Abstract
Background and aim
For over 40 years of the HIV/AIDS global epidemic, no effective cure nor vaccine is yet available, making the current control strategies focused on curbing new infections through risk reduction. The study aimed to determine the prevalence of HIV risk factors and their associated socio-demographics among women of reproductive age in Sierra Leone.
Methods
We used weighted data from the Sierra Leone Demographic and Health Survey (SLDHS) of 2019 for 12,005 women aged 15–49 years. Multistage sampling was used to select study participants. Exposure to HIV risk factors was considered if a woman reported at least one of the following; having multiple sexual partners, transactional sex, non-condom use for the unmarried, and having other sexually transmitted infections (STIs). We, then, conducted multivariable logistic regression to explore the associated socio-demographics. All the analyses were done using SPSS (version 25).
Results
Of the 12,005 women, 38.1% (4577/12005) (95% confidence interval (CI) 37.3–39.0) had at least one of the four risk factors. Women of 15 to 19 years (adjusted odds ratio (AOR) = 1.34, 95% CI 1.00–1.80) and 20 to 34 years (AOR = 1.25, 95% CI 1.05–1.49) had more odds of having HIV risk factors compared to those of 35 to 49 years. Urban residents (AOR = 1.49, 95% CI 1.17–1.89) and those from the Northwestern region (AOR = 1.81, 95% CI 1.26–2.60) were also more likely to encounter HIV risk factors compared to their respective counterparts. Moreover, unmarried women (AOR = 111.17, 95% CI 87.55–141.18) and those working (AOR = 1.38, 95% CI 1.14–1.67) also had higher odds of having HIV risk factors, compared to their respective counterparts. Sex of household head and parity were also significant associates.
Conclusions
More than a third of women in Sierra Leone had encountered at least one HIV risk factor, and this was associated with age, place of residence, region, marital status, working status, household head and parity. There is a need for strengthening HIV/AIDS education programs, laws and policies targeting the young, working, unmarried and urban-resident women.
Similar content being viewed by others
Introduction
Over 40 years since its identification, the human immunodeficiency virus (HIV) is still a global public health concern and one of the major causes of death, especially in developing countries [1]. According to a recent Joint United Nations Programme on HIV/AIDS (UNAIDS) report, over 37 million people globally were living with HIV in 2020, 1.5 million became infected and close to 1 million died due to acquired immunodeficiency syndrome (AIDS) related illnesses [1]. Africa still shares the biggest burden of HIV/AIDS, whereby over two-thirds of people living with HIV globally are found in sub-Saharan Africa [2].
In Sierra Leone, a small low-income West African country with a population size of around 8 million, the prevalence of HIV is around 1.7%, with a higher burden in Freetown- the capital [3,4,5]. Like in other countries, the key population groups in Sierra Leone include female sex workers, their partners and clients, long-distance truck drivers, members of the fishing community, men who have sex with men, transgender people, uniformed armed personnel, prisoners, and people who inject drugs (PWID), among others [3, 5]. Moreover, often the under-looked vulnerable group are the women; HIV/AIDS is shown to disproportionately affect women, where they account for more than half (55%) of people living with HIV/AIDS globally [2]. A similar trend has also been reported in Sierra Leone with women having a higher HIV prevalence than men (1.8% vs 1.3%) [6]. Besides the known risk of mother to child transmission, HIV/AIDS is also reported to have other adverse pregnancy complications [7] and is the leading cause of death among women of reproductive age [8]. In sub-Saharan Africa, the disproportionate burden of HIV/AIDS among women is attributed to lack of power, early marriages, coerced first sex, limited access to reproductive health services, extreme poverty, sexual violence, wars and conflict [9, 10].
Generally, several studies have explored the epidemiological characteristics of HIV/AIDS in Sierra Leone, with some studies focusing on HIV prevalence, testing and associated factors [6, 11,12,13,14,15,16,17], or other aspects [18]. These studies have focused mainly on the general population [6, 12, 15,16,17,18], military personnel [11], adolescents [13] and some other key population groups [14], but not women. Moreover, several factors/behaviours have been documented in Sierra Leone and elsewhere to increase the risk of HIV, which include; having multiple sexual partners, other sexually transmitted infections (STIs), inconsistent condom use, engaging in transactional sex, alcohol and drug use before/during sex, among others [11, 13, 19,20,21,22].
Given the considerable vulnerability of women to HIV/AIDS, we, therefore, aimed to determine the burden, in terms of prevalence, of HIV risk factors and their associated socio-demographics among women of reproductive age in Sierra Leone, using a nationwide dataset. We hypothesized that several socio-demographic characteristics are associated with HIV risk factors/behaviours. Thus establishing the magnitude of these risk factors and their associates would be vital in informing targeted interventions to address this global epidemic.
Methods
Study design and sampling methods
The Sierra Leone Demographic and Health Surveys (SLDHS) are cross-sectional surveys that are periodically conducted to obtain information on demographic, health and nutritional indicators of non-elderly adults and children. The latest survey was conducted over 4 months between May 2019 and August 2019 [5]. This national survey used a stratified, two-stage cluster sampling design with the first stage having 578 enumeration areas (EAs) (214 urban and 364 rural) selected leading to 13,872 households [5]. Using interviewer-administered questionnaires, the survey obtained sociodemographic information about the respondents. A detailed explanation of the sampling process is available elsewhere [5]. Women aged 15–49 years who were either permanent residents or visitors who had stayed in the selected households the night before the survey were eligible for interviews with a total of 15,574 women being interviewed. Of these, a weighted sample of 12,005 had been sexually active within 12 months preceding the survey and was included in this secondary analysis as shown in Table 1. Written informed consent was provided by all participants of the survey. Written permission to access the whole SLDHS database was obtained through the DHS program website [23].
Variables of the study
Dependent variable
Four variables from the SLDHS were used in this study to measure the risk factors for HIV and these included; (1) engaging in sex with more than one partner in the past 12 months, (2) engaging in transactional sex in the past 12 months, (3) not using a condom during the most recent intercourse for those who were not married, and (4) having had a sexually transmitted infection in the past 12 months [19, 20]. The total number of risk factors per woman was not a variable in the SLDHS but was generated by first giving a score of 1 for every exposure to an HIV risk factor and a score of 0 for every non-exposure, and then summing up the scores for each woman. The minimum possible score is 0 while the maximum possible score is 4. Exposure to any of the four risk factors for HIV was categorized as a binary (Yes/No) outcome and women were considered to have been exposed to risk factors for HIV if they reported any of the four behaviours. The use of alcohol/being drunk during the last sexual intercourse was not included because the data was not available in the SLDHS data set.
Independent variables
Nineteen explanatory variables were used and included: Maternal age (15–19 years, 20–34 years and 35–49 years), Wealth index (poorest, poorer, middle, richer and richest quintiles), place of residence (urban and rural), region (Northern, Eastern, Southern, Western and Northwestern), level of education (no education, primary education, and post-primary education), household size (less than seven members and seven and above members), sex of household head (male or female), working status (not working and working), marital status (married including those in formal and informal unions, and not married). Religion was categorised as Muslims and Christians and others, problems seeking permission and distance to health facility were categorised as a big problem and no big problem while exposure to mass media was categorised as yes and no (if exposed to any of TV, radio, internet and newspapers), and visited by field worker or visited a health facility were categorised as yes and no, parity (less than 2, 2–4 and 5 and above). Wealth quintiles (poorest, poorer, middle, richer and richest) are a measure of relative household economic status and were calculated from household asset ownership information using Principal Component Analysis [5]. According to Sierra Leone, an urban area is a town with 2000 inhabitants or more [24].
Statistical analysis
The study first presented descriptive statistics of the background characteristics and risk factors of HIV of the study sample. This study first examined the proportion of women that reported ever engaging in risk factors for HIV and then examined the factors associated with these risk factors. Bivariable and multivariable logistic regression analyses were conducted where variables found significant at p-value less than 0.25 in the bivariable analysis and not strongly collinear with other independent variables were included as candidate variables in the multivariable model [25]. Multi-collinearity was assessed using variance inflation factor (VIF) and wealth index was excluded in the multivariable model because it had VIFs above 3 with marital status, age, working, exposure to newspapers, internet, parity and problems with distance and seeking permission to healthcare. Hosmer and Lemeshow test was finally done to test the goodness of the multivariable regression model. Analysis was carried out based on the weighted count to account for the unequal probability sampling in different strata and to ensure the representativeness of the survey results at the national and regional levels. In order to account for the multi-stage cluster study design, we used SPSS (version 25.0) statistical software complex samples package incorporating the following variables in the analysis plan to account for the multistage sample design inherent in the DHS dataset: individual sample weight, sample strata for sampling errors/design, and cluster number [26,27,28]. Adjusted odds ratios (AOR), 95% confidence intervals (CI) and p-values were calculated with statistical significance level set at p-value < 0.05.
Results
Sociodemographic characteristics of study participants
In this study, a weighted sample of 12,005 women was used as shown in Table 1. The majority of women were aged 20–34 years (51.8%), had visited a health facility within 12 months preceding the survey (56.2%), working (73.9%), Muslims (76.6%), resided in rural areas (55.4%), no education (48.6%) and were married (70.8%). Most women had no exposure to mass media with 92.1%, 84.7%, 72.1% and 53.9% not being exposed to newspapers/magazines, internet, TV, and Radio respectively.
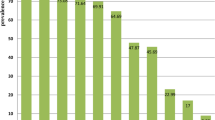
Out of the 12,005 women, 3289 (27.4%, 95% CI 26.6–28.2) were unmarried and had not used condom for their most recent sexual intercourse, 1490 (12.4%, 95% CI 11.9–13.1) had a sexually transmitted infection, 580 (4.8%, 95% CI 4.4–5.2) had multiple sexual partners, 154 (6.6%, 95% CI 5.5–7.4) had transactional sex and 4577 (38.1%, 95% CI 37.3–39.0) had any of the four risk factors as shown in Table 2. Additional file 1 shows how many women had one, two, three or four HIV risk factors.
Factors associated with risk factors for HIV
Results of regression analyses are detailed in Table 3. After adjusting for other factors, age, residence, region, sex of household head, working status, marital status and parity remained significantly associated with HIV risk factors.
Women of 15 to 19 years (AOR = 1.34, 95% CI 1.00–1.80) and those of 20 to 34 years (AOR = 1.25, 95% CI 1.05–1.49) were respectively, 34% and 25% more likely to have HIV risk factors compared to those of 35 to 49 years of age. Urban residents were 49% more likely to encounter HIV risk factors (AOR = 1.49, 95% CI 1.17–1.89). Compared to women in the Western region, those from the South were 33% less likely (AOR = 0.67, 95% CI 0.50–0.90) while those in the Northwest were 81% more likely (AOR = 1.81, 95% CI 1.26–2.60) to have HIV risk factors. Moreover, women from female-headed households (AOR = 1.22, 95% CI 1.03–1.44), and those working (AOR = 1.38, 95% CI 1.14–1.67) were 22% and 38% respectively, more likely to have HIV risk factors, compared to their respective counterparts. Marital status was strongly associated with HIV risk factors; whereby unmarried women were over 111% (AOR = 111.17, 95% CI 87.55–141.18) more likely to have HIV risk factors. In addition, women with parity of 0–1 (AOR = 1.32, 95% CI 1.01–1.72) and 2–4 (AOR = 1.26, 95% CI 1.01–1.57) were 32% and 26% more likely have HIV risk factors, respectively as shown in Table 3.
Discussion
We conducted a secondary analysis of SLDHS data to estimate the prevalence of HIV risk factors and their socio-demographic associates among women of reproductive age in Sierra Leone. In this study, four factors were considered as potential HIV risk factors, including; non-condom use at last sexual intercourse for unmarried women, engaging in transactional sex, having other sexually transmitted infections (STIs), and having multiple sexual partners. To our knowledge, this is the first study to focus on the burden of HIV risk factors in Sierra Leone.
The study results showed that 38% of the women had encountered at least one of the four risk factors, 27% had non-condom use (the unmarried), 12% had other STIs, while less than 10% had engaged in transactional sex and had multiple sex partners. Although no immediate similar study to compare our results with, the overall prevalence of such risk factors is of significant impact in a low-income country with a high burden of other infectious diseases coupled with a weak health system [3]. Moreover, there is also a lower rate of HIV testing and antiretroviral treatment notably even among pregnant women living with HIV (less than 60%) in Sierra Leon [29]. Although the country currently has a relatively low prevalence of HIV, all the above risk factors collectively pose a threat of increased new infections if not addressed at hand. With yet no effective cure nor vaccine against HIV, preventive measures aimed at reducing new infections mainly through risk-reduction are paramount in the fight against the HIV epidemic. The observed high prevalence of HIV risk factors, therefore, reflects a gap in the HIV/AIDS prevention and control strategies implemented in Sierra Leone, implying a need to strengthen health promotion and sexual behaviour educational programs among reproductive-aged women in the country. However, the reported prevalence, specifically, of non-condom use in this study is less than that reported by the World Health Organisation [30], and that from Tanzania [31], Malawi [32], USA [33] and China [34].
Our study also explored several socio-demographics associated with the burden of HIV risk factors, where age, parity, place of residence, region, sex of household head, marital status, and working status were found to be significant.
Women of younger age were more likely to engage in/encounter HIV risk factors compared to older women in Sierra Leone. This is similar to other studies that have individually reported age to be associated with inconsistent/non-condom use [3, 32], having other STIs [20, 35], transactional sex [20] and multiple sex partners [36]. Younger people are generally curious and common victims of peer influence thus can easily end up engaging in various risk behaviours for not only HIV but also other STIs [20, 35]. Moreover, parity was also significantly associated with HIV risk factors among women, whereby those who had ever produced fewer children were more likely to face HIV risk factors compared to their counterparts of more parity. The possible reason could be that women with no or fewer children are usually younger with less responsibilities and children to look after, so they can easily engage in risky behaviours [20, 36].
The current study results revealed that place of residence is associated with HIV risk factors, where urban women had more chances of encountering HIV risk factors. Due to the appealing and active nature of urban settings, with more entertainment avenues such as bars and clubs, women residing in these places are more exposed to risky behaviours [20]. Moreover, commercialized sexual activities and drug use tend to be more concentrated in urban areas, possibly due to the increasing trends of the urban poor and slum dwellings [20, 37]. Consistently, region was also found to be associated with HIV risk factors, where women in the Northwestern part of the country were more likely to face HIV risk factors. This may be attributed to the differential social-cultural contexts and economic developments in various parts of the country. No wonder, the Northwestern part has a higher concentration of economic development and mining activities, with a generally urban or semi-urban lifestyle [5]. Furthermore, the low employment rate of women in this region lures majority of them to engage in petty trading which exposes them to HIV risk factors during hawking from one community to another [5]. However, our results showed that women in the Southern part were less likely to encounter HIV risk factors yet the region has several fishing communities. The finding deviates from previous studies that have labelled such fishing communities as HIV/AIDS hotspots due to various unique risky behaviours in such communities [3, 38]. Region and place of residence have been reported in other studies to be associated with multiple sex partners [36], inconsistent condom use [39], STIs [39], and transactional sex [37].
Participants from female-headed households were more likely to encounter HIV risk factors compared to those from male-headed households. Consistently, unmarried women also had extremely higher chances of facing HIV risk factors compared to married women. Unmarried women from female-headed households tend to have more freedom from marital obligations and autonomy to do whatever they please, unlike their married counterparts, implying they can easily engage in risky behaviours for survival or economic reasons [36]. Marital status of women has been, disaggregatively, shown in other studies to be associated with transactional sex [37], multiple sex partners [36], and having other STIs [35].
Working status also had an association with HIV risk factors, whereby working women had more chances of encountering HIV risk factors compared to non-working women. Depending on the type and nature of the employment, most informal jobs predispose women to risky behaviours, for instance, working in bars, guesthouses, and sex workers, among others [37, 40]. Furthermore, although regarded as a crucial aspect of women empowerment, employment has been shown to have other negative associates, for example, sexual violence [40]. Working status of women has been reported in previous studies to be associated with having other STIs [35], transactional sex [37], and condom use [41].
Strengths and limitations
This is the first nationwide analysis that explores the burden of HIV risk factors and the associated socio-demographics, therefore, it can be used as a yardstick and motivation for further studies on the same topic in Sierra Leone and other countries. Secondly, we used the most current nationally representative dataset, thus our findings are generalizable to all women in Sierra Leone. However, our study is not without limitations, for example, the cross-sectional design only enables associations to be established but not causal relationships. There is also a possibility of recall bias due to self-reported answers, and giving false answers due to social desirability. There was also a lack of data on other key HIV risk factors such as alcohol and drug use and the missing data in the transactional sex variable risks underestimating transactional sex prevalence. Moreover, although marital status had extremely large odds ratios, it had a wider confidence interval as well, which could be due to inconsistency in the collected DHS data or other reasons, to which we had no control.
Conclusions
The study revealed that more than a third of the reproductive aged women in Sierra Leone had encountered at least one HIV risk factor. Age, parity, place of residence, region, sex of household head, marital status, and working status were associated with the prevalence of HIV risk factors in the country. There is thus a need for strengthening HIV/AIDS education and sex behaviour-change communication targeting the young working unmarried women, and those residing in urban areas of the country. In addition, the existing laws and policies in the country should be strengthened to safeguard working women from the associated risks of not only HIV but also other STIs.
Availability of data and materials
The data set used is openly available upon permission from MEASURE DHS website (https://www.dhsprogram.com/data/available-datasets.cfm).
Availability of data and materials
The data set used in this study is openly available from MEASURE DHS website and the modified data set that was used for the final analysis can be availed upon request from the corresponding author.
Abbreviations
- EA:
-
Enumeration area
- AOR:
-
Adjusted odds ratio
- CI:
-
Confidence interval
- COR:
-
Crude odds ratio
- DHS:
-
Demographic Health Survey
- SLDHS:
-
Sierra Leone Demographic Health Survey
- OR:
-
Odds ratio
- SD:
-
Standard deviation
- STI:
-
Sexually transmitted infection
- AIDS:
-
Acquired immunodeficiency syndrome
- HIV:
-
Human Immunodeficiency virus
- SPSS:
-
Statistical Package for Social Science
References
UNAIDS. Global HIV & AIDS statistics-Fact sheet. 2021. https://www.unaids.org/en/resources/fact-sheet. Accessed 25th Aug 2021.
KFF. Global Health Policy-The Global HIV/AIDS Epidemic. 2021. https://www.kff.org/global-health-policy/fact-sheet/the-global-hivaids-epidemic/#footnote-513952-10 . Accessed 25th Aug 2021.
Yendewa GA, Poveda E, Yendewa SA, Sahr F, Quiñones-Mateu ME, Salata RA. HIV/AIDS in Sierra Leone: characterizing the hidden epidemic. AIDS Rev. 2018;20:104–13.
CIA. Country comparisons: HIV/AIDS- Adult prevalence rate. 2021. https://www.cia.gov/the-world-factbook/field/hiv-aids-adult-prevalence-rate/country-comparison. Accessed 25th Aug 2021.
Statistics Sierra Leone (Stats SL) and ICF. Sierra Leone Demographic and Health Survey 2019. Freetown: Stats SL and ICF. 2020. https://dhsprogram.com/pubs/pdf/FR365/FR365.pdf. Accessed 7th Oct 2021.
Brima N, Burns F, Fakoya I, Kargbo B, Conteh S, Copas A. Factors associated with HIV prevalence and HIV testing in Sierra Leone: findings from the 2008 demographic health survey. PLoS ONE. 2015;10(10):e0137055.
Calvert C, Ronsmans C. HIV and the risk of direct obstetric complications: a systematic review and meta-analysis. PLoS ONE. 2013;8(10):e74848.
UNAIDS. 2020 Global AIDS update: seizing the moment; July 2020. UNAIDS. UNAIDS 2016–2021 strategy; Aug. 2015. https://www.unaids.org/sites/default/files/media_asset/2020_global-aids-report_en.pdf. Accessed 25th Aug 2021.
Spittal PM, Malamba SS, Ogwang MD, Musisi S, Ekwaru JP, Sewankambo NK, Pearce ME, Jongbloed K, Patel SH, Katamba A, Blair AH. Cango Lyec (Healing the Elephant): Gender differences in HIV infection in post-conflict Northern Uganda. J Acquir Immune Defic Syndr (1999). 2018;78(3):257.
Watts CH, Foss AM, Hossain M, Zimmerman C, von Simson R, Klot J. Sexual violence and conflict in Africa: prevalence and potential impact on HIV incidence. Sex Transm Infect. 2010;86(Suppl 3):iii93–9.
Audrey Djibo D, Sahr F, Allen McCutchan J, Jain S, Araneta RG, Brodine KS, Shaffer AR. Prevalence and risk factors for human immunodeficiency virus (HIV) and syphilis infections among military personnel in Sierra Leone. Curr HIV Res. 2017;15(2):128–36.
Kaiser R, Spiegel P. HIV sero prevalence and behavioral risk factor survey in Sierra Leone. Atlanta: Centers for Disease Control and Prevention; 2002.
Conjoh AM, Zhou Z, Xiong J. Socio-cultural factors affecting the spread of HIV/AIDS among adolescents in Sierra Leone. Soc Sci. 2011;6(4):269–76.
National HIV/AIDS Secretariat 2015. HIV sero-prevalence study for key populations. 2015. http://www.nas.gov.sl/images/stories/publications/Seroprevalence%20Study%20of%20Key%20Populations.pdf. Accessed 25th Aug 2021.
Ansumana R, Dariano DF, Jacobsen KH, et al. Prevalence of markers of HIV infection among febrile adults and children in Bo, Sierra Leone, 2012–2013. BMC Res Notes. 2017;10:565.
Kassa G, Dougherty G, Madevu-Matson C, Egesimba G, Sartie K, Akinjeji A, Tamba F, Gleason B, Toure M, Rabkin M. Improving inpatient provider-initiated HIV testing and counseling in Sierra Leone. PLoS ONE. 2020;15(7):e0236358.
Lakoh S, Firima E, Jiba DF, Sesay M, Conteh MM, Deen GF. Low partner testing in high HIV prevalence setting in Freetown, Sierra Leone: a retrospective study. BMC Res Notes. 2019;12(1):1–6.
Kelly JD, Reid MJ, Lahiff M, Tsai AC, Weiser SD. Community-level HIV stigma as a driver for HIV transmission risk behaviors and sexually transmitted diseases in Sierra Leone: a population-based study. J Acquir Immune Defic Syndr (1999). 2017;75(4):399.
Sakboonyarat B, Mungthin M, Nelson KE, Rangsin R. Rising prevalence of HIV infection and associated risk factors among young Thai Men in 2018. Sci Rep. 2021;11(1):1.
Zhao Y, Luo T, Tucker JD, Wong WC. Risk factors of HIV and other sexually transmitted infections in China: a systematic review of reviews. PLoS ONE. 2015;10(10):e0140426.
Simbayi LC, Kalichman SC, Jooste S, Mathiti V, Cain D, Cherry C. HIV/AIDS risks among South African men who report sexually assaulting women. Am J Health Behav. 2006;30(2):158–66.
Hoffman S, O’Sullivan LF, Harrison A, Dolezal C, Monroe-Wise A. HIV risk behaviors and the context of sexual coercion in young adults’ sexual interactions: results from a diary study in rural South Africa. Sex Transm Dis. 2006;33(1):52–8.
Demographic and Health Surveys. The DHS program. https://www.dhsprogram.com/.
Fish TD, Janocha B, Dontamsetti T, Mayala BK. Predicting geospatial covariates: proxies for mapping urban-related indicators. DHS spatial analysis reports no. 19. Rockville: ICF; 2020.
Bursac Z, Gauss CH, Williams DK, Hosmer DW. Purposeful selection of variables in logistic regression. Source Code Biol Med. 2008;3:17–17.
Agbadi P, Eunice TT. Complex samples logistic regression analysis of predictors of the current use of modern contraceptive among married or in-union women in Sierra Leone: insight from the 2013 demographic and health survey. PLoS ONE. 2020;15(4):e0231630.
Zou D, Lloyd JEV, Baumbusch JL. Using SPSS to analyze complex survey data: a primer. J Mod Appl Stat Methods. 2019;18(1):eP3253. https://doi.org/10.22237/jmasm/1556670300.
Croft Trevor N, Aileen MJM, Courtney KA, et al. Guide to DHS statistics. Rockville: ICF; 2018.
Country progress report—Sierra Leone Global AIDS Monitoring 2020. UNAIDS 2020. https://www.unaids.org/sites/default/files/country/documents/SLE_2020_countryreport.pdf. Accessed 21st Dec 2021.
World Health Organisation. Prevalence of condom use by adults during higher-risk sex (15–49). 2015. https://www.who.int/data/gho/data/indicators/indicator-details/GHO/prevalence-of-condom-use-by-adults-during-higher-risk-sex-(15-49)-(-).
Exavery A, Kanté AM, Jackson E, Noronha J, Sikustahili G, Tani K, Mushi HP, Baynes C, Ramsey K, Hingora A, Phillips JF. Role of condom negotiation on condom use among women of reproductive age in three districts in Tanzania. BMC Public Health. 2012;12(1):1–1.
Haddad LB, Tang JH, Krashin J, Ng’ambi W, Tweya H, Samala B, Chiwoko J, Chaweza T, Hosseinipour MC, Lathrop E, Jamieson DJ. Factors associated with condom use among men and women living with HIV in Lilongwe, Malawi: a cross-sectional study. BMJ Sex Reprod Health. 2018;44(1):1–2.
Copen CE. Condom use during sexual intercourse among women and men aged 15–44 in the United States: 2011–2015 National Survey of Family Growth. Natl Health Stat Rep. 2017;105:1–8.
Tang L, Chen R, Huang D, Wu H, Yan H, Li S, Braun KL. Prevalence of condom use and associated factors among Chinese female undergraduate students in Wuhan, China. AIDS Care. 2013;25(4):515–23.
Ginindza TG, Stefan CD, Tsoka-Gwegweni JM, Dlamini X, Jolly PE, Weiderpass E, Broutet N, Sartorius B. Prevalence and risk factors associated with sexually transmitted infections (STIs) among women of reproductive age in Swaziland. Infect Agents Cancer. 2017;12(1):1–2.
Simelane MS, Vermaak K, Zwane E, Masango S. Individual and community-level factors associated with lifetime number of sexual partners among women aged 15–49 in Eswatini. PLoS ONE. 2021;16(1):e0246100.
Dunkle KL, Jewkes RK, Brown HC, Gray GE, McIntryre JA, Harlow SD. Transactional sex among women in Soweto, South Africa: prevalence, risk factors and association with HIV infection. Soc Sci Med. 2004;59(8):1581–92.
Musumari PM, Techasrivichien T, Srithanaviboonchai K, Wanyenze RK, Matovu JK, Poudyal H, Suguimoto SP, Zamani S, Tangmunkongvorakul A, Ono-Kihara M, Kihara M. HIV epidemic in fishing communities in Uganda: a scoping review. PLoS ONE. 2021;16(4):e0249465.
Ajayi AI, Ismail KO, Akpan W. Factors associated with consistent condom use: a cross-sectional survey of two Nigerian universities. BMC Public Health. 2019;19(1):1–1.
Kawuki J, Sserwanja Q, Mukunya D, Sepenu AS, Musaba MW. Prevalence and factors associated with sexual violence among women aged 15–49 years in rural Uganda: evidence from the Uganda Demographic and Health Survey 2016. Public Health. 2021;196:35–42.
Hooshyar SH, Karamouzian M, Mirzazadeh A, Haghdoost AA, Sharifi H, Shokoohi M. Condom use and its associated factors among Iranian youth: results from a population-based study. Int J Health Policy Manag. 2018;7(11):1007.
Acknowledgements
We thank the DHS program for making the data available for this study.
Funding
No funding was obtained for this study.
Author information
Authors and Affiliations
Contributions
QS conceived the idea, drafted the manuscript, performed analysis, interpreted the results and drafted the subsequent versions of the manuscript. JK drafted the manuscript, interpreted the results and drafted the subsequent versions of the manuscript. KK reviewed the first draft and drafted the subsequent versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
High international ethical standards are ensured during MEASURE DHS surveys and the study protocol is performed in accordance with the relevant guidelines. The SLDHS 2019 survey protocol was reviewed and approved by the Sierra Leone Ethics and Scientific Review Committee and the ICF Institutional Review Board. Written informed consent was obtained from human participants and written informed consent was also obtained from legally authorized representatives of minor participants. This data set was obtained from the MEASURE DHS website (https://www.dhsprogram.com/data/available-datasets.cfm) after getting their permission, and no formal ethical clearance was obtained since we conducted a secondary analysis of publicly available data.
Consent for publication
Not applicable.
Competing interests
All authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Frequency of risk factors for HIV among reproductive aged women in Sierra Leone.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kawuki, J., Kamara, K. & Sserwanja, Q. Prevalence of risk factors for human immunodeficiency virus among women of reproductive age in Sierra Leone: a 2019 nationwide survey. BMC Infect Dis 22, 60 (2022). https://doi.org/10.1186/s12879-022-07037-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12879-022-07037-7