Abstract
Background
Several studies suggest a significant risk of hospitalization because of drug–drug interactions in the general population. However, to our knowledge, this risk has never been measured precisely in a large population.
Objective
We aimed to estimate the risk of emergency hospitalization associated with exposure to the contraindicated concomitant use of interacting drugs in the general population.
Methods
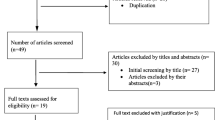
A self-controlled case-series analysis was carried out on a cohort of 150,000 subjects randomly selected from the French national health insurance database, between 01/01/2016 and 31/12/2016. Exposure to the contraindicated concomitant use of interacting drugs was defined as the overlapping period of dispensings of drugs contraindicated because of clinically meaningful drug–drug interactions. The main outcome, incidence rate ratios, comparing the incidence rate of emergency hospitalizations during each category of exposure time periods with that during the reference period, was estimated using the conditional Poisson regression model.
Results
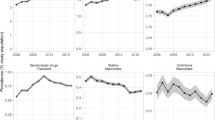
Over the study period, 967 subjects were exposed to at least one contraindicated concomitant use of interacting drug and 177 had been exposed and presented at least one emergency hospitalization. Compared to the unexposed follow-up time, the risk of emergency hospitalization increased during exposure to contraindicated concomitant use of interacting drug periods (incidence rate ratio: 2.41; 95% confidence interval 1.55–3.76). This could translate into 7200 (4500–8900) potentially preventable emergency hospitalizations yearly in France.
Conclusions
We evidenced an almost 2.5-fold increase in the risk of emergency hospitalizations during periods of exposure to contraindicated concomitant use of interacting drugs, with a potential public health impact exceeding 7000 preventable hospitalizations yearly in France. These results confirm the need to reinforce training in prescription practices and tools for prevention concerning contraindicated concomitant use of interacting drugs. These would especially concern drugs involved in an increase in long QT syndrome when associated such as citalopram, and highly prescribed drugs with a risk of overdose if co-prescribed with cytochrome P450 inhibitors, such as antigout and lipid-lowering drugs.


Similar content being viewed by others
References
Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2015;386:743–800.
Schumock GT, Li EC, Suda KJ, et al. National trends in prescription drug expenditures and projections for 2014. Am J Health Syst Pharm. 2014;71:482–99.
Abolhassani N, Castioni J, Marques-Vidal P, Vollenweider P, Waeber G. Determinants of change in polypharmacy status in Switzerland: the population-based CoLaus study. Eur J Clin Pharmacol. 2017;73:1187–94.
Wastesson JW, Minguez AC, Fastbom J, Maioli S, Johnell K. The composition of polypharmacy: a register-based study of Swedes aged 75 years and older. PLoS ONE. 2018;13: e0194892.
Guthrie B, Makubate B, Hernandez-Santiago V, Dreischulte T. The rising tide of polypharmacy and drug-drug interactions: population database analysis 1995–2010. BMC Med. 2015;13:74.
Kantor ED, Rehm CD, Haas JS, Chan AT, Giovannucci EL. Trends in prescription drug use among adults in the United States from 1999–2012. JAMA. 2015;314:1818–30.
Qato DM, Wilder J, Schumm LP, Gillet V, Alexander GC. Changes in prescription and over-the-counter medication and dietary supplement use among older adults in the United States, 2005 vs 2011. JAMA Intern Med. 2016;176:473–82.
Guillot J, Maumus-Robert S, Marceron A, Noize P, Pariente A, Bezin J. The burden of potentially inappropriate medications in chronic polypharmacy. J Clin Med. 2020;9:3728.
Létinier L, Cossin S, Mansiaux Y, et al. Risk of drug-drug interactions in out-hospital drug dispensings in France: results from the DRUG-Drug Interaction Prevalence Study. Front Pharmacol. 2019;10:265.
Chatsisvili A, Sapounidis I, Pavlidou G, et al. Potential drug-drug interactions in prescriptions dispensed in community pharmacies in Greece. Pharm World Sci. 2010;32:187–93.
Marzolini C, Elzi L, Gibbons S, et al. Prevalence of comedications and effect of potential drug-drug interactions in the Swiss HIV Cohort Study. Antivir Ther (Lond). 2010;15:413–23.
van Leeuwen RWF, Brundel DHS, Neef C, et al. Prevalence of potential drug-drug interactions in cancer patients treated with oral anticancer drugs. Br J Cancer. 2013;108:1071–8.
Nusair MB, Al-Azzam SI, Arabyat RM, Amawi HA, Alzoubi KH, Rabah AA. The prevalence and severity of potential drug-drug interactions among adult polypharmacy patients at outpatient clinics in Jordan. Saudi Pharm J. 2020;28:155–60.
Ren W, Liu Y, Zhang J, et al. Prevalence of potential drug-drug interactions in outpatients of a general hospital in China: a retrospective investigation. Int J Clin Pharm. 2020;42:1190–6.
Seymour RM, Routledge PA. Important drug-drug interactions in the elderly. Drugs Aging. 1998;12:485–94.
Becker ML, Kallewaard M, Caspers PWJ, Visser LE, Leufkens HGM, Stricker BHC. Hospitalisations and emergency department visits due to drug-drug interactions: a literature review. Pharmacoepidemiol Drug Saf. 2007;16:641–51.
Dechanont S, Maphanta S, Butthum B, Kongkaew C. Hospital admissions/visits associated with drug–drug interactions: a systematic review and meta-analysis. Pharmacoepidemiol Drug Saf. 2014;23:489–97.
Bykov K, Schneeweiss S, Glynn RJ, Mittleman MA, Gagne JJ. A case-crossover-based screening approach to identifying clinically relevant drug-drug interactions in electronic healthcare data. Clin Pharmacol Ther. 2019;106:238–44.
De Vincentis A, Gallo P, Finamore P, et al. Potentially inappropriate medications, drug-drug interactions, and anticholinergic burden in elderly hospitalized patients: does an association exist with post-discharge health outcomes? Drugs Aging. 2020;37:585–93.
Hochheiser H, Jing X, Garcia EA, et al. A minimal information model for potential drug-drug interactions. Front Pharmacol. 2021;11:2477.
Bezin J, Noize P, Mansiaux Y, Jarne A, Pariente A. Antidopaminergic antiemetics and trauma-related hospitalization: a population-based self-controlled case series study. Br J Clin Pharmacol. 2021;87:1303–9.
Thésaurus des interactions médicamenteuses. ANSM. 2021. Available from: https://ansm.sante.fr/documents/reference/thesaurus-des-interactions-medicamenteuses-1. [Accessed 13 Dec 2022].
Bezin J, et al. The national healthcare system claims databases in France, SNIIRAM and EGB: powerful tools for pharmacoepidemiology. Pharmacoepidemiol Drug Saf. 2017;26:954–62.
Farrington P, Pugh S, Colville A, et al. A new method for active surveillance of adverse events from diphtheria/tetanus/pertussis and measles/mumps/rubella vaccines. Lancet. 1995;345:567–9.
Petersen I, Douglas I, Whitaker H. Self controlled case series methods: an alternative to standard epidemiological study designs. BMJ. 2016;354: i4515.
Rockhill B, Newman B, Weinberg C. Use and misuse of population attributable fractions. Am J Public Health. 1998;88:15–9.
Whitaker HJ, Paddy Farrington C, Spiessens B, Musonda P. Tutorial in biostatistics: the self-controlled case series method. Stat Med. 2006;25:1768–97.
Jawaro T, Bridgeman PJ, Mele J, Wei G. Descriptive study of drug-drug interactions attributed to prescriptions written upon discharge from the emergency department. Am J Emerg Med. 2019;37:924–7.
Guédon-Moreau L, Ducrocq D, Duc MF, et al. Absolute contraindications in relation to potential drug interactions in outpatient prescriptions: analysis of the first five million prescriptions in 1999. Eur J Clin Pharmacol. 2003;59:689–95.
Danielsson B, Collin J, Nyman A, et al. Drug use and torsades de pointes cardiac arrhythmias in Sweden: a nationwide register-based cohort study. BMJ Open. 2020;10: e034560.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The present study is part of the Drugs Systematized Assessment in real-liFe Environment (DRUGS-SAFE) research program that is funded in part by the French Medicines Agency (Agence Nationale de Sécurité du Médicament et des Produits de Santé, ANSM); grant number 2014s029. This program aims at creating an integrated system for the concomitant monitoring of drug use and safety in France. The potential impact of drugs, the frailty of populations, and the seriousness of risks drive the research program. The funder had no role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and the decision to submit the manuscript for publication. This publication represents the views of the authors and does not necessarily represent the opinion of the French Medicines Agency.
Conflict of interest
All authors declare research grants from the French Medicines Agency (Agence Nationale de Sécurité du Médicament et des Produits de Santé, ANSM).
Ethical approval
This study received the consent of The National Institute for Health Data.
Consent to participate
Not applicable.
Consent for publications
Not applicable.
Availability of Data and Material
Publicly sharing EGB data is forbidden by law according to the French national data protection agency (Commission Nationale de l’Informatique et des LIbertés, CNIL); regulatory decisions AT/CPZ/SVT/JB/DP/CR05222O of 14 June, 2005 and DP/CR071761 of 28 August, 2007. To request data access, please contact The National Institute for Health Data (Institut National des Données de Santé, INDS; website: http://www.indsante.fr/).
Code availability
Not applicable.
Author contributions
LL, JB, and AP contributed to the conception and design; AJ contributed to data acquisition; LL and AJ contributed to data analysis; LL, JB, AJ, and AP contributed to data interpretation; LL contributed to drafting of the article; JB, AJ, and AP critically revised the article for important intellectual content. All authors read and approved the final version of the article.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Létinier, L., Bezin, J., Jarne, A. et al. Drug–Drug Interactions and the Risk of Emergency Hospitalizations: A Nationwide Population-Based Study. Drug Saf 46, 449–456 (2023). https://doi.org/10.1007/s40264-023-01283-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40264-023-01283-7