Abstract
Objective
This study aimed to assess the budget impact of introducing fixed-duration mosunetuzumab as a treatment option for adult patients with relapsed or refractory follicular lymphoma after at least two prior systemic therapies and to estimate the total cumulative costs per patient in the USA.
Methods
A 3-year budget impact model was developed for a hypothetical 1-million-member cohort enrolled in a mixed commercial/Medicare health plan. Comparators were: axicabtagene ciloleucel, tisagenlecleucel, tazemetostat, rituximab plus lenalidomide, copanlisib, and older therapies (rituximab or obinutuzumab ± chemotherapy). Costs per patient comprised treatment-associated costs including the drug, its administration, adverse events, and routine care. Dosing and safety data were ascertained from respective package inserts and clinical trial data. Drug costs (March 2023) were estimated based on the average wholesale acquisition cost reported in AnalySource®, and all other costs were based on published sources and inflated to 2022 US dollars. Market shares were obtained from Genentech internal projections and expert opinion. Budget impact outcomes were presented on a per-member per-month basis.
Results
Compared with a scenario without mosunetuzumab, its introduction over 3 years resulted in a budget increase of $69,812 (1% increase) and an average per-member per-month budget impact of $0.0019. Among the newer therapies, mosunetuzumab had the second-lowest cumulative per patient cost (mosunetuzumab = $202,039; axicabtagene ciloleucel = $505,845; tisagenlecleucel = $476,293; rituximab plus lenalidomide = $263,520; tazemetostat = $250,665; copanlisib = $127,293) and drug costs, and its introduction only increased total drug costs by 0.1%. By year 3, the cumulative difference in the per patient cost with mosunetuzumab was −$303,805 versus axicabtagene ciloleucel, −$274,254 versus tisagenlecleucel, −$61,481 versus rituximab plus lenalidomide, −$48,625 versus tazemetostat, and $74,747 versus copanlisib. Older therapies were less costly with 3-year cumulative costs that ranged from $36,512 to $147,885.
Conclusions
Over 3 years, the estimated cumulative per patient cost of mosunetuzumab is lower than most available newer therapies, resulting in a small increase in the budget after its formulary adoption for the treatment of relapsed or refractory follicular lymphoma.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
A budget impact model assessed the incremental budget of adding mosunetuzumab for relapsed or refractory follicular lymphoma treatment in a US health plan. |
Mosunetuzumab offers cost savings over most other newer therapies, which ranged from a 19% to a 60% reduction in total cumulative per patient costs over 3 years. |
The addition of fixed-duration mosunetuzumab treatment resulted in a minimal budget impact on a US health plan over a 3-year time horizon. |
1 Introduction
Non-Hodgkin lymphomas (NHLs) are a group of heterogeneous neoplasms of the lymphoid system that vary from the most indolent to the most aggressive malignancies [1,2,3]. In the USA, 788,781 people were living with NHL in 2020, and it was estimated that 80,550 new cases would occur in 2023 [3]. Follicular lymphoma (FL) is the second most common lymphoma and accounts for approximately 20–35% of all NHLs [3, 4]. Despite being classified as indolent, FL is not curable with current therapies. Most patients experience relapses and face a risk of transformation to aggressive lymphoma, which is associated with poor outcomes [3, 4].
New treatment modalities have emerged in recent years for patients with relapsed or refractory (R/R) FL who had received two or more previous lines of systemic therapy including: phosphoinositide 3-kinase inhibitors (PI3K), enhancer of zeste homolog 2 (EZH2) inhibitors (tazemetostat), immunomodulatory agents (lenalidomide), and chimeric antigen receptor (CAR) T-cell therapies [4]. However, among the PI3K, the US Food and Drug Administration (FDA) withdrew its approval of umbralisib [5] while the sponsors of idelalisib [6] and duvelisib [7] voluntarily withdrew the accelerated approval of these agents for R/R FL in the USA in 2022 and 2021, respectively, leaving only copanlisib available and approved for the indication. Additionally, therapies such as copanlisib [8] and tazemetostat [9] are not fixed duration, but must be taken continuously until disease progression or unacceptable toxicity. Conversely, two approved CAR T-cell therapies, namely axicabtagene ciloleucel (YESCARTA®) and tisagenlecleucel (KYMRIAH®), are available as a single infusion and have demonstrated high complete response rates, with the median duration of response not reached at the data cut-off in clinical trials. However, they are only accessible through restricted programs because of the risk of high-grade cytokine release syndrome (CRS) and neurological events [10, 11]. Both have caused fatal or life-threatening reactions following administration and require strict monitoring [10, 11].
Despite the availability of multiple therapies, there is no standard treatment or sequence of treatments for patients with R/R FL. Treatment options also become increasingly limited from the third line onwards, especially for patients who are not able to receive select immunochemotherapies due to comorbidities [12]. Patients with FL also acquire increasing resistance to chemotherapy with each successive relapse and re-treatment event [12], leading to a shorter duration of response and progression-free survival with each line of therapy [13]. Lastly, patients who relapse or experience early treatment failure with immunochemotherapies typically experience inferior outcomes to subsequent immunochemotherapies [14], further underlining a need for newer therapies with different mechanisms of action.
In December 2022, the FDA granted mosunetuzumab (LUNSUMIO™) accelerated approval for the treatment of adult patients with R/R FL after two or more lines of systemic therapy [15, 16]. Mosunetuzumab is a CD20xCD3 T-cell engaging bispecific antibody that redirects T cells to eliminate B cells, including those that cause malignant disease. The approval of fixed-duration mosunetuzumab was based on the results of the phase II GO29781 study (NCT02500407) that evaluated the efficacy and safety of mosunetuzumab in patients with R/R FL [15, 16]. Over a median follow-up of 18.3 months, a complete response was recorded in 60% of patients (95% confidence interval [CI]: 49–70%) and an objective response was observed in 80% (95% CI: 70–88%) according to an independent review committee assessment [17]. The median duration of response was 22.8 months [17]. In addition, mosunetuzumab had a manageable safety profile. The step-up dosing in the first cycle effectively mitigated the risk of CRS allowing for outpatient administration [17]. Despite the promising clinical data, evidence on the economic benefit of mosunetuzumab to payers is currently lacking. To address the budgetary concerns from payers over the inclusion of mosunetuzumab to their formularies, we developed a budget impact model (BIM) to analyze the per patient cost and budget impact of introducing mosunetuzumab as treatment for R/R FL from a third-party payer perspective.
2 Methods
2.1 Model Overview
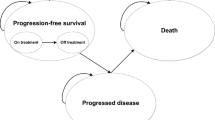
Two scenarios were modeled to explore the budgetary impact of introducing mosunetuzumab. The current scenario reflects the current standard of care (without mosunetuzumab) whereas the projected scenario is defined as a world where mosunetuzumab is an available option in the treatment landscape (Fig. 1 of the Electronic Supplementary Material [ESM]). A comparison of the current and projected scenarios provided an estimate of the budget impact of mosunetuzumab being covered and reimbursed over a given time horizon. The analyses were conducted over a 3-year time horizon, where each year had a duration of 364 days (i.e., 52 weeks × 7 days per week). The model cycle length varied for each regimen to align with their dosing schedule. Costs included drug and wastage costs, administration costs, adverse event (AE) costs, CRS costs, and routine costs of care. All costs are presented in 2022 US Dollars, except drug acquisition costs, which were current as of March 2023. Where applicable, the medical care component of the consumer price index was used to inflate costs to 2022 US Dollars [18].
Comparison of cumulative costs per patient per regimen over 3 years. AE adverse events, Admin administration, Axi-cel axicabtagene ciloleucel, Copan copanlisib, CRS cytokine release syndrome, G Obinutuzumab, Len lenalidomide, Mono monotherapy, Mosun mosunetuzumab, R rituximab, Taz tazemetostat, Tisa-cel tisagenlecleucel
The budget impact for each of the first 3 years and the overall 3-year budget impact were assessed. Budget outcomes were presented in absolute and net terms and included per-member per-month (PMPM) calculations. The BIM was developed in Microsoft Excel 2016 (Microsoft Corporation, Redmond, WA, USA) and complied with recommendations of the International Society for Pharmacoeconomics and Outcomes Research Principles of Good Practice for Budget Impact Analysis [19]. The model did not include discounting (i.e., all results are presented undiscounted), which is standard practice and consistent with International Society for Pharmacoeconomics and Outcomes Research guidelines [19].
2.2 Target Population
The target population in the model included adult patients with R/R FL. The model considered a hypothetical population of one million people enrolled in a nationally representative mix of commercial and Medicare health plans. Within this population, the number of adult enrollees (aged ≥18 years) was estimated from the National Population Projections Datasets of the US Census Bureau [20]. The same source was used to stratify the adult population between two age groups, namely those who were aged 18–64 years versus those aged 65 years or older [20]. These figures were then multiplied by the respective prevalence of NHL obtained from the Surveillance, Epidemiology, and End Results Program [21]. Among the identified adult patients with NHL, the proportion of those with FL were based on estimates derived from the literature [3]. Finally, this figure was then multiplied by the proportion of patients with FL who were R/R after two or more previous lines of systemic therapy to estimate the total existing number of people with R/R FL for year 1. In the base case, Link et al. was used, but an alternate source was tested in a scenario analysis [22, 23]. For years 2 and 3, the number of patients receiving treatment in the previous year was summed with the expected new cases per year. The expected new cases per year were calculated as detailed above but after subtracting the number of patients already identified as R/R FL from the one million-member health plan. The inputs used to estimate the size of the target population are summarized in Table 1. It was assumed that 45.9% of patients were covered by commercial plans, based on internal commercial data on file [24]. The remainder of patients were assumed to be covered by Medicare.
2.3 Comparators and Market Share
Comparators were chosen based on current market shares and the anticipated treatment landscape in the R/R FL indication and included the following: rituximab monotherapy and in combination with bendamustine or lenalidomide, obinutuzumab monotherapy and in combination with bendamustine, copanlisib, and tazemetostat, and finally two CAR T-cell therapies, namely axicabtagene ciloleucel and tisagenlecleucel. Patients were distributed to different treatment regimens according to specified market shares based on projections made by Genentech as well the expertise provided by Dr. Matasar, a co-author on this study and expert in the field of oncology (Table 1 of the ESM). Comparators were grouped into two subgroups: older therapies, consisting of the anti-CD20 monoclonal antibodies with or without chemotherapy; and newer therapies (copanlisib, axicabtagene ciloleucel, tisagenlecleucel, tazemetostat, and rituximab with lenalidomide).
2.4 Cost Components
2.4.1 Total Treatment Costs
Total treatment costs (Table 2) included drug costs, wastage costs, and administration costs; these were applied for as long as treatments were given (i.e., until discontinuation). Dosing of each regimen was based on US Prescribing Information (PI) or trial publication (Table 2 of the ESM). Treatment duration was estimated and incorporated into the model based on the mean treatment duration as reported in clinical trials or estimated from the median using the methodology by Hozo et al. [25] except for rituximab plus lenalidomide due to data limitations (Table 2). Drug costs were based on wholesale acquisition cost (WAC) prices sourced from AnalySource® [26] and, where applicable, considered the availability of biosimilars (Table 3 of the ESM). Dosing calculations were based on an average body weight of 81.4 kg and an average body surface area of 1.96 m2 based on patients in the GO29781 study [17]. Wastage costs were estimated by comparing the daily discrepancy between vial size and the actual dosage required. Oral medications incur no wastage.
Administration costs were applied for intravenous treatments and CAR T-cell therapies. Resource use was calculated based on the time needed to administer the drug, taking into account information on dosing and the infusion rate found in US PI [8, 16, 27,28,29]. We applied a conservative approach where the standard infusion rate was used, ignoring infusion-related complications. The time required for administering each drug compound was then matched to its relevant Current Procedural Terminology code. Finally, unit costs for each Current Procedural Terminology code were based on the 2022 Centers for Medicare and Medicaid Services (CMS) physician fee schedule [30].
The administration of CAR T-cell therapies requires additional resources. These are detailed in Table 4 of the ESM. CAR T-cell therapies require a leukapheresis procedure. Aligned with Liu et al. [31], the costs of leukapheresis and administration were obtained from the CMS Physician Fee Schedule [30]. Patients also received one-time conditioning chemotherapy prior to infusion of the CAR T cells for which drug and administration costs were captured. The choice of conditioning chemotherapy and associated dosing was aligned with US PI and trial publications [10, 11, 32] while drug acquisition costs were based on WAC prices sourced from AnalySource® [26]. Finally, a hospital stay was assumed. For axicabtagene ciloleucel, per its US PI [10], all patients were assumed to be hospitalized, whereas for tisagenlecleucel, the proportion of patients receiving tisagenlecleucel in the inpatient setting versus outpatient setting was based on the ELARA study [32]. The duration of the hospital stay was conservatively assumed equal to 9 days (from day −1 to day 7 inclusively) per expert opinion, without admission to the intensive care unit (ICU). The cost per day was based on the literature [33].
2.4.2 Adverse Events
Adverse events (AEs) of Grade ≥3 severity and occurring in at least 5% of patients treated with any regimen were included, except those not expected to have significant cost impacts. The AE rates, outlined in Table 5 of the ESM, were extracted from relevant publications or US PIs and were applied once in the model at the beginning of treatment. Adverse event rates not reported for a given regimen were assumed to be zero. Costs for neurologic events were based on Abramson et al. [34] whereas all other AE costs were derived from the Healthcare Cost and Utilization Project (Hospital Inpatient National Sample 2015, available at https://hcupnet.ahrq.gov/, accessed 8 May, 2022 and 12 December, 2022) and based on the appropriate International Classification of Diseases, Ninth Revision codes of each AE (Table 5 of the ESM). Where available, distinct Medicare and commercial costs were obtained and the model computed a weighted average of the Medicare and commercial costs based on the proportion of Medicare patients assumed (54.1% in the base case).
2.4.3 Cytokine Release Syndrome
Aside from the AE rates, patients treated with mosunetuzumab and CAR T-cell therapies face the additional risk of CRS. This was modeled separately in the BIM and all grade AEs were included. The management of CRS followed the suggested management of immunotherapy-related toxicities in the US PI of mosunetuzumab, axicabtagene ciloleucel, and tisagenlecleucel [10, 11, 16], as well as the study protocol of mosunetuzumab as reported in Budde et al. [17]. It included: tocilizumab use, ICU admission, and hospitalization (non-ICU). Rates of CRS and resources for the management of CRS are outlined in Table 3. The cost of tocilizumab accounted for drug, wastage, and administration costs. The dosing schedule of tocilizumab was assumed the same across all regimens and was based on the mosunetuzumab GO29781 study protocol as reported in Budde et al. [17]. The drug acquisition cost was based on WAC prices extracted from AnalySource® [26]. Administration costs were obtained from the 2022 CMS Physician Fee Schedule [30] based on CPT code 96413, aligned with its infusion schedule [35]. For the ICU and hospitalization (non-ICU) costs, the model assumed a daily cost of $6615 (ICU) and $3323 (non-ICU), which was derived from Liu et al. [31] and HCUP [33], respectively. The CRS costs stratified by regimen are detailed in Table 6 of the ESM. These are weighted by the proportion of patients experiencing CRS and are applied once at treatment initiation.
2.4.4 Routine Care
Routine care costs comprised management costs associated with FL. These were sourced from expert opinion, which stated that typical clinical practice would include one visit every 3 months with laboratory work (complete blood count, comprehensive metabolic panel, and lactate dehydrogenase) as well as a computed tomography chest abdomen pelvis scan every 6 months. For CAR T-cell therapies, a positron emission tomography scan at day 90 would be added and visits for laboratory work (complete blood count, comprehensive metabolic panel, and lactate dehydrogenase) would occur monthly for the first 6 months. The unit costs for office visits, laboratory tests, and imaging were obtained from the CMS Physician Fee Schedule and laboratory schedules (Table 7 of the ESM) [30, 36]. The resulting total FL management costs in year 1 were $1713 for CAR T-cell therapies and $1132 for all other regimens. In years 2–3, the FL management costs were the same across all regimens and amounted to $1132 annually. Routine care costs were applied continuously throughout the model, as mortality was excluded in the base case.
2.5 Sensitivity Analyses
Sensitivity analyses were conducted around the budget impact, including a deterministic sensitivity analysis and scenario analyses. The deterministic sensitivity analysis examined the impact of uncertainty of model parameters including parameters related to the size of the target population, patient characteristics, market penetration of mosunetuzumab, and costs (intervention and comparator drug costs, administration, AEs, CRS, and routine care). Each parameter was varied ±20% around its base-case value. Scenario analyses were conducted to test structural assumptions. First, the time horizon was limited to 1 year. Second, the share of patients with FL who are R/R was aligned with another published BIM in R/R FL [23]. Third, the treatment duration of each regimen was set to the maximum duration as opposed to the mean duration. For regimens with maintenance therapy, separate scenario analyses were included to vary the parameters related to both the use of maintenance (0–100%) and duration (full course of maintenance). Furthermore, we tested an alternative source for the routine care costs that considered broader outpatient costs. Additionally, we tested the impact of the payer mix on the budget impact by analyzing two scenarios: all patients were assumed to be 18–64 years of age and commercially insured or aged 65 years of age or older and covered by Medicare. To assess the impact of the base-case assumption of no vial sharing, a scenario analysis assuming zero wastage was generated. Additionally, we re-generated the results using the average sales price (ASP) (where feasible), in lieu of WAC, for the subset of patients with Medicare coverage. Except for mosunetuzumab and oral drugs where WAC was used, the ASP was extracted from the April 2023 Medicare Part B Drug and Biological ASP Quarterly Payment files and the 2023 CMS Hospital Outpatient Prospective Payment System (Addendum B) [37, 38]. Lastly, a scenario analysis considering a generic uptake of lenalidomide similar to rituximab (68%) was analyzed; rituximab was used as a proxy because of a lack of data.
3 Results
3.1 Base-Case Results
In the hypothetical health plan of 1 million lives, the annual number of patients eligible for mosunetuzumab was estimated to be 10. Table 4 presents the overall current and projected budget as well as the budget impact (total and PMPM) associated with the addition of mosunetuzumab for the treatment of R/R FL. The breakdown of the current and projected budget by cost components for each year of the time horizon is shown in Tables 8 and 9 of the ESM. The introduction of mosunetuzumab to the R/R FL treatment landscape was estimated to result in an increase in budget of $69,812 (1% increase), which translated to an average incremental PMPM of $0.0019 over the 3-year time horizon (Table 4). This 1% budget increase corresponds to a net budget of $23,380,551 for the overall US population in 2023 (N = 334,906,000) [39].
The 3-year cumulative per patient cost for each regimen is depicted in Fig. 1 and Table 10 of the ESM. Over 3 years, the estimated cumulative per patient cost of mosunetuzumab is lower than most available newer therapies. More specifically, mosunetuzumab had the second lowest total cumulative per patient and drug costs among other newer therapies included in the model. When compared with mosunetuzumab, the cumulative difference over 3 years in the per patient cost amounted to a cost savings of $303,805 versus axicabtagene ciloleucel, $274,254 versus tisagenlecleucel, $61,481 versus rituximab plus lenalidomide, $48,625 versus tazemetostat, and a cost increase of $74,747 versus copanlisib. Older therapies, such as anti-CD20 monoclonal antibodies with or without chemotherapy, were cheaper with 3-year cumulative costs that ranged from $36,512 to $147,885.
Figure 1 and Table 10 of the ESM also show the cumulative per patient costs broken down into their cost components: drug costs accounted for the largest share of cumulative per patient cost for all regimens (~86% on average). Mosunetuzumab and the CAR T-cell therapies had an extra cost attributable to CRS. However, mosunetuzumab had the lowest CRS costs ($7174) relative to tisagenlecleucel ($7987) and axicabtagene ciloleucel ($29,310). Mosunetuzumab also incurred zero wastage contrary to chemotherapy-based regimens where wastage costs contributed up to 8% of the total per patient costs. Administration costs were highest for the CAR T-cell therapies (tisagenlecleucel: $27,121; axicabtagene ciloleucel: $32,045) whereas mosunetuzumab administration costs ($1878) were among the lowest. Finally, routine care costs were comparable among all regimens.
3.2 Sensitivity and Scenario Analyses
Results from one-way sensitivity and scenario analyses results were consistent with base-case findings. More specifically, Fig. 2 presents the PMPM budget impact over the 3-year time horizon for each sensitivity analysis conducted. Only the ten most impactful parameters on the PMPM budget impact are depicted in the tornado plot. Applying a discount or mark-up on the mosunetuzumab WAC or all comparator WACs combined, varying the patient’s body surface area (which impacts total drug costs), and varying the share of plan members who are between the ages of 18 and 64 years (which impacts the total number of treated patients) were the top drivers on the budget impact. The market uptake of mosunetuzumab had only a small impact on the PMPM budget impact. Across all sensitivity analyses, the inclusion of mosunetuzumab had a minimal impact on the PMPM cost, with a range from −$0.0072 to $0.0111 compared with $0.0019 in the base case. See Fig. 2 of the ESM for the tornado diagram of one-way sensitivity analyses on the total budget impact over 3 years.
The results of the ten scenario analyses conducted are shown in Table 5, and are aligned with the base-case findings. The scenario that increased the PMPM budget impact the most was the use of the maximum duration for all regimens in the drug cost calculations instead of the mean duration (Scenario 3), which yielded a PMPM budget impact of $0.0115. The payer channel (Scenario 7) had the second biggest impact on the PMPM budget associated with the inclusion of mosunetuzumab over 3 years ($0.0009–$0.0059). This is mostly due to the size of the target population: from five patients (100% commercial) to 31 patients (100% Medicare) in year 1 versus ten in the base case. Another important scenario limiting the time horizon to 1 year (Scenario 1) only resulted in a PMPM budget impact of $0.0050. Relying on a different source for the share of patients with FL who are R/R (Scenario 2), assuming all patients taking obinutuzumab plus bendamustine or rituximab plus bendamustine used the full course of maintenance therapy versus none (Scenarios 4 and 5), excluding wastage (Scenario 8), considering a mix of brand/generic formulations for the drug acquisition cost of lenalidomide (Scenario 9), and substituting WAC for ASP (where feasible) for the subset of patients with Medicare coverage (Scenario 10) all modestly impacted the model’s results. However, in all these scenarios, the addition of mosunetuzumab continued to be associated with an increase in the budget. The only exception is Scenario 6 where considering broader outpatient costs for the routine cost of care led to a modest cost savings (PMPM budget impact of −$0.0002).
4 Discussion
The base-case results suggest that over a 3-years time horizon the introduction of mosunetuzumab will lead to an increase in overall costs for the treatment of R/R FL (incremental budget impact of $60,596, −$3583, and $12,799 for years 1, 2, and 3). The average PMPM net budget over this period is $0.0019 for a hypothetical US health plan of one million members.
The two largest drivers contributing to the net budget increase over the 3-year period stem from drug costs and CRS costs. Despite drug costs accounting for over 90% of the total costs in the projected scenario, the introduction of mosunetuzumab only increases the total drug costs (including wastage) by 0.1%, compared with the current scenario. This is the result of mosunetuzumab having the second lowest cumulative drug cost among the newer therapies (mosunetuzumab = $180,000; axicabtagene ciloleucel = $424,000; tisagenlecleucel = $427,347; rituximab plus lenalidomide = $244,347; tazemetostat = $246,820; copanlisib = $107,556). The costs associated with CRS were the second largest driver of the increase in budget with the introduction of mosunetuzumab. This is expected as only patients who take mosunetuzumab and CAR T-cell therapies are at risk of experiencing CRS events.
The cost savings of mosunetuzumab relative to most other newer therapies is driven by a variety of reasons. Relative to the CAR T-cell therapies, mosunetuzumab had lower drug acquisition costs, administration costs, and CRS costs. Relative to tazemetostat, which is a treat-to-progression regimen, mosunetuzumab benefits from a fixed treatment duration that resulted in lower drug costs. Finally, relative to rituximab plus lenalidomide, while both treatments are administered over a fixed duration, mosunetuzumab is administered for a shorter duration than lenalidomide, which again reduced the total drug costs.
In the base case, the introduction of mosunetuzumab led to a modest increase in the net budget in year 1 ($60,596) and year 3 of the model ($12,799) but budget savings in year 2 (−$3,583). These results may appear counterintuitive considering that new patients enter the model every year (~10/year). However, these year-to-year differences can be explained not only by the per patient costs of each regimen at each year of treatment (most notably the drug costs) but also on the market share breakdown between the current (without mosunetuzumab) versus projected (with mosunetuzumab) scenarios. If the uptake of mosunetuzumab was assumed to proportionally displace all therapies including the CAR T cells, the introduction of mosunetuzumab would have resulted in budget savings at each year of the model. Instead, if the uptake of mosunetuzumab was assumed to proportionally displace all therapies excluding the CAR T cells, the introduction of mosunetuzumab would have resulted in a budget increase at each year of the model.
Deterministic sensitivity analyses of select inputs highlighted that parameters directly influencing the drug costs are the most impactful parameters on the budget impact. It is worth noting that assuming a slower or faster penetration of mosunetuzumab on the market for years 1, 2, and 3 had a minimal impact on the net budget. However, this sensitivity analysis assumed that mosunetuzumab would not displace CAR T-cell therapies. Hence, the results could vary if this assumption does not hold.
Currently, the only published budget impact model for therapies in the R/R FL space is the study conducted by Appukkuttan et al. The authors examined the 1-year budget impact for treatments for R/R FL with and without the introduction of copanlisib [23]. Despite a similar approach to derive the eligible population, their model estimated that 18 patients (roughly 4.5% of prevalent FL population) had relapsed FL and had received at least two previous systemic therapies. In contrast, our model estimated only 2.2% of the prevalent FL population to have R/R FL and at least two prior therapies. Our base-case assumption of 2.2% is from Link et al. [22], a real-world study of treatment patterns among patients with FL between 2004 and 2007. Appukkuttan et al. relied on estimations from SEER, the Datamonitor Healthcare report, and unpublished Kantar Health data [23, 40, 41]. In the scenario analysis, increasing the prevalent R/R population to 4.5% resulted in an increase in our model’s PMPM value from $0.0019 in the base case to $0.0039. There were other differences between the models as well. Appukkuttan et al. included off-label or since withdrawn therapies, specifically ibrutinib and idelalisib, whereas our model did not. Further, their study did not include the costs of AEs or consider the impact of biosimilars. Despite these differences, the mosunetuzumab model’s findings align with those of Appukkuttan et al. in that both models demonstrate a minimal budget impact for a third-party payer from the introduction of new therapies in this area.
While no other published budget impact models were available for comparison, there are many published studies on the economics of CAR T-cell therapies in FL or large B-cell lymphoma that can shed light on treatment and associated costs with these regimens. Potnis et al. published a cost-effectiveness analysis of CAR T-cell therapy, namely axicabtagene ciloleucel, for patients with R/R FL, and modeled upfront costs of CAR T-cell therapies (including drug acquisition costs, leukapheresis, dose preparation, bridging/conditioning therapies, inpatient hospitalization, and AE management) as costing $443,118, with a range of $373,000–$711,884 in a sensitivity analysis [42]. By comparison, our analysis estimated the cost per patient in the first year to be $503,580 for axicabtagene ciloleucel, which falls within the range reported by Potnis et al. [42] A few differences are worth noting. First, the present analysis is based on more recent costing estimates versus Potnis et al. and is based on a different payer perspective (mix of commercial/Medicare vs Medicare only). For example, drug prices in Potnis et al. have been extracted from the 2021 CMS Hospital Outpatient Prospective Payment System and the July 2021 CMS ASP files. The base case presented here relies on WAC from March 2023 although ASP from the 2023 CMS Hospital Outpatient Prospective Payment System and the April 2023 CMS ASP files have been used (where appropriate) in the scenario analysis for the proportion of patients covered by Medicare. In terms of administration costs, Potnis et al. assumed that patients were admitted to the hospital on the day of the CAR T-cell infusion and remained in the hospital for 7 additional days after the infusion, whereas we assumed that patients required a hospital stay of 9 days (from day −1 to day 7) based on expert opinion. Note that our assumption aligns with the protocol of Memorial Sloan Kettering Cancer Center, which states patients undergoing an inpatient infusion will be required to be in the hospital 24 h prior to, during, and post-infusion (extending for a duration of 1–2 weeks or even longer) [43]. In terms of AE costs, both models assumed that grade 3+ AEs resulted in inpatient hospitalization. However, costs in Potnis et al. were derived from 2021 Medicare diagnosis-related group payments, whereas our analysis relied on HCUP, a source that has been used extensively in the literature [44,45,46,47]. Despite these differences, our model produced a conservative estimate that is well within the range reported by Potnis et al. as previously stated. Liu et al. reported the total treatment associated costs (not disease related) to be $452,629 and $471,628 for axicabtagene ciloleucel and tisagenlecleucel, respectively [31]. While these are reported as lifetime discounted costs, most treatment-related costs will be incurred around the time of administration. Davies et al. conducted a real-world study of costs related to CAR T-cell treatment and found that the total all-cause costs from the 30 days prior to treatment through the 90 days after treatment to be $511,139 [48]. More recently, a study by Oluwole et al. assessed the cost effectiveness of axicabtagene ciloleucel versus mosunetuzumab in R/R FL. Despite a direct comparison with our BIM being difficult considering that only lifetime discounted costs are detailed, their study accounted for similar cost items as the present analysis [49]. For example, drug acquisition costs were the same between both studies despite relying on different sources. Also, our model applied lower costs for leukapheresis, conditioning chemotherapy, and administration (total costs: $2142) compared with $4219 in the study by Oluwole et al. due to differences in the cost of leukapheresis. The cost per day for a hospitalization was also very similar ($3323 vs $3461). However, assumptions related to the duration of hospitalization differed between both studies. More specifically, Oluwole et al. assumed a 13-day hospital stay ($44,999) that encompassed the cost of treating all AEs, except for hypogammaglobulinemia. By contrast, our study assumed an initial 9-day hospital stay with additional costs for CRS and AEs for a combined cost of $75,725. Our model appears more closely aligned to real-world studies [50, 51]. Keating et al., using real-world data, estimated the mean total inpatient hospital days from 17–22 days for patients with DLBCL treated with CAR T-cell therapies [50]. The length of stay increased with severe CRS (19–27 days) or severe neurological events (22–29 days) [50]. Similarly, a study by Maziarz et al. estimated the mean inpatient length of stay during infusion at 18.3 days for axicabtagene ciloleucel [51]. In summary, our analysis estimated the cost per patient in the first year to be $503,580 for axicabtagene ciloleucel and $476,293 for tisagenlecleucel, which is aligned with published sources and a priori, appear conservative as updated WAC prices were used ($424,000 for axicabtagene ciloleucel and $427,048 for tisagenlecleucel, compared with $373,000 for each in Liu et al. and Potnis et al.).
This budget impact analysis presented here has several limitations that should be noted. Firstly, the model does not include progression-free survival and overall survival effects from the patient disease pathway directly; these were excluded for simplicity and transparency into cost drivers. Despite progression-free survival and overall survival not being explicitly modeled, the base-case analysis incorporated the mean treatment duration as reported in clinical trials, which should mitigate this limitation. Further, it should be noted that post-discontinuation therapy was not assessed in this model; in practice, patients would likely switch to another therapy upon relapse or disease progression. These costs were excluded for simplicity and because the median time for next treatment for novel therapies extended beyond the relatively short (1–3 years) model time horizon [52,53,54,55,56,57]. In addition, without any head-to-head trials or matched-adjusted indirect treatment comparisons assessing the relative efficacy of mosunetuzumab versus all comparators in the model, incorporating unadjusted efficacy would bias the analysis because of inherent differences in trial populations.
Another limitation concerned the compliance rate. In the model, a 100% compliance rate was assumed for all regimens, which may vary in real-world settings. As compliance would directly impact the drug costs, it is unclear how this could impact the overall budget. However, mosunetuzumab is administered intravenously, as are most of the existing therapies. Hence, it is unlikely that the compliance rate would differ between mosunetuzumab and the regimens being displaced by the entry of mosunetuzumab.
Finally, the model inputs considered in this framework were obtained from multiple data sources and assumptions in some cases. This led to uncertainties in model inputs in the present analysis. Estimates of the market share are based on projections and hence subject to uncertainty. For existing therapies, there are also likely to be discounts in place that could further augment the incremental cost associated with the entry of mosunetuzumab. For this reason, these should be included into the BIM if data are available. However, to assess the importance of these uncertainties, extensive sensitivity analyses were conducted. The results from these analyses generally support the robustness of the model results to reasonable variations in key model inputs.
5 Conclusions
The budget impact analysis estimated that fixed-duration mosunetuzumab treatment offers cost savings compared with most other newer drugs that range from a 19 to a 60% reduction in total cumulative per patient costs over 3 years. This led to an average PMPM budget impact of $0.0019 over this period for a one-million-member plan. The current treatment landscape for FL is complex and evolving. Treatment options for R/R FL are relatively limited with no current standard of care. Providing access to mosunetuzumab, a fixed-duration therapy with a newer mechanism of action for the treatment of adult patients with R/R FL, provides a new treatment option to patients, which at the same time should have a minimal budget impact on US health plans over a 3-year time horizon.
References
Shankland KR, Armitage JO, Hancock BW. Non-Hodgkin lymphoma. Lancet. 2012;380(9844):848–57. https://doi.org/10.1016/s0140-6736(12)60605-9.
Armitage JO, Gascoyne RD, Lunning MA, Cavalli F. Non-Hodgkin lymphoma. Lancet. 2017;390(10091):298–310. https://doi.org/10.1016/s0140-6736(16)32407-2.
National Cancer Institute. Adult non-Hodgkin lymphoma treatment (PDQ®), Health Professional Version. 2022. Available from: https://www.cancer.gov/types/lymphoma/hp/adult-nhl-treatment-pdq. [Accessed 6 Dec 2022].
Freedman A, Jacobsen E. Follicular lymphoma: 2020 update on diagnosis and management. Am J Hematol. 2020;95(3):316–27. https://doi.org/10.1002/ajh.25696.
US Food and Drug Administration. FDA withdrew its approval for the cancer medicine Ukoniq (umbralisib) due to safety concerns. 2022. Available from: https://www.fda.gov/drugs/fda-drug-safety-podcasts/fda-withdrew-its-approval-cancer-medicine-ukoniq-umbralisib-due-safety-concerns. [Accessed 1 Jun 2022].
Gilead Inc. Gilead Statement on Zydelig® US indication for follicular lymphoma and small lymphocytic leukemia. 2022. Available from: https://www.gilead.com/news-and-press/company-statements/gilead-statement-on-zydelig-us-indication-for-follicular-lymphoma-and-small-lymphocytic-leukemia. [Accessed 18 Aug 2023].
Secura Bio Inc. Secura Bio announces Copiktra® (duvelisib) strategic focus on T-cell lymphoma and voluntary U.S. withdrawal of the relapsed or refractory follicular lymphoma indication. 2021. Available from: https://www.prnewswire.com/news-releases/secura-bio-announces-copiktra-duvelisib-strategic-focus-on-t-cell-lymphoma-and-voluntary-us-withdrawal-of-the-relapsed-or-refractory-follicular-lymphoma-indication-301436834.html. [Accessed 18 Aug 2023].
Bayer HealthCare Pharmaceuticals Inc. ALIQOPA™ (copanlisib): highlights of prescribing information. 2022. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2022/209936s010lbl.pdf. [Accessed 18 Apr 2022].
Epizyme Inc. TAZVERIK (tazemetostat) tablets: highlights of prescribing information. 2020. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/213400s000lbl.pdf. [Accessed 18 Apr 2022].
Kite Pharma Inc. YESCARTA® (axicabtagene ciloleucel): highlights of prescribing information. 2022. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2020/213400s000lbl.pdf. [Accessed 18 Apr 2022].
Novartis Pharmaceuticals Corporation. KYMRIAH® (tisagenlecleucel): highlights of prescribing information. 2022. Available from: https://www.fda.gov/media/107296/download?attachment. [Accessed 1 Jun 2022].
National Institute for Health and Care Excellence. Mosunetuzumab for treating relapsed or refractory follicular lymphoma [TA892]. National Institute for Health and Care Excellence,, London, UK. 2023. Available from: https://www.nice.org.uk/guidance/ta892. [Accessed 18 Aug 2023].
Batlevi CL, Sha F, Alperovich A, Ni A, Smith K, Ying Z, et al. Follicular lymphoma in the modern era: survival, treatment outcomes, and identification of high-risk subgroups. Blood Cancer J. 2020;10(7):74. https://doi.org/10.1038/s41408-020-00340-z.
Casulo C, Byrtek M, Dawson KL, Zhou X, Farber CM, Flowers CR, et al. Early relapse of follicular lymphoma after rituximab plus cyclophosphamide, doxorubicin, vincristine, and prednisone defines patients at high risk for death: an analysis from the National LymphoCare Study. J Clin Oncol. 2015;33(23):2516–22. https://doi.org/10.1200/jco.2014.59.7534.
US FDA. FDA grants accelerated approval to mosunetuzumab-axgb for relapsed or refractory follicular lymphoma. 2022. Available from: https://www.fda.gov/drugs/resources-information-approved-drugs/fda-grants-accelerated-approval-mosunetuzumab-axgb-relapsed-or-refractory-follicular-lymphoma. [Accessed 27 Oct 2023].
Genentech Inc. LUNSUMIO™ (mosunetuzumab-axgb): highlights of prescribing information. 2022. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2022/761263s000lbl.pdf. [Accessed 3 Jan 2023].
Budde LE, Sehn LH, Matasar M, Schuster SJ, Assouline S, Giri P, et al. Safety and efficacy of mosunetuzumab, a bispecific antibody, in patients with relapsed or refractory follicular lymphoma: a single-arm, multicentre, phase 2 study. Lancet Oncol. 2022;23(8):1055–65. https://doi.org/10.1016/s1470-2045(22)00335-7.
United States Bureau of Labor Statistics. Consumer price index for all urban consumers: medical care (CUSR0000SAM). 2022. Available from: https://www.bls.gov/data/. [Accessed 5 Dec 2022].
Sullivan SD, Mauskopf JA, Augustovski F, Jaime Caro J, Lee KM, Minchin M, et al. Budget impact analysis: principles of good practice: report of the ISPOR 2012 Budget Impact Analysis Good Practice II Task Force. Value Health. 2014;17(1):5–14. https://doi.org/10.1016/j.jval.2013.08.2291.
US Census Bureau. 2017 national population projections datasets, Table 1. Projected population by single year of age, sex, race, and hispanic origin for the United States: 2016 to 2060. Available from: https://www.census.gov/content/census/en/data/datasets/2017/demo/popproj/2017-popproj.html. [Accessed 6 Dec 2022].
SEER. Non-Hodgkin lymphoma: people alive with cancer (U.S. prevalence) on January 1, 2019. 2019. Available from: https://seer.cancer.gov/explorer/application.html. [Accessed 6 Dec 2022].
Link BK, Day BM, Zhou X, Zelenetz AD, Dawson KL, Cerhan JR, et al. Second-line and subsequent therapy and outcomes for follicular lymphoma in the United States: data from the observational National LymphoCare Study. Br J Haematol. 2019;184(4):660–3. https://doi.org/10.1111/bjh.15149.
Appukkuttan S, Yaldo A, Gharibo M, Babajanyan S, Duchesneau E, Zichlin ML, et al. A budget impact analysis of the introduction of copanlisib for treatment of relapsed follicular lymphoma in the United States. J Manag Care Spec Pharm. 2019;25(4):437–46. https://doi.org/10.18553/jmcp.2019.18259.
Unpublished data on file, Genentech Inc., 2023
Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5(1):13. https://doi.org/10.1186/1471-2288-5-13.
AnalySource®. Reprinted with permission by First Databank, Inc. All rights reserved. 2023. Available from: https://www.analysource.com/. [Accessed 10 Mar 2023].
Genentech Inc. RITUXAN® (rituximab) injection: highlights of prescribing information. 2021. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/103705s5464lbl.pdf. [Accessed 18 Apr 2022].
Genentech Inc. GAZYVA® (obinutuzumab): highlights of prescribing information. 2022. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2022/125486s029lbl.pdf. [Accessed 18 Apr 2022].
Teva Pharmaceuticals USA Inc. BENDEKA® (bendamustine hydrochloride injection): highlights of prescribing information. 2021. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2015/208194s000lbl.pdf. [Accessed 18 Apr 2022].
Centers for Medicare & Medicaid Services. Physician fee schedule. 2022. Available from: https://www.cms.gov/medicare/physician-fee-schedule/search/overview. [Accessed 23 Jan 2024].
Liu R, Oluwole OO, Diakite I, Botteman MF, Snider JT, Locke FL. Cost effectiveness of axicabtagene ciloleucel versus tisagenlecleucel for adult patients with relapsed or refractory large B-cell lymphoma after two or more lines of systemic therapy in the United States. J Med Econ. 2021;24(1):458–68. https://doi.org/10.1080/13696998.2021.1901721.
Fowler NH, Dickinson M, Dreyling M, Martinez-Lopez J, Kolstad A, Butler J, et al. Tisagenlecleucel in adult relapsed or refractory follicular lymphoma: the phase 2 ELARA trial. Nat Med. 2022;28(2):325–32. https://doi.org/10.1038/s41591-021-01622-0.
HCUP Fast Stats. Trends in inpatient stays. 2020. Available from: https://datatools.ahrq.gov/hcup-fast-stats/?type=tab&tab=hcupfseds. [Accessed 5 Dec 2022].
Abramson JS, Siddiqi T, Garcia J, Dehner C, Kim Y, Nguyen A, et al. Cytokine release syndrome and neurological event costs in lisocabtagene maraleucel-treated patients in the TRANSCEND NHL 001 trial. Blood Adv. 2021;5(6):1695–705. https://doi.org/10.1182/bloodadvances.2020003531.
Genentech Inc. ACTEMRA® (tocilizumab): highlights of prescribing information. 2022. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2017/125276s114lbl.pdf. [Accessed 10 Dec 2022].
Centers for Medicare & Medicaid Services. Clinical Diagnostic Laboratory Fee Schedule. 2022. Available from: https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/ClinicalLabFeeSched/Clinical-Laboratory-Fee-Schedule-Files. [Accessed 23 Jan 2024].
April 2023 Medicare Part B Drug and Biological Average Sales Price Quarterly Payment files. 2023. Available from: https://www.cms.gov/medicare/medicare-part-b-drug-average-sales-price/2023-asp-drug-pricing-files. [Accessed 14 Dec 2023].
April 2023 Addendum B. OPPS Payment by HCPCS Code for CY 2023. 2023. Available from: https://www.cms.gov/medicare/medicare-fee-service-payment/hospitaloutpatientpps/addendum-and-addendum-b-updates/april-2023. [Accessed 19 Dec 2023].
US Census Bureau. 2023 population projections for the nation by age, sex, race, Hispanic origin and nativity. Available from: https://www.census.gov/newsroom/press-kits/2023/population-projections.html. [Accessed 4 Dec 2023].
Howlader N, Noone A, Krapcho M, Miller D, Bishop K, Kosary C et al. SEER Cancer Statistics Review (CSR) 1975-2014. Cancer prevalence tables, January 1, 2014. 2017. Available from: https://seer.cancer.gov/csr/1975_2014/. [Accessed 12 Dec 2023].
Fulton Z, Dandamudi N. Epidemiology: follicular lymphoma. In: NHL. Follicular lymphoma forecast and market analysis to 2025. Available from: https://pharmastore.informa.com/product/nhl-follicular-lymphoma/. [Accessed 12 Dec 2023].
Potnis KC, Di M, Isufi I, Gowda L, Seropian SE, Foss FM, et al. Cost-effectiveness of chimeric antigen receptor T-cell therapy in adults with relapsed or refractory follicular lymphoma. Blood Adv. 2023;7(5):801–10. https://doi.org/10.1182/bloodadvances.2022008097.
Memorial Sloan Kettering Cancer Center. CAR T cell therapy: a guide for adult patients & caregivers. 2023. Available from: https://www.mskcc.org/cancer-care/patient-education/car-cell-therapy-guide-adult-patients-caregivers. [Accessed 30 Nov 2023].
Cho SK, Manzoor BS, Sail KR, Parisé H, Ravelo A, Shapouri S, et al. Budget impact of 12-month fixed treatment duration venetoclax in combination with obinutuzumab in previously untreated chronic lymphocytic leukemia patients in the United States. Pharmacoeconomics. 2020;38(9):941–51. https://doi.org/10.1007/s40273-020-00919-1.
Appukkuttan S, Farej R, Miles L, Purser M, Wen L. Budget impact analysis of darolutamide for treatment of nonmetastatic castration-resistant prostate cancer. J Manag Care Spec Pharm. 2021;27(2):166–74. https://doi.org/10.18553/jmcp.2020.20330.
Cai B, Zhou ZY, Xue W, Hazra NC, Singh M, Mishra D, et al. Budget impact of capmatinib for adults with metastatic non-small cell lung cancer harboring a MET exon 14 skipping mutation in the United States. J Med Econ. 2021;24(1):131–9. https://doi.org/10.1080/13696998.2020.1867470.
Liu S, Yang K, Carter J, Zimmerman T, Tang B. POSA145 budget impact of zanubrutinib to treat relapsed or refractory marginal zone lymphoma from a payer perspective in the United States. Value Health. 2022;25(1):S62. https://doi.org/10.1016/j.jval.2021.11.288.
Davies KR, Kamalakar R, Yu J, Huang Y, Wang A, Sail K, et al. Health care resource utilization and costs of CAR T therapy in patients with large B-cell lymphoma: a retrospective US claims database analysis. Blood. 2022;140(Suppl 1):5058–9. https://doi.org/10.1182/blood-2022-157758.
Oluwole OO, Ray MD, Zur R, Little A, Ferrufino C, Doble B, et al. Cost-effectiveness of axicabtagene ciloleucel versus mosunetuzumab in relapsed/refractory follicular lymphoma in the US. Blood. 2023;142(Suppl 1):5082. https://doi.org/10.1182/blood-2023-186548.
Keating SJ, Gu T, Jun MP, McBride A. Health care resource utilization and total costs of care among patients with diffuse large B cell lymphoma treated with chimeric antigen receptor T cell therapy in the United States. Transplant Cell Ther. 2022;28(7):404.e1-6. https://doi.org/10.1016/j.jtct.2022.03.021.
Maziarz RT, Yang H, Liu Q, Wang T, Zhao J, Lim S, et al. Real-world healthcare resource utilization and costs associated with tisagenlecleucel and axicabtagene ciloleucel among patients with diffuse large B-cell lymphoma: an analysis of hospital data in the United States. Leuk Lymphoma. 2022;63:2052–62. https://doi.org/10.1080/10428194.2022.2060503.
Schuster SJ, Sehn LH, Bartlett NL, Matasar M, Assouline S, Giri P, et al. Mosunetuzumab monotherapy continues to demonstrate durable responses in patients with relapsed and/or refractory follicular lymphoma after ≥2 prior therapies: 3-year follow-up from a pivotal phase II study. Blood. 2023;142:603. https://doi.org/10.1182/blood-2023-173692.
Neelapu SS, Chavez JC, Sehgal A, Epperla N, Ulrickson ML, Bachy E, et al. Three-year follow-up analysis of axicabtagene ciloleucel in relapsed/refractory indolent non-Hodgkin lymphoma (ZUMA-5). Blood. 2023. https://doi.org/10.1182/blood.2023021243.
Neelapu SS, Chavez JC, Sehgal AR, Epperla N, Ulrickson ML, Bachy E, et al. Axicabtagene ciloleucel (Axi-Cel) in patients with relapsed/refractory indolent non-Hodgkin lymphoma: 4-year follow-up from the phase 2 ZUMA-5 trial. Blood. 2023;142(Suppl 1):4868. https://doi.org/10.1182/blood-2023-174914.
Schuster SJ, Fowler N, Dickinson M, Martinez-Lopez J, Kolstad A, Butler J, et al. Clinical outcomes of patients with relapsed/refractory follicular lymphoma treated with tisagenlecleucel: phase 2 Elara 3-year follow-up. Blood. 2023;142(Suppl 1):601. https://doi.org/10.1182/blood-2023-180936.
Leonard JP, Trneny M, Offner F, Mayer J, Zhang H, Nowakowski GS, et al. Five-year results and overall survival update from the phase 3 randomized study augment: lenalidomide plus rituximab (R2) vs rituximab plus placebo in patients with relapsed/refractory indolent non-Hodgkin lymphoma. Blood. 2022;140(Suppl. 1):561–3. https://doi.org/10.1182/blood-2022-158631.
Gribben JG, Ghione P, Palomba ML, Ray MD, Limbrick-Oldfield EH, Kanters S, et al. An updated comparison of clinical outcomes from 4-year follow-up of Zuma-5 (axicabtagene ciloleucel) and the international Scholar-5 external control cohort in relapsed/refractory follicular lymphoma. Blood. 2023;142(Suppl. 1):4869. https://doi.org/10.1182/blood-2023-186842.
Briggs A, Sculpher M, Claxton K. Decision modelling for health economic evaluation. Oxford: Oxford University Press; 2006.
Sehn LH, Goy A, Offner FC, Martinelli G, Caballero MD, Gadeberg O, et al. Randomized phase II trial comparing obinutuzumab (GA101) with rituximab in patients with relapsed CD20+ indolent B-cell non-Hodgkin lymphoma: final analysis of the GAUSS Study. J Clin Oncol. 2015;33(30):3467–74. https://doi.org/10.1200/JCO.2014.59.2139.
Rummel M, Kaiser U, Balser C, Stauch M, Brugger W, Welslau M, et al. Bendamustine plus rituximab versus fludarabine plus rituximab for patients with relapsed indolent and mantle-cell lymphomas: a multicentre, randomised, open-label, non-inferiority phase 3 trial. Lancet Oncol. 2016;17(1):57–66. https://doi.org/10.1016/s1470-2045(15)00447-7.
van Oers MH, Van Glabbeke M, Giurgea L, Klasa R, Marcus RE, Wolf M, et al. Rituximab maintenance treatment of relapsed/resistant follicular non-Hodgkin’s lymphoma: long-term outcome of the EORTC 20981 phase III randomized intergroup study. J Clin Oncol. 2010;28(17):2853–8. https://doi.org/10.1200/jco.2009.26.5827.
Sehn LH, Chua N, Mayer J, Dueck G, Trněný M, Bouabdallah K, et al. Obinutuzumab plus bendamustine versus bendamustine monotherapy in patients with rituximab-refractory indolent non-Hodgkin lymphoma (GADOLIN): a randomised, controlled, open-label, multicentre, phase 3 trial. Lancet Oncol. 2016;17(8):1081–93. https://doi.org/10.1016/s1470-2045(16)30097-3.
Center for Drug Evaluation and Research (CDER). NDA/BLA multi‐disciplinary review and evaluation 213400 - Tazverik (tazemetostat). 2019.
Celgene Corporation. REVLIMID (lenalidomide): highlights of prescribing information. 2021. Available from: https://www.accessdata.fda.gov/drugsatfda_docs/label/2019/021880s057lbl.pdf. [Accessed 18 Apr 2022].
Bristol Myers Squibb. R2 revlimid/rituximab promotional brochure. 2021. Available from: https://media.revlimidhcp.com/wp-content/uploads/2021/11/R2-Efficacy.pdf. [Accessed 23 Jan 2024].
Jacobson CA, Chavez JC, Sehgal AR, William BM, Munoz J, Salles G, et al. Axicabtagene ciloleucel in relapsed or refractory indolent non-Hodgkin lymphoma (ZUMA-5): a single-arm, multicentre, phase 2 trial. Lancet Oncol. 2022;23(1):91–103. https://doi.org/10.1016/s1470-2045(21)00591-x.
US FDA. Multi-disciplinary review and evaluation. BLA 125643/394 clinical review and evaluation: Yescarta (axicabtagene ciloleucel). 2022. Available from: https://fda.report/media/157687/April-1-2022-Clinical-Review-and-Evaluation-YESCART_0.pdf. [Accessed 23 Jan 2024].
Acknowledgments
The authors acknowledge the medical writing support provided by Eric Zuk (Medicus Economics, LLC) funded by Genentech, Inc. and the third-party medical editorial assistance provided by Ashfield MedComms, an Inizio company, funded by F. Hoffmann-La Roche Ltd.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The design, study conduct, and financial support for the study were provided by F. Hoffmann-La Roche Ltd. and Genentech, Inc.
Conflicts of Interest/Competing Interests
Shih-Wen Lin, Sheila Shapouri, Mei Wu, and Eunice Kim are employees of Genentech, Inc. and may own stocks/and or options from F. Hoffmann-La Roche Ltd. Hélène Parisé and Eric Bercaw are employees of Medicus Economics, LLC and received consulting fees for research from Genentech, Inc. Matthew Matasar is an employee of the Rutgers Cancer Institute of New Jersey. He has appointments for consultancy or is an advisory board member to Genentech, Inc., F. Hoffmann-La Roche Ltd, Bayer, Juno, Seattle Genetics, Takeda, Teva, and Merck; has institutional research funding from Genentech, Inc., F. Hoffmann-La Roche Ltd, Bayer, GM Biosciences, Immunovaccine Technologies, Janssen, Pharmacyclics, and Seattle Genetics; has received honoraria or stipends from Genentech, Inc., F. Hoffmann-La Roche Ltd, ADC Therapeutics, AstraZeneca, Bayer, BMS, Celgene, Epizyme, Immunovaccine Technologies, IMV Therapeutics, Janssen, Kite, Pharmacyclics, Regeneron, Seagen, Seattle Genetics, Takeda, and Teva; and he owns stocks/and or options from Merck.
Ethics Approval
Not applicable.
Consent to Participate
Not applicable.
Consent for Publication
Not applicable.
Availability of Data and Material
The data that support the findings of this study are available in this article. The model is not publicly available because of its intrinsic commercial value and cannot be shared for legal reasons.
Code Availability
Not applicable.
Authors’ Contributions
Genentech, Inc. and Medicus Economics, LLC participated in the design of the research, the analysis and interpretation of finding, and in the manuscript writing, review, and approval. All authors contributed to the development of the manuscript and maintained control over the final content.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Lin, SW., Shapouri, S., Parisé, H. et al. Budget Impact of Introducing Fixed-Duration Mosunetuzumab for the Treatment of Relapsed or Refractory Follicular Lymphoma After Two or More Lines of Systemic Therapy in the USA. PharmacoEconomics 42, 569–582 (2024). https://doi.org/10.1007/s40273-024-01358-y
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40273-024-01358-y