuracy of the Legionella prediction score for Legionella-related CAP. Furthermore, we assessed the predictive value of the original, continuous parameters and the proposed cut-off points, both univariate and multivariate.
Statistical analysis
According to Toll et al., for validation of a prediction rule with a dichotomous outcomes, at least 100 cases and 100 controls are needed [23]. We estimated that a random selection of 185 REDUCE participants would provide sufficient controls. Patient characteristics were assessed for normal distribution with the Kolmogorov–Smirnov test. Either mean, standard deviation and Chi-square test or median, percentiles and Mann–Whitney-U test were reported.
Continuous parameters were analysed in a logistic regression model that was performed for each individual parameter and for all parameters combined. Thereafter, parameters were dichotomized in the categories used in the prediction score. Univariate and multivariate logistic regression was repeated with these dichotomized parameters.
For each regression, the b-coefficient, the odds ratio, AUC and p were calculated. A p-value < 0.05 was considered significant. Sensitivity, specificity, positive and negative predictive values were calculated for scores 0–6 of the prediction score.
To further assess accuracy, chi-square, the loglikelihood ratio and Nagelkerke square were calculated. IBM SPSS Statistics version 25.0 was used for all analyses.
Results
We identified 252 patients with Legionella-related CAP and 185 patients with non-Legionella related CAP. Of 252 patients with Legionella, 131 had complete data and were included. Of non-Legionella patients, 160 were included as controls (Fig. 1). Baseline characteristics are summarized in Table 1. Patients with Legionella were often male, relatively younger, had less comorbidities (such as COPD and cancer), but were more frequently active smokers. Of cases, 126 (96%) were confirmed by UAT and 29 (22%) were confirmed by sputum PCR or culture. In the control group, the most frequently detected pathogens were Streptococcus pneumoniae (18.8%), Staphylococcus aureus (10.1%) and Haemophilus influenzae (8.1%). A further specification of pathogens in the control group is available in Table 2.
Flow chart of inclusion and exclusion. Patients were excluded if items needed to calculate the Legionella prediction score could not be obtained. These items are: temperature, dry cough, sodium, LDH, CRP and platelets. CAP community acquired pneumonia, LDH lactate dehydrogenase, CRP C-reactive protein
In univariate regression of the original values (Table 3), all six predictors were significantly associated with Legionella-related CAP. The strongest predictors were sodium, CRP and LDH levels (AUC respectively 0.76, 0.80 and 0.93). In multivariate regression, this association persisted for all parameters except for dry cough. The AUC of the multivariate model of these variables was 0.96 (95% CI 0.94–0.98).
In Table 4 all variables were expressed as dichotomous parameters. In univariate analysis again, all predictive values were statistically significant. The strongest predictors were hyponatremia < 133 mmol/L, elevated CRP > 187 mg/L and elevated LDH > 225 mmol/L (AUC respectively 0.71, 0.75 and 0.81). In the multivariate model, dry cough was a significant predictor. Fever above 39.4 °C and platelets below 171 × 109/L were not significant predictors. The AUC of the complete dichotomic multivariate model was 0.89 (95% CI 0.86–0.93).
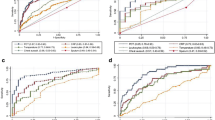
As shown in Fig. 2, a prediction score of 0 only occurred in non-Legionella-related CAP patients. Above, the number of cases gradually increased per score point. A prediction score of 5 or 6 points was only found in Legionella-related CAP patients (specificity 100%). The prediction score detected Legionella with a specificity of 93.1% and a sensitivity of 58.8% when a cut-off ≥ 4 was chosen. A cut-off ≥ 2 resulted in a sensitivity of 98.5% and a specificity of 50.6%. Figure 3 illustrates the receiver operating characteristics curve (ROC-curve) of the individual predictors and of the prediction score.
ROC-curve of individual parameters and Legionella predictive score. This figure shows the ROC-curve of the individual parameters, analyzed as continuous values. Furthermore, it shows the ROC-curve of the diagnostic scoring system, which is calculated by dichotomizing the individual parameters, followed by multivariate regression analysis. ROC-curve receiver operating curve, AUC area under the curve, LDH lactate dehydrogenase, CRP C-reactive protein
Discussion
Legionella-related CAP is a disease with a high mortality rate and increasing incidence [1,2,3,4,5,6]. It requires targeted antibiotic treatment, in an era where antibiotic resistance is rising and antibiotic stewardship is important. Although clinical symptoms of Legionella prove non-specific [15], they can be a decisive factor in the treatment choice on admission [18,19,20]. This retrospective study further validated a prediction score based on six clinical parameters, that can be applied easily on admission, and found a high accuracy with an AUC of 0.89 (95% CI 0.86–0.93). We demonstrated that this score can potentially be used to rule-in or rule-out Legionella CAP, depending on the cut-off point chosen. Therefore, in patients presenting with mild to moderate disease symptoms, it could be applied both for early identification and specific treatment of those infected with Legionella, in particular in cases that are not detected by UAT. The negative predictive value of the score will likely be higher in an unselected population of hospital admitted CAP patients, since the incidence of Legionella is lower than in our population.
All predictors were associated significantly with the outcome. However, temperature and platelets were no significant predictors in the multivariate analysis after dichotomization. Assumably, this can be explained by the wide range in which these variables occurred in both patients with Legionella CAP and with non-Legionella CAP.
Our study yielded an accuracy similar to that found by a Spanish study (AUC 0.86 (95% CI 0.81–0.90)), based on 82 cases [21]. It was higher than in a previous multinational validation study, which found an AUC of 0.73 (95% CI 0.65–0.81) [22]. This difference can be explained by a smaller sample size (37 cases). Baseline differences between the cases and controls (age, COPD and smoking) in our study were similar to both other studies [22]. This was not the case in a Japanese validation study published in 2017, in which participants were more often male and that also included patients with cancer [24]. They found a sensitivity of 94% and a specificity of 49% at a cut-off ≥ 2, resembling our present study.
In the literature two other diagnostic scoring systems for Legionella-related CAP were proposed, namely the Winthrop University score and the Community-Based Pneumonia Incidence Study Group scoring system. These two scoring systems were validated, but found unsuitable for diagnosing or excluding Legionella in a clinical setting, due to low accuracy [16, 17, 24, 25].
A Japanese study group recently proposed a variation on the Legionella prediction score, which includes dyspnoea and gender instead of on temperature and platelets. This score performed well (AUC 0.93) in a Japanese validation cohort. However, in study populations outside Japan, male gender and dyspnoea were not identified as risk factors for Legionella-related CAP. Therefore this score may be less relevant [26].
This multi-centre study included a large number of patients with Legionella-related CAP. The number of participants considerably exceeds the number that is due sufficient for validation of a prediction score with a dichotomous outcome, according to Toll et al. [23]. All hospital admitted patients with CAP were eligible for inclusion and data was collected from five different large hospitals with a wide geographical spread. This adds to the external validity of the study because it closely resembles a real-life clinical population. We chose to only include patients with complete data, so imputation of missing data could be avoided which adds on to the internal validity of the study. However, this has the potential to introduce some sort of selection bias but given the large sample of patients we believe the effect of this potential bias is likely small.
A weak point of this study is that its retrospective. Missing data on occurrence of especially (dry) cough lead to many exclusions. In a prospective study setting, this parameter would be easy to obtain. Furthermore, cases were retrospectively selected, based on positive microbiological tests. Mostly, this was the UAT, which does not detect species other than Legionella pneumophila serogroup 1. Because cultures and PCR have not been performed in all participants, some Legionella cases might have been missed. This could potentially influence the performance of the score. A Japanese study demonstrated a better performance of the Legionella prediction score for Legionella serogroup 1 (N = 11) than for other Legionella species (n = 23) [27]. This suggests that the score is particularly useful for detecting Legionella serogroup 1, which was detected in 96% of the cases in the present study.
Future research should validate the diagnostic scoring system prospectively, preferably in an unselected CAP population, in which Legionella is detected via UAT, PCR and cultures. This research could also analyse the accuracy of the scoring system, give more insight into performance of the score over the course of the disease, mild versus advanced disease, and investigate its clinical significance in addition to UAT. Moreover, longitudinal studies on clinical outcomes resulting from implementation of the test, such as change in antibiotic prescriptions, mortality, ICU admissions and of length of stay in the hospital, are needed.
Conclusion
This six-items prediction score detects Legionella related CAP infections with a high specificity of 93.1% (sensitivity 58.8%) in patients who score positive for at least four items. It is easy to implement in day to day practice with data readily available in every CAP patient and. Overall, based on our data and previous studies we believe it shows promise for further prospective validation and could contribute to targeted antibiotic treatment of Legionella-related CAP.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- ALAT:
-
Alanine transaminase
- AP:
-
Alkaline phosphatase
- ASAT:
-
Aspartate transaminase
- AUC:
-
Area under the curve
- BPM:
-
Beats per minute
- CAP:
-
Community-acquired pneumonia
- CI:
-
Confidence interval
- COPD:
-
Chronic obstructive pulmonary disease
- CRP:
-
C-reactive protein
- GGT:
-
Gamma-glutamyltransferase
- IQR:
-
Interquartile range
- LDH:
-
Lactate dehydrogenase
- OR:
-
Odds ratio
- PCR:
-
Polymerase chain reaction
- ROC-curve:
-
The receiver operating characteristics curve
- UAT:
-
Urinary antigen test
References
Phin N, Parry-ford F, Harrison T, Stagg HR, Zhang N, Kumar K, Lortholary O, Zumla A, Abubakar I. Epidemiology and clinical management of Legionnaires’ disease. Lancet Infect Dis. 2014;14:1011–21.
Marchello C, Dale AP, Thai TN, Han DS, Ebell MH. Prevalence of atypical pathogens in patients with cough and community-acquired pneumonia: a meta-analysis. Ann Fam Med. 2016;14:552–66.
Stout JE, Yu VL. Legionellosis. N Engl J Med. 1997;337:682–7.
Fang G-D, Fine M, Orloff J, Arisumi D, Yu VL, Kapoor W, Grayston JT, Wang SP, Kohler RB, Muder RR, Yee YC, Rihs JD, Vickers RM. New and emerging etiologies for community-acquired pneumonia with implications for therapy. Medicine (Baltimore). 1990;69:307–16.
Shah P, Barskey A, Binder A, Edens C, Lee S, Smith J, Whitney C, Cooley L, Cooley L. Legionnaires’ disease surveillance summary report, United States—2014 and 2015. 2018. https://www.cdc.gov/legionella/health-depts/surv-reporting/2014-15-surv-report-508.pdf. Accessed 1 Feb 2021.
Herwaldt LA, Marra AR. Legionella: a reemerging pathogen. Curr Opin Infect Dis. 2018;31:325–33.
Falco V, De Sevilla TF, Alegre J, Ferrer A, Vazquez JMM. Legionella pneumophila; a cause of severe community-acquired pneumonia. Chest. 1991;100:1007–11.
Gacouin A, Le Tulzo Y, Lavoue S, Camus C, Hoff J, Bassen R, Arvieux C, Heurtin C, Thomas R. Severe pneumonia due to Legionella pneumophila: prognostic factors, impact of delayed appropriate antimicrobial therapy. Intensive Care Med. 2002;28:686–91.
Okada C, Kura F, Wada A, Inagawa H, Lee GH, Matsushita H. Cross-reactivity and sensitivity of two Legionella urinary antigen kits, biotest EIA and binax NOW, to extracted antigens from various serogroups of L. pneumophila and other Legionella species. Microbiol Immunol. 2002;46:51–4.
Kohler RB, Winn WC, Wheat LJ. Onset and duration of urinary antigen excretion in Legionnaires disease. J Clin Microbiol. 1984;20:605–7.
European Centre for Disease Prevention and Control. Legionnaires’ disease. In: ECDC. Annual epidemiological report for 2018. Stockholm; 2020.
van Heijnsbergen E, van Deursen A, Bouwknegt M, Bruin JP, de Roda Husman AM, Schalk JAC. Presence and persistence of viable, clinically relevant Legionella pneumophila bacteria in garden soil in the Netherlands. Appl Environ Microbiol. 2016;82:5125–31.
Isenman HL, Chambers ST, Pithie AD, MacDonald SLS, Hegarty JM, Fenwick JL, Maze MJ, Metcalf SCL, Murdoch DR. Legionnaires’ disease caused by Legionella longbeachae: clinical features and outcomes of 107 cases from an endemic area. Respirology. 2016;21:1292–9.
Picard-Masson M, Lajoie É, Lord J, Lalancette C, Marchand G, Levac É, Lemieux MA, Hudson P, Lajoie L. Two related occupational cases of Legionella longbeachae infection, Quebec, Canada. Emerg Infect Dis. 2016;22:1289–91.
Mulazimoglu L, Yu VL. Can Legionnaires disease be diagnosed by clinical criteria? A critical review. Chest. 2001;120:1049–53.
Fernández-Sabé N, Rosón B, Carratalà J, Dorca J, Manresa F, Gudiol F. Clinical diagnosis of Legionella pneumonia revisited: evaluation of the Community-Based Pneumonia Incidence Study Group scoring system. Clin Infect Dis. 2003;37:483–9.
Gupta SK, Imperiale TF, Sarosi GA. Evaluation of the Winthrop-University Hospital criteria to identify Legionella pneumonia. Chest. 2001;120:1064–71.
Lim WS, Baudouin SV, George RC, Hill AT, Jamieson C, Le Jeune I, Macfarlane JT, Read RC, Roberts HJ, Levy ML, Wani M, Woodhead MA. BTS guidelines for the management of community acquired pneumonia in adults: update 2009. Thorax. 2009;64:iii1–55.
Wiersinga WJ, Bonten MJ, Boersma WG, Jonkers RE, Aleva RM, Kullberg BJ, Schouten JA, Degener JE, van de Garde EMW, Verheij TJ, Sachs APE, Prins JM. Management of community-acquired pneumonia in adults: 2016 guideline update from the Dutch Working Party on Antibiotic Policy (SWAB) and Dutch Association of Chest Physicians (NVALT). Neth J Med. 2018;76:4–13.
Mandell LA, Wunderink RG, Anzueto A, Bartlett JG, Campbell GD, Dean NC, Dowell SF, File TM, Musher DM, Niederman MS, Torres A, Whitney C. Infectious Diseases Society of America/American Thoracic Society Consensus Guidelines on the Management of Community-Acquired Pneumonia in adults. Clin Infect Dis. 2007;44:S27-72.
Fiumefreddo R, Zaborsky R, Haeuptle J, Christ-Crain M, Trampuz A, Steffen I, Frei R, Müller B, Schuetz P. Clinical predictors for Legionella in patients presenting with community-acquired pneumonia to the emergency department. BMC Pulm Med. 2009;9:1–9.
Haubitz S, Hitz F, Graedel L, Batschwaroff M, Wiemken TL, Peyrani P, Ramirez JA, Fux CA, Mueller B, Schuetz P. Ruling out Legionella in community-acquired pneumonia. Am J Med. 2014;127:1010.e11-1010.e19.
Toll DB, Janssen KJM, Vergouwe Y, Moons KGM. Validation, updating and impact of clinical prediction rules: a review. J Clin Epidemiol. 2008;61:1085–94.
Miyashita N, Higa F, Aoki Y, Kikuchi T, Seki M, Tateda K, Maki N, Uchino K, Ogasawara K, Kiyota H, Watanabe A. Clinical presentation of Legionella pneumonia: evaluation of clinical scoring systems and therapeutic efficacy. J Infect Chemother. 2017;23:727–32.
Cunha BA. Clinical features of Legionnaires’ disease. Semin Respir Infect. 1998;13:116–27.
Miyashita N, Horita N, Higa F, Aoki Y, Kikuchi T, Seki M, Tateda K, Maki N, Uchino K, Ogasawara K, Kiyota H, Watanabe A. Validation of a diagnostic score model for the prediction of Legionella pneumophila pneumonia. J Infect Chemother. 2019;25:407–12.
Ito A, Ishida T, Washio Y, Yamazaki A, Tachibana H. Legionella pneumonia due to non-Legionella pneumophila serogroup 1: usefulness of the six-point scoring system. BMC Pulm Med. 2017;17:1–9.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
All authors contributed to data collection. RB and RD analysed the data and wrote the manuscript. WB supervised the project. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
No permission by the medical ethical board was required for this retrospective study.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Beekman, R.R.A.L., Duijkers, R.R., Snijders, D.D. et al. Validating a clinical prediction score for Legionella-related community acquired pneumonia. BMC Infect Dis 22, 442 (2022). https://doi.org/10.1186/s12879-022-07433-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-022-07433-z