Abstract
Introduction
Concerns of the persistence and severity of the adverse effects of fluoroquinolones, mainly involving the nervous system, muscles and joints, resulted in the 2018 referral procedure led by the European Medicines Agency (EMA). They advised to stop prescribing fluoroquinolones for infections of mild severity or of a presumed self-limiting course and for prevention of infections, plus to restrict prescriptions in cases of milder infections where other treatment options are available, and restrict in at-risk populations. We aimed to examine whether the impact of EMA regulatory interventions implemented throughout 2018–2019 had an impact on fluoroquinolone prescribing rates.
Methods
A retrospective population-based cohort study was conducted using electronic health care records from six European countries between 2016 and 2021. We analysed monthly incident fluoroquinolone use rates overall and for each fluoroquinolone active substance through flexible modelling via segmented regression to detect time points of trend changes, in monthly percentage change (MPC).
Results
The incidence of fluoroquinolone use ranged from 0.7 to 8.0/1000 persons per month over all calendar years. While changes in fluoroquinolone prescriptions were observed over time across countries, these were inconsistent and did not seem to be temporally related to EMA interventions (e.g., Belgium: February/May 2018, MPC − 33.3%, 95% confidence interval [CI] − 35.9 to − 30.7; Germany: February/May 2019, MPC − 12.6%, 95% CI − 13.7 to − 11.6]; UK: January/April 2016, MPC − 4.9%, 95% CI − 6.2 to − 3.6).
Conclusion
The regulatory action associated with the 2018 referral did not seem to have relevant effects on fluoroquinolone prescribing in primary care.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
The impact of European Medicines Agency (EMA) regulatory interventions to reduce fluoroquinolone use in 2018–2019 is unknown. |
In six countries, the regulatory action did not seem to have relevant effects on fluoroquinolone prescribing in primary care. |
1 Introduction
Fluoroquinolones are broad spectrum antimicrobials used in managing various bacterial infections [1, 2]. Over the last decade, it has become increasingly clear that use of fluoroquinolones is associated with increased risk of serious and disabling adverse events. These events, mainly involving tendons, muscles and the nervous system, can be long-lasting and sometimes irreversible [3,4,5]. Additionally, the risk of adverse events seemed to be dose-dependent and modified by co-medication such as corticosteroids [3, 6]. Due to the concerns about serious harm to patients, the European Medicines Agency (EMA) conducted a pharmacovigilance referral procedure that re-assessed adverse drug reactions and the benefit-risk balance of fluoroquinolones for systemic and inhalation use [7]. In November 2018, the EMA confirmed the presence and severity of fluoroquinolone-induced adverse events, and that risks clearly exceeded benefits for some indications and a subset of users at increased risk for adverse events. Consequently, the EMA advised to stop prescribing fluoroquinolones for infections of mild severity or of a presumed self-limiting course and for prevention of infections, and to restrict prescriptions in case of milder infections where other treatment options are available and in at-risk populations [7]; no restriction of fluroquinolones use was issued for elderly patients. Revised indications, warnings, and other measures such as direct healthcare professional communications (DHPCs) were implemented in European Union (EU) member states [2]. Although these national communications might differ across EU countries, it could involve media campaigns and professional societies and medical associations directly reaching physicians and healthcare organisations.
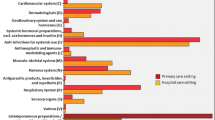
This drug utilisation study (DUS) commissioned by the EMA aimed to describe fluoroquinolone prescriptions in the EU and determine the potential impact of regulatory interventions taken to reduce the use of fluoroquinolones. It focuses on the primary care setting, where prescriptions of fluoroquinolone may be most common, while the severity of infections may be relatively low compared with the potential harm. The objectives are to determine patterns over time for (1) monthly incident fluoroquinolone prescriptions, both overall and stratified by on-label and off-label, and determine early discontinuation of a prescription; (2) prescriber’s compliance with revised product warnings for use in patients at increased risk of harm; and (3) monthly incident prescription rates for alternative antibiotics prescribed in patients where fluoroquinolones have previously been prescribed or discontinued.
2 Methods
2.1 Study Setting and Design
We conducted a retrospective population-based cohort study with a time series regression model to identify the potential impact of regulatory interventions on prescribing trends of fluoroquinolones in the EU. Electronic healthcare records were used from primary care databases across six European countries where fluoroquinolones were marketed: Longitudinal Patient Database (LPD) Belgium (Belgium), LPD France (France), Disease Analyser Germany (Germany), Integrated Primary Care Information (The Netherlands), SIDIAP (Catalonia Spain) and IQVIA Medical Research Data (UK). The study focused on primary care databases. However, Germany has no mandatory general practice (GP) system and patients have free choice of specialist. As a result, data were collected from visits to GP and specialists such as otolaryngology, dermatology or obstetrics/gynaecology (see further details in Table S2 of the electronic supplementary material (ESM). Data from all these databases have independently adopted the Observational Medical Outcomes Partnership (OMOP) Common Data Model (CDM) to allow harmonisation of their data with others. The CDM combined with its standardised content, ensures that research methods can be systematically applied to any data partner to analyse results across cohorts. The OMOP CDM is developed and maintained by the Observational Health Data Sciences and Informatics (OHDSI) initiative, described in detail at https://ohdsi.github.io/CommonDataModel/ and in The Book of OHDSI: http://book.ohdsi.org. Further details on data sources can be found in the study protocol (EU PAS Register, identifier EUPAS37856). This study is registered at the European Network of Centres for Pharmacoepidemiology and Pharmacovigilance (ENCEPP).
From the abovementioned databases, we considered data from 1 January 2016 until the latest available data cut-off, as shown in ESM Table S1. An additional censoring rule was applied to exclude the last 6 months of records within each database (see ESM Table S1 for further details on the observation period). Active individuals were defined as persons contributing for more than 12 months in each of the databases. Cohort entry was defined as the latest of the study start date or at the end date of the 12 months of registration with the healthcare practice. Cohort exit was defined by the earliest of the following criteria: date of patient death, date of patient exit (deregister) from a contributing data provider (GP) when available, last consultation date, date that a contributing provider exited the data source (last collection date), or end of the study period (latest data cut-off) (ESM Table S1).
2.2 Study Population
We included as the study population all persons with non-missing data on age and sex, and continuous enrolment in each of the aforementioned databases for more than 12 months. Categories of subpopulations of interest were investigated and defined by age group, sex, active fluoroquinolone substance, indication of use, on- and off-label use and country. For each objective, applied subgroups were predefined in the protocol (EUPAS37856). Furthermore, exposure of interest, risk groups of interest (at-risk of tendinitis and tendon rupture, at-risk of aortic dissection and aneurysm and concomitant or recent systemic corticosteroid exposure) and alternative antibiotics exposure were derived from the data sources and analysed in the study population. More details about the subpopulations and risk groups of interest are presented in the Methods section of the ESM.
2.3 Exposure of Interest
From the study population, we identified prescriptions of fluoroquinolones and defined those as our exposed cohort. The native drug coding structure for each country was derived from prescriptions issued within the primary care setting and standardised to RxNorm concepts, which contains details of ingredients, strengths and formulation at clinical drug level. Rules applied before standardisation to RxNorm concepts across databases are presented in ESM Fig. S1. The episodes of each prescription were obtained by subtracting the drug exposure start date from the drug exposure end date. A gap of more than 30 days between prescriptions signalled the end of the treatment episode [8], potentially including multiple prescriptions (Fig. 1). Incident fluoroquinolone use was defined as a recorded prescription of fluoroquinolone in patients without any fluoroquinolone use in the previous 30 days, irrespective of indication, calculated at substance level. The exposed cohort was further stratified by the following fluoroquinolone active substances of interest: ciprofloxacin, levofloxacin, lomefloxacin, ofloxacin, moxifloxacin and norfloxacin. Lomefloxacin was only used in France, while norfloxacin was used in all countries studied; however, norfloxacin use was ≤ 5 in any month in the UK. Therefore, masking rules was applied as appropriate. Although stratification by route of administration (systemic or inhaled) was planned, records of other than ‘systemic’ or ‘unknown’ routes were not available in the data sources.
Schematic depiction ascertainment of treatment episodes. A gap of more than 30 days between prescriptions signalled the end of the treatment episode (Case A). If the interval between fluoroquinolone prescriptions was ≤ 30 days (Case B), these will be considered the same treatment episode and attributed to the first fluoroquinolone type prescribed (drug A in this case). As the choice of 30 days was somewhat arbitrary, sensitivity analysis was conducted by varying the look-back window to 60, 90 and 180 days. The exact period to determine an incident prescription depends on the average duration of treatment, and the average fluoroquinolone treatment duration depends on the indication. Durations may vary from 3 days for acute uncomplicated cystitis, up to 4–6 weeks for osteomyelitis; on average, treatment duration is between 7 and 14 days
2.4 Statistical Analysis
All results are presented separately per country. Age was assessed at the start of each calendar year, and sex was regarded as a fixed covariate throughout the study period.
We described monthly incident fluoroquinolone use by calculating the number of incident users per 1000 persons per month: \((i)=\frac{{\text{Incident new fluoroquinolone users in the month}}}{{\text{Total active population in the month}}} \times 1000\). The denominator consisted of the persons contributing at least 1 day of follow-up time in that calendar month, without incident use in the previous calendar month. One individual could have multiple incident fluoroquinolone prescriptions. Since calculations for the number of persons was taken monthly and were summed to the population level, it was not necessary to calculate the attributed person-time as any deviations would be minimal. Monthly incident fluoroquinolone prescription rates were presented overall and stratified for age (< 18, 18–75 and > 75 years), sex (male/female), fluoroquinolone active substance type, treatment duration (six different strata from short duration [0–6 days] to very long duration [≥ 28 days]), line of treatment (first, second or third), indication and on- versus off-label use. Specific algorithms were used to first identify indications for which fluoroquinolones were used, and second, determine on- and off-label classification based on information from the summary of product characteristics (SmPC), the article 31 referral plus the UK and Dutch treatment prescribing guidelines [2, 9, 10]. These were used in combination to classify fluoroquinolone indications at a class level as on- or off-label. For instance, acute bronchitis or pharyngitis are restricted or removed based on the fluoroquinolone SmPCs and article 31, and were subsequently classified as off-label. Another off-label classification example is when indication is not recommended as first- or second-line treatments (e.g., pneumonia due to gram-negative). More details and examples on these algorithms are presented in the Methods section of the ESM (ESM Fig. S3). For analyses stratified by indication, we did not further differentiate between on- or off-label use. Use in at-risk persons was reported per 1000 persons per month, whereas early discontinuation and use of alternative antibiotics were expressed per 1000 monthly incident fluoroquinolone prescriptions that month.
We further analysed monthly incident fluoroquinolone prescription rate overall and for each fluoroquinolone active substance separately through flexible modelling via segmented regression to detect time points of trend changes. The approach was used with no prespecified breakpoints but a maximum number of 20. The best model was selected according to the Bayesian Information Criterion (BIC) implemented using the selgmented command in R software. Data counts were modelled by a Poisson model on the log-linear scale, with calendar month as an independent variable and monthly incidence rate as a dependent variable. In addition, the age-standardised rate of incident fluoroquinolone prescription (standardised to European Standard Population 2013Footnote 1 [11]; see ESM Table S2), was also modelled, but using a segmented linear regression. Age-standardised rates were not modelled for individual fluoroquinolones. The final model was described by the time periods where a trend change was detected and the corresponding monthly percentage change (MPC) (or coefficient for age-standardised linear model) for each segmented block of time with 95% confidence intervals (CIs). Seasonality has not been tested in the data, but the segmented model allows for seasonal variations if they are identified by changes in the slope of the model. The final model predicted moments of change in trend and was described in relation to country-specific calendar times (Table 1) during which the regulatory actions based on the Referral under Article 31 of Directive 2001/83/EC [2] were implemented:
-
Restrictions of prescriptions for infections of mild severity or of presumed self-limiting course, as defined in section 4.1 of the SmPC of all antimicrobials falling under the fluoroquinolone group with market authorisation per country (hereafter: SmPC).
-
Warnings and precautions of use in section 4.4 of the SmPC on tendinitis and tendon rupture, aortic dissection and aneurysm, and in patients with concomitant use of corticosteroids.
-
DHPC sent to healthcare professionals to increase awareness on the long-term, persistent, potentially irreversible adverse events and the associated changes to the SmPC. These communications were disseminated nationally through direct communication to healthcare professionals, and media campaigns if considered appropriate by National Competent Authorities (NCAs).
3 Results
The study population included between 16 and 21 million patients each month during the study period (2016–2021) [ESM Table S3].
The incidence of fluoroquinolone prescriptions across countries ranged from 0.7/1000 persons per month (UK) to 8.0/1000 persons per month (Spain) during follow-up. Prescriptions were highest in persons aged > 75 years of age in all countries (ESM Fig. S6). Indications for fluoroquinolone prescriptions could often not be classified; unknown indications ranged between 31 and 94.0% across countries (ESM Table S8). For the minority of persons in which the indication could be classified, respiratory tract infections, urinary tract infections (uncomplicated) and ear infections were the most frequent indications. For respiratory tract infections, we observed clear seasonal variations in Belgium, Germany, and Spain. These variations suddenly dropped from May 2018 in Belgium (ESM Fig. S7). Additional stratifications, including on- and off-label, are shown in ESM Figs. S13–S18.
Other indicators of changes in prescribing behaviour by healthcare professionals, such as early discontinuation or prescription rates for alternative antibiotics (prescribed in patients where systemic use of fluoroquinolones has been previously used), or for at-risk groups showed no changes after the regulatory interventions across countries (ESM Figs. S19–S25). Sensitivity analyses varying the time period to classify incident fluoroquinolone use and indications did not meaningfully change the rate of fluoroquinolone use (ESM Tables S5 and S6). Similarly, restricting the look-back period for assessing at-risk groups did not substantially change the number of at-risk fluoroquinolone users detected (ESM Table S7).
3.1 Segmented Point Regression of Overall Fluoroquinolone Prescriptions
In Belgium, seasonal patterns were observed, with peaks every year in January/February and lowest levels in June/July. There was a large drop in prescriptions around February/May 2018 (MPC − 33.3%, 95% CI − 35.9 to − 30.7), after which seasonal fluctuations continued at a lower level (Fig. 2 and Table 2). In France, prescription rates, on average, slightly decreased over time throughout follow-up with similar fluctuations per year (Fig. 3 and Table 3). In Germany, seasonal patterns were not pronounced although rates seemed higher in winter and lower in summer. A sharper decrease in prescriptions was seen from February to May 2019 (MPC − 12.6%, 95% CI − 13.7 to − 11.6) and prescription rates fluctuated at a lower level after this (Fig. 4 and Table 4). In the Netherlands, a drop in prescriptions was seen around December 2019 (MPC − 6.5%, 95% CI − 9.4 to − 3.4), followed by an increase around April 2020 (MPC 9.3%, 95% CI 7.2–11.4) and another decrease from August 2020 (MPC − 5.0%, 95% CI − 6.7 to − 3.2) [Fig. 5 and Table 5]. In Spain, after an initial drop in prescriptions in the first 3 months of 2016, there was a gradual increase over the first 20 months (MPC 0.4%, 95% CI 0.4–0.5) followed by a gradual drop from around December 2017 to June 2019 (MPC − 0.7%, 95% CI − 0.7 to − 0.6) and a steeper decrease thereafter (MPC − 2.3%, 95% CI − 2.3 to − 2.2) [Fig. 6 and Table 6]. In the UK, there was a drop in the first 3.5 months of the study follow-up (MPC − 4.9%, 95% CI − 6.2 to − 3.6) followed by steady rates showing seasonal variation, with peaks in winter. From November 2018 onwards, before implementation of regulatory interventions, there was a general reduction in prescriptions (Fig. 7 and Table 7). The most recent prescription rates were about 25% lower than average rates before the decrease started at around November 2018. Stratifications by substance are shown in ESM Figs. S26–S31.
Incidence rate of all fluoroquinolone use with segmented regression for Belgium. The grey shaded interval represents the SmPC implementation period for the fluoroquinolone warnings (24 February 2019–17 April 2020) and the associated DHPC (1 April 2019) [blue line]. SmPC summary of product characteristics, DHPC direct healthcare professional communication
Incidence rate of all fluoroquinolone use with segmented regression for France. The grey shaded interval represents the SmPC implementation dates for the fluoroquinolone warnings (2 August 2019–28 May 2020) and the associated DHPC date (10 April 2019) [blue line]. Although several dates were reported for the SmPC implementations in France (see Table 1 for the exact dates), the graph shows the interval between the first and last dates. SmPC summary of product characteristics, DHPC direct healthcare professional communication
Incidence rate of all fluoroquinolone use with segmented regression for Germany. The grey shaded interval represents the SmPC implementation period for the fluoroquinolone warnings (22 March 2019–11 December 2019) and the associated DHPC date (8 April 2019) [blue line]. SmPC summary of product characteristics, DHPC direct healthcare professional communication
Incidence rate of all fluoroquinolone use with segmented regression for the Netherlands. The grey shaded interval represents the SmPC implementation period (14 February 2019–30 March 2020) for the fluoroquinolone warnings and the associated DHPC date (9 April 2019) [blue line]. SmPC summary of product characteristics, DHPC direct healthcare professional communication
Incidence rate of all fluoroquinolone use with segmented regression for Spain. The grey shaded interval represents the SmPC implementation dates/period for the fluoroquinolone warnings (27 March 2019–2 July 2020 and 31 July 2020) and the associated DHPC date (8 April 2019) [blue line]. SmPC summary of product characteristics, DHPC direct healthcare professional communication
Incidence rate of all fluoroquinolone use with segmented regression for the UK. The grey shaded interval represents the SmPC implementation periods for the fluoroquinolone warnings (25 April 2019–23 December 2019 and 1 April 2020–18 May 2020) and the associated DHPC date (21 March 2019) [blue line]. SmPC summary of product characteristics, DHPC direct healthcare professional communication
3.2 Segmented Point Regression of Age-Standardised Rates in Overall Fluoroquinolone Use
The visualisation and linear regression of age-standardised rates, similar to the crude rates, did not show a decrease in incident fluroquinolone prescriptions after regulatory interventions across countries (Figs. S32–S37). In Belgium, age-standardised rates patterns were similar to crude rates. Spanish rates showed a linear pattern over the first 3 years, followed by a decline from around December 2018 to December 2020 (MPC − 9.4%, 95% CI − 13.0 to − 5.6). In France, Germany, the UK and the Netherlands, linear regression of age-standardised rates did not identify the changes seen in the analysis of the crude rates.
4 Discussion
This retrospective DUS examined the use of fluoroquinolones through prescriptions in primary care in six countries between 2016 and 2021, and explored whether the EMA regulatory interventions implemented throughout 2018–2019 had any impact on fluoroquinolone prescribing rates. Although we found reductions in prescription rates during follow-up, these were not temporally related to the implementation of regulatory interventions and were inconsistent across countries. Other indicators of changes in prescribing behaviour, such as early discontinuation or prescriptions of alternative antibiotics, were unaffected by regulatory interventions. Our findings did not support a relevant effect of regulatory interventions on fluoroquinolone prescriptions in primary care in the studied countries.
The lack of evident changes after interventions could indicate that these had, at best, low effectiveness and were not detectable in the primary care setting in these countries. Our findings were similar to studies performed in the United States (US). One US study reported a significant decrease in outpatient fluoroquinolone prescribing (by 39% reduction in total prescriptions per 1000 patient visits) after a multimodal stewardship intervention between 2016 and 2018 [12]. Yet, fluoroquinolone use declined before and after a US FDA black-box warning on fluoroquinolones in 2016, suggesting limited impact of regulatory changes [13]. Another US study in a large outpatient centre did not find a significant impact after the FDA black-box warning on fluoroquinolone prescribing trends between 2013 and 2018 [14]. Our findings may also indicate that the timeframe studied was too short to allow adequate dissemination of regulatory measures to healthcare practices and subsequent prescription rates. A systematic review on the effectiveness of UK regulatory risk communications assumed a 12-month lag time to evaluate the effects of country-wide interventions [15]. Although no lag time was implemented in our study, even considering that a 6-month follow-up time at study end was excluded, we would still have been able to observe any changes in fluoroquinolone prescriptions.
Possibly, one may argue that observing a lack of changes associated with regulatory interventions suggests that the data were somehow not well reflective of clinical practice. Yet, study setting and design support that the data reflect GP. Moreover, the absolute levels of fluoroquinolone prescriptions, the prescription patterns across countries, age groups, and main indications, and the avoidance in risk groups aligned well with known country differences and clinical guidelines [16,17,18].
Detection of any effect of regulatory interventions may have been obscured by decreases in prescriptions rates already occurring before implementation of regulatory interventions. In the UK, although the decreases started before implementation, regression analyses showed a reduction in prescriptions that later coincided with SmPC changes and DHPCs. Timing of this reduction also corresponded to EMA communications regarding fluoroquinolone restrictions (16 October 2018, Pharmacovigilance Risk Assessment Committee [PRAC] recommendation; November 2018, Committee for Medicinal Products for Human Use (CHMP) opinion; and March 2019, European Commission Decision) [7, 19]. Only a few studies have focused on such country-level dynamics of prescription rates of fluoroquinolones and factors influencing any changes. One study on German prescription data from community pharmacies found a significant downward trend also starting before the regulatory interventions [20]. Overall, decreases could be attributable to other factors influencing prescription behaviour such as antibiotic stewardships, or local changes in clinical guidance. Nevertheless, in our data, such decreases were of modest size, showing, at best, a reduction of prescriptions of around 25% in the UK; if any effect of regulatory interventions may have been obscured, the relevance of its effect was not supported by our data. Interestingly, in Spain, a decrease in prescriptions could be seen in the overall rates around March/April 2020, with a small increase in discontinuation rates and alternative antibiotic use rates. Although temporally related to the regulatory interventions more than 1 year earlier, this change coincided with the first wave of the coronavirus disease 2019 (COVID-19) pandemic hitting Western Europe. Considering the major changes due to the pandemic and the associated population-level interventions (e.g., dynamics of infectious diseases, or willingness and possibilities of visiting primary care physicians), this decrease of fluoroquinolone use and increase in alternative antibiotics in Spain was difficult to attribute to the regulatory interventions taken for fluoroquinolones. Further research may consider examining why, specifically in Spain, this time period was associated with drops in prescription rates of fluoroquinolones, or possibly overall antimicrobial prescriptions, and whether changes observed in Spain may have been driven by the COVID-19 pandemic changes. In Belgium, an absolute reduction as well as a reduction in seasonally fluctuating peaks in prescriptions was found to occur no later than the summer of 2018. This sudden drop was related to changes in reimbursement criteria of fluoroquinolones in Belgium. As of May 2018, fluoroquinolones, including ofloxacin, ciprofloxacin, norfloxacin, levofloxacin and moxifloxacin, are no longer reimbursed for the treatment of respiratory tract infections or uncomplicated urinary tract infections [21]. In the Netherlands, a drop in prescription rates in the regression analyses could be observed after implementation of regulatory interventions. However, the changes were, at best, modest and, for example, not reflected as breakpoints when modelling age-adjusted rates.
Several methodological considerations should be mentioned. First, we could not determine any potential impact of regulatory interventions on prescriptions in secondary care, including hospitals. Considering that hospitals include a higher density of healthcare professionals and may possess more professionalised or matured networks of disseminating safety information on medications, the impact of regulatory interventions may have been stronger or swifter there. Second, unknown indications were ranging from 37.7 to 94.1%. This may make our stratified analyses for indication, and estimates of ratio on/off-label, vulnerable to selection bias and accordingly introduce challenges in interpretation for these analyses. Moreover, our study included specific code lists and excluded symptom-related codes and general infection diagnoses codes, which may have led to an underestimation of the known indications in all the databases. Third, as data on medicine prescriptions did not equate to actual use, the algorithm for determining early discontinuation of fluoroquinolones may have underestimated true discontinuation. Vice versa, the early discontinuation proportion may have been overestimated due to the definition used (start of a new antibiotic before finishing the course of fluoroquinolone), as switching followed by early discontinuation might be actual add-on treatments. Fourth, it was not feasible to (manually) validate the automatic classification of key supporting variables in our retrospective data, e.g., indications for fluoroquinolone prescriptions, and, subsequently, classifications of on- or off-label use. Indications could only be indirectly identified using comprehensive code lists to classify indications on related data such as comorbidities. We could not exclude that missingness of information to classify indications may occur more often in persons where fluoroquinolone prescriptions truly changed across time. We used segmented regression methods to analyse time trends. This was a data-driven approach that allowed for seasonal trends to be observed if they occurred, but did not explicitly test for changes in fluoroquinolone use before and after regulatory intervention, or adjust for seasonality. This could be explored in further studies.
The strengths of our study included using a large number of patients per country, which increases precision to show any potential changes of prescriptions across time. Furthermore, use of the OMOP CDM increased comparability of results across countries. Lastly, findings seemed generalisable to the primary care situation in countries with a similar healthcare system where similar regulatory interventions were implemented.
5 Conclusion
The regulatory actions on reducing fluoroquinolone use associated with the 2018 referral was not associated with a significant impact on fluoroquinolone prescribing in primary care based on our analysis. For future work, researchers may consider looking into prescription changes in secondary care, potential country-specific changes, or to include longer follow-up time to evaluate potential lagged effects.
Notes
The age-standardised monthly usage rate was calculated as a weighted sum of the age-specific incident rates each month. The European Standard Population 2013 was used as the standard population for all time points and countries. Each age-specific rate was multiplied by the associated weight and summed to give the total age-standardised rate per month. For example, the age band 50–59 years was associated with 0.135.
References
Hooper DC. Mechanisms of action of antimicrobials: focus on fluoroquinolones. Clin Infect Dis. 2001;32:S9-15. https://doi.org/10.1086/319370.
PRAC. Referral under Article 31 of Directive 2001/83/EC resulting from pharmacovigilance data—quinolone and fluoroquinolone medicinal products for systemic and inhalation use. In: PRAC Assessment Report; 2018. https://www.ema.europa.eu/en/documents/referral/quinolone-fluoroquinolone-article-31-referral-assessment-report_en.pdf. Accessed 19 Nov 2022.
Morales DR, Slattery J, Pacurariu A, Pinheiro L, McGettigan P, Kurz X. Relative and absolute risk of tendon rupture with fluoroquinolone and concomitant fluoroquinolone/corticosteroid therapy: population-based nested case–control study. Clin Drug Investig. 2019;39:205–13. https://doi.org/10.1007/s40261-018-0729-y.
Etminan M, Brophy JM, Samii A. Oral fluoroquinolone use and risk of peripheral neuropathy: a pharmacoepidemiologic study. Neurology. 2014;83(14):1261–3. https://doi.org/10.1212/WNL.0000000000000846.
Lee C-C, Lee MG, Chen Y-S, Lee S-H, Chen Y-S, Chen S-C, et al. Risk of aortic dissection and aortic aneurysm in patients taking oral fluoroquinolone. JAMA Intern Med. 2015;175:1839–47. https://doi.org/10.1001/jamainternmed.2015.5389.
Kim GK. The risk of fluoroquinolone-induced tendinopathy and tendon rupture. J Clin Aesthet Dermatol. 2010;3:49–54.
European Medicines Agency. Quinolone- and fluoroquinolone-containing medicinal products; 2019. https://www.ema.europa.eu/en/medicines/human/referrals/quinolone-fluoroquinolone-containing-medicinal-products. Accessed 14 Feb 2022.
Pasternak B, Inghammar M, Svanström H. Fluoroquinolone use and risk of aortic aneurysm and dissection: nationwide cohort study. Br Med J. 2018;360: k678. https://doi.org/10.1136/bmj.k678.
NICE. Antimicrobial prescribing guidance—managing common infections; 2021. https://www.bnf.org/wp-content/uploads/2021/07/summary-antimicrobial-prescribing-guidance_july-21-for-BNF.pdf. Accessed 19 Nov 2022.
SWAB. Antimicrobial Stewardship—Algemene informatie; 2016. https://swab.nl/nl/antimicrobial-stewardship. Accessed 3 Aug 2020.
European Commission Eurostat. Revision of the European Standard Population: report of Eurostat’s task force; 2013. https://data.europa.eu/doi/10.2785/11470. Accessed 21 Apr 2021.
Lin K, Zahlanie Y, Ortwine JK, Mang NS, Wei W, Brown LS, et al. Decreased outpatient fluoroquinolone prescribing using a multimodal antimicrobial stewardship initiative. Open Forum Infect Dis. 2020;7: ofaa182. https://doi.org/10.1093/ofid/ofaa182.
Yarrington ME, Anderson DJ, Dodds Ashley E, Jones T, Davis A, Johnson M, et al. Impact of FDA black box warning on fluoroquinolone and alternative antibiotic use in southeastern US hospitals. Infect Control Hosp Epidemiol. 2019;40:1297–300. https://doi.org/10.1017/ice.2019.247.
Bratsman A, Mathias K, Laubscher R, Grigoryan L, Rose S. Outpatient fluoroquinolone prescribing patterns before and after US FDA boxed warning. Pharmacoepidemiol Drug Saf. 2020;29:701–7. https://doi.org/10.1002/pds.5018.
Weatherburn CJ, Guthrie B, Dreischulte T, Morales DR. Impact of medicines regulatory risk communications in the UK on prescribing and clinical outcomes: systematic review, time series analysis and meta-analysis. Br J Clin Pharmacol. 2020;86:698–710. https://doi.org/10.1111/bcp.14104.
Morales DR, Slattery J, Pinheiro L, Kurz X, Hedenmalm K. Indications for systemic fluoroquinolone therapy in Europe and prevalence of primary-care prescribing in France, Germany and the UK: descriptive population-based study. Clin Drug Investig. 2018;38:927–33. https://doi.org/10.1007/s40261-018-0684-7.
Adriaenssens N, Coenen S, Versporten A, Muller A, Minalu G, Faes C, et al. European Surveillance of Antimicrobial Consumption (ESAC): outpatient antibiotic use in Europe (1997–2009). J Antimicrob Chemother. 2011;66(Suppl 6):vi3–12. https://doi.org/10.1093/jac/dkr453.
Kabbani S, Hersh AL, Shapiro DJ, Fleming-Dutra KE, Pavia AT, Hicks LA. Opportunities to improve fluoroquinolone prescribing in the United States for adult ambulatory care visits. Clin Infect Dis. 2018;67:134–6. https://doi.org/10.1093/cid/ciy035.
FAMHP. Public hearing on quinolones and fluoroquinolones at EMA; 2018. https://www.famhp.be/en/news/public_hearing_on_quinolones_and_fluoroquinolones_at_ema. Accessed 14 Feb 2022.
Gradl G, Werning J, Enners S, Kieble M, Schulz M. Quality appraisal of ambulatory oral cephalosporin and fluoroquinolone use in the 16 German federal states from 2014–2019. Antibiotics. 2021;10:831. https://doi.org/10.3390/antibiotics10070831.
Vermeulen H, Coenen S, Hens N, Bruyndonckx R. Impact of changing reimbursement criteria on the use of fluoroquinolones in Belgium. J Antimicrob Chemother. 2021;76:2725–32. https://doi.org/10.1093/jac/dkab255.
Acknowledgements
The authors sincerely thank Dr Claire Burton and Dr Katia Verhamme for their contributions to the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was funded by the EMA.
Conflict of interest
This document expresses the opinion of the authors of this paper and may not be understood or quoted as being made on behalf of or reflecting the position of the EMA or one of its committees or working parties.
Data availability
Not applicable.
Code availability
Not applicable.
Ethics approval
This retrospective study using secondary data was conducted in accordance with the ethical standards of the institutional and national research committees and with the Declaration of Helsinki. The study protocol has been reviewed by the Institutional Review Boards of the respective databases. As this was a non-interventional observational study, there was no need for ethical approval in the Netherlands, UK, Belgium, Germany, and France. For SIDIAP (Spain), the scientific committee for SIDIAP studies and the local ethics committee evaluated the protocol before the study was carried out (#21/272-P).
Consent to participate
Informed consent was unnecessary as the study used only electronic health medical records, which had been de-identified prior to data access.
Consent for publication
Not applicable.
Author contributions
NFL, CF, TL, EM, HvB, LK, CR and DL are employees of IQVIA. All authors agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Ly, N.F., Flach, C., Lysen, T.S. et al. Impact of European Union Label Changes for Fluoroquinolone-Containing Medicinal Products for Systemic and Inhalation Use: Post-Referral Prescribing Trends. Drug Saf 46, 405–416 (2023). https://doi.org/10.1007/s40264-023-01286-4
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-023-01286-4