Abstract
Background and objective
Side effects of irinotecan treatment can be dose limiting and may impair quality of life. In this study, we investigated the correlation between single nucleotide polymorphisms (SNPs) in genes encoding enzymes involved in the irinotecan metabolism and transport, outside UGT1A1, and irinotecan-related toxicity. We focused on carboxylesterases, which are involved in formation of the active metabolite SN-38 and on drug transporters.
Methods
Patients who provided written informed consent at the Erasmus Medical Center Cancer Institute to the Code Geno study (local protocol: MEC02-1002) or the IRI28-study (NTR-6612) were enrolled in the study and were genotyped for 15 SNPs in the genes CES1, CES2, SLCO1B1, ABCB1, ABCC2, and ABCG2.
Results
From 299 evaluable patients, 86 patients (28.8%) developed severe irinotecan-related toxicity. A significantly higher risk of toxicity was seen in ABCG2 c.421C>A variant allele carriers (P = 0.030, OR 1.88, 95% CI 1.06–3.34). Higher age was associated with all grade diarrhea (P = 0.041, OR 1.03, 95% CI 1.00–1.06). In addition, CES1 c.1165-41C>T and CES1 n.95346T>C variant allele carriers had a lower risk of all-grade thrombocytopenia (P = 0.024, OR 0.42, 95% CI 0.20–0.90 and P = 0.018, OR 0.23, 95% CI 0.08–0.79, respectively).
Conclusion
Our study indicates that ABCG2 and CES1 SNPs might be used as predictive markers for irinotecan-induced toxicity.
Similar content being viewed by others
Even after upfront UGT1A1 genotyping, irinotecan treatment is accompanied by severe adverse events in more than 30% of patients. |
We show that single nucleotide polymorphisms in ABCG2 and CES1 are associated with adverse events. |
These results may be used to further individualize irinotecan treatment schedules. |
1 Introduction
Irinotecan is an antineoplastic agent that remains a cornerstone treatment for gastrointestinal cancers such as advanced colorectal and pancreatic cancer [1, 2]. Despite its frequent use in clinical practice, the side effects of irinotecan can be dose limiting and may impair quality of life [2]. Most common side effects are diarrhea, febrile neutropenia, anemia, and thrombocytopenia, which occur in around a third of the patients treated with monotherapy irinotecan [3,4,5,6]. The incidence is even higher if irinotecan is given in combination with other anticancer agents such as 5-fluorouracil, leucovorin, and oxaliplatin [2].
Irinotecan, a topoisomerase I inhibitor, is a prodrug that is hydrolyzed into the active metabolite SN-38 by carboxylesterase (CES) [7]. Due to its complex metabolic pathway (Fig. 1), only 2–5% of irinotecan will eventually be converted into SN-38, mainly in the liver [7, 8]. A small part of SN-38 is converted in the peripheral blood, and subsequently transported into the liver by the organic anion transporting polypeptide 1B1 (OATP1B1) [9]. In the liver and the intestines, SN-38 is predominantly inactivated into SN-38-glucuronide (SN-38-G) by UDP-glucuronosyltransferase 1A1 (UGT1A1), and to a much lesser extent, by cytochrome P450 3A4 (CYP3A4) [10, 11]. Once biliary excreted, SN-38-G can in turn be deconjugated back into SN-38 by bacterial beta-glucuronidase in the intestine [12].
Many studies have provided insights into the risk factors for developing irinotecan-induced toxicity [2]. Much of this research has focused on pharmacogenetic causes of a higher SN-38 exposure [13], predominantly due to reduced UGT1A1 mediated SN-38 metabolism [13]. In particular, the *28 and *93 variants in UGT1A1 were studied extensively and proven to be clinically relevant in Caucasian patients and potentially suitable for genotype-guided dosing [14,15,16]. Recently, Hulshof et al. have shown that preemptive genotyping for identification of homozygous carriers of UGT1A1 *28 and/or *93, followed by a 30% dose reduction, results in significantly lower incidence of febrile neutropenia and irinotecan-related hospital admissions due to adverse events [17].
Furthermore, polymorphisms in membrane transporter genes such as ABCB1, ABCC2, and ABCG2 are associated with both irinotecan/SN-38 pharmacokinetics and irinotecan-related adverse events such as diarrhea, febrile neutropenia, anemia, and thrombocytopenia [11, 18, 19], but the results of these findings have not been prospectively validated yet.
Despite all efforts to predict and mitigate toxicity during irinotecan treatment, the incidence of severe adverse events still exceeds 30% in wild type patients for UGT1A1 polymorphisms [17]. In this study we attempted to further clarify the impact of single nucleotide polymorphisms (SNPs) in genes involved in the irinotecan metabolism or transportation on irinotecan-induced toxicity, predominantly focusing on carboxylesterases, which are involved in SN-38 formation and on drug transporters.
2 Methods
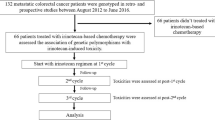
2.1 Study Design and Participants
In this single-center study conducted at Erasmus MC Cancer Institute, we enrolled patients who were treated within this center with irinotecan between July 2001 and June 2021, if they provided written informed consent in the Code Geno study (local protocol: MEC02-1002) or the IRI-28 study (NTR-6612, local protocol: MEC20-007) and if blood samples and clinical data were available. In both studies, blood samples were collected prospectively for genotyping purposes.
2.2 Single Nucleotide Polymorphism Selection
To identify potentially relevant SNPs in carboxylesterases or transporter genes involved in the metabolism of irinotecan, MEDLINE was searched for CES1, CES2, SLCO1B1, ABCB1, ABCC2, and ABCG2. All SNPs reported to be associated with irinotecan toxicity or pharmacokinetics were included if their estimated minor allele frequency (MAF) was higher than 10% in the Dutch population. To broaden the scope of this research even more, a separate literature search was conducted to identify more carboxylesterase SNPs related to other substrate drugs. Eventually, 15 SNPs in six genes involved in irinotecan metabolism or transport were selected (Table 1) [19,20,21,22,23]. As patients with a genotype homozygous for UGT1A1 *28 and/or *93 already had an initial 30% dose reduction, which resulted in significantly lower incidence of irinotecan-related toxicity, these patients were excluded from analysis [17].
2.3 Data Collection
The following demographic and clinical data were collected retrospectively; age, sex, body surface area (BSA), Eastern Cooperative Oncology Group Performance Status (ECOG-PS), tumor type, treatment regimen, dose reductions, treatment interruptions, treatment discontinuation, neutropenia, anemia, thrombocytopenia, diarrhea, nausea, and vomiting during irinotecan treatment. Data were collected until 1 month after the last administration of irinotecan. The different side effects were also analyzed as one group and defined as “overall toxicity.” Adverse events were graded according to the Common Terminology Criteria for Adverse Events version 5.0 (CTCAE) [24]. Only adverse events (AEs) which were possibly, probably, or definitely related to irinotecan treatment were classified as treatment-related AEs. CTCAE grade ≥ 3 was defined as “severe.” AE grading was primarily done by the treating physician, or if not registered in the patient file, assessed by the authors (MdW, LvD, EK). Both grade ≥ 1 and grade ≥ 3 adverse events were analyzed.
2.4 DNA Isolation and Genotyping
Ethylenediamine tetraacetic acid (EDTA) whole blood samples were collected for pharmacogenetic analysis. The DNA isolation was performed on the MagCore® SUPER DNA/RNA Extraction Instrument (Artrida, Amersfoort, The Netherlands) with the MagCore® Genomic DNA Whole Blood Kit (for genotyping, type 106). Following DNA isolation, the DNA samples were diluted to a work solution of 10 ng/µL.
Genotyping for the genes CES1 (rs2244613, rs2244614, rs3217164, rs7187684, rs3785161, rs3815583), CES2 (rs2241409), ABCC2 (rs717620, rs3740066), ABCG2 (rs2231142), ABCB1 (rs1045642, rs1128503, rs2032582), and SLCO1B1 (rs4149056, rs2306283) was performed on the TaqMan 7500 software (Applied Biosystems, Life Technologies Europe BV, Bleijswijk, the Netherlands) with a TaqMan GTXpress Mastermix (Applied Biosystems, Life Technologies Europe BV,) in combination with the specific SNP assays (Applied Biosystems, Life Technologies Europe BV). The protocol for the qPCR consists of 40 cycles of 95 °C denaturation lasting 20 s. After the denaturation step, there is an annealing of 92 °C for 3 s and then an extension step of 60 °C for 30 s.
2.5 Statistical Analysis
The distribution of the studied genotypes was tested according to Hardy–Weinberg equilibrium (HWE) using the chi-squared test. SNPs with HWE P-value below 0.05 were excluded from analysis. SNPs in the same gene were tested for linkage disequilibrium (LD) by calculating R2 using LDlink (https://ldlink.nci.nih.gov/). SNPs were considered to be in (partial) LD if R2 > 0.8; in that case, a haplotype of the SNPs was included in HWE analysis. According to the distribution of the genotypes per SNP, the most appropriate genetic model was used; additive, dominant, or recessive.
Adverse events were tested against genotypes, baseline factors (i.e., age, sex, and BSA), irinotecan dosing interval (i.e., every 2 weeks or every 3 weeks) and whether patients were treated with oxaliplatin. Dichotomized data (including the dominant and recessive model) were tested using the Fisher’s exact or the chi-squared test. Continuous data were tested using logistic regression analysis. Adverse events associated with genetic polymorphisms and baseline factors with P < 0.1 in univariable analysis were entered in multivariable logistic regression analysis (without backward selection). All statistical analyses were performed using SPSS version 28.0.1.0.
3 Results
3.1 Patients
A total of 299 patients were eligible for this analysis. Most patients were treated with irinotecan monotherapy (n = 168, 56.2%) or in combination with 5-fluorouracil and oxaliplatin (n = 115, 38.5%). Median weekly dose was 225 mg (IQR 110–300 mg) and most patients were treated in a 3-weekly schedule (n = 172, 57.5%). Patient characteristics are summarized in Table 2.
3.2 Severe Irinotecan-Related Adverse Events
In total, 86 patients (28.8%) developed severe irinotecan-related adverse events (CTCAE grade ≥ 3) during treatment. Febrile neutropenia was observed in 16 patients (5.4%), severe diarrhea in 44 patients (14.7%), severe anemia in 23 patients (7.7%), and severe thrombocytopenia in 12 patients (4.0%). A complete overview of the irinotecan-related toxicity is presented in Table 2.
3.3 Associations of SNPs with Irinotecan-Related Adverse Events
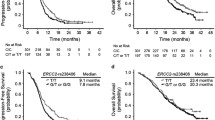
Table 1 presents MAF of the studied SNPs. Associations of toxicity with the investigated SNPs with P < 0.1 in univariable analysis are presented in Table 3. Higher risk of overall severe irinotecan-related toxicity was found in ABCG2 c.421C>A variant allele carriers (P = 0.030, OR 1.88, 95% CI 1.06–3.34) compared with non-carriers of the SNP, also after correction for other potential influencing factors in multivariable analysis. Both carriers of the ABCB1 2677TT variant and age were significantly associated with diarrhea in univariable analysis (P = 0.045 and P = 0.014, respectively). However, in a multivariable model only age remained significant associated (P = 0.041, OR 1.03, 95% CI 1.00–1.06). In multivariable analysis, CES1 c.1165-41C>T variant allele carriers and CES1 n.95346CC carriers had lower risk on thrombocytopenia, independent of the grade (P = 0.024, OR 0.42, 95% CI 0.20–0.90, and P = 0.018, OR 0.23, 95% CI 0.08–0.79, respectively).
4 Discussion
In this study, we found that SNPs in CES1 and ABCG2 were significantly associated with irinotecan-related toxicity in multivariable analysis: two different SNPs in CES1 were, independent of each other, associated with all-grade thrombocytopenia, whereas ABCG2 c.421C>A was associated with grade ≥ 3 overall toxicity. The latter association seems to be explained by significantly more frequent severe anemia and thrombocytopenia in ABCG2 c.421C>A variant carriers, but these associations could only be tested in univariable analysis due to the relatively low incidence of these adverse events.
The association between this SNP in ABCG2 and adverse events is supported by in vitro research, where a reduced protein expression and sensitivity to anticancer drugs of the mutant protein was observed [25]. Furthermore, pharmacokinetics of irinotecan and its major metabolites are not significantly different between ABCG2 c.421C>A variant carriers and wild types [22, 26]. Since ABCG2 c.421C>A has been repeatedly associated with irinotecan-related toxicity, we hypothesize that the active irinotecan metabolite SN-38 might accumulate intracellularly in organs, causing adverse reactions in carriers of the SNP without affecting systemic pharmacokinetics. Prospective validation of the association with adverse events is needed to evaluate potential clinical utilization in predicting and mitigating irinotecan-related toxicity.
Our study focused on genetic polymorphisms in carboxylesterase genes, as they are responsible for converting irinotecan into SN-38 [7]. Several associations between CES activity and irinotecan effectiveness were found [27,28,29,30], although conflicting studies have been published [31,32,33,34,35,36]. We recently found that CES1 polymorphisms are associated with adverse events due to another carboxylesterase substrate, the 5-FU prodrug capecitabine [37]. This was also found by Hamzic et al. and Laizure et al. [20, 23] indicating the potential role of CES polymorphisms in the development of irinotecan-related toxicity. In patients treated with irinotecan, however, we found that two CES1 germline polymorphisms, that is, CES1 c.1165-41C>T and CES1 n.95346T>C, had a significant inverse association with “any grade” thrombocytopenia. Interestingly, these SNPs markedly differ from those associated with severe thrombocytopenia (ABCC2 3792C>T and ABCG2 c.421C>A). Although this seems contradictory, low-grade thrombocytopenia might be a sign of cumulative myelosuppression in patients who are treated for a prolonged period, that is, those that tolerate irinotecan well, whereas high-grade thrombocytopenia represents a more acute and severe mechanism of action. The inverse association of CES1 SNPs with any grade thrombocytopenia might therefore illustrate that these variant carriers form SN-38 at a lower rate than wild type patients for this gene and that they are able to better tolerate irinotecan. Prospective validation of this theory is also warranted, especially in combination with pharmacokinetic research.
In addition to the ABCG2 SNP, we also investigated other SNPs in genes encoding for other ABC transporters. Irinotecan and SN-38 are both substrates of a spectrum of ABC transporters (Fig. 1), and polymorphisms in their encoding genes could potentially affect the incidence of irinotecan-related toxicity. For ABCB1 c.3435C>T, for example, an association with toxicity was previously shown [38,39,40,41,42], whereas several other studies could not confirm this association [19, 43,44,45]. Moreover, this SNP has been associated with lower irinotecan exposure [38, 40], which potentially explains the lack of an association between ABCB1 c.3435C>T and irinotecan-related toxicity in this study. For ABCB1 1236C>T previous studies were also conflicting, reporting either an association with higher exposure and higher incidence of irinotecan-related toxicity [19, 41, 46], with lower risk of toxicity [43], or with no association at all [43, 44].
Furthermore, SNPs in ABCC2 were significantly associated with severe anemia and thrombocytopenia, but the small number of events for these endpoints stopped us from performing multivariable analyses on these endpoints. Previous studies showed higher irinotecan exposure but a lower risk on grade 3 or 4 neutropenia in ABCC2 c.-24T>C carriers [47], a higher irinotecan and SN-38 exposure and higher risk on irinotecan-related adverse events in ABCC2 3972C>T carriers [18, 40, 44, 48], while haplotype analysis of this SNP showed a decreased incidence of diarrhea [49]. The dosing interval of irinotecan was significantly and strongly associated with many of the toxicity endpoints. Although one would expect the lower peak concentrations of irinotecan in a twice-weekly schedule to lead to fewer adverse events than in a thrice-weekly dosing schedule, we found that toxicity was significantly higher with the shorter intervals in univariable analysis. We believe this predominantly reflects the incorporation of oxaliplatin in many of the twice-weekly schedules, as the odds ratios of oxaliplatin-containing regimens versus others were even more extreme than those of the twice-weekly versus thrice-weekly schedules (data not shown). Likewise, fluoropyrimidines might have contributed to the incidence of diarrhea. Another significantly associated clinical parameter was age in the case of diarrhea. Although the median age in this study is relatively low (61 years, IQR 55–67), it is already known that the incidence of severe chemotherapy-related toxicity in elderly patients (65 years or older) is 64% [50]. Geriatric assessments before start with irinotecan treatment can rule out patients not suitable for irinotecan-containing treatment [51], although the value of geriatric treatment in predicting toxicity remains unclear [50]. For severe diarrhea, neither an association with a SNP or baseline factor was found.
A limitation of this study is its retrospective character, which hampered us in studying low-grade adverse events and concomitant medication, querying ambiguities in the older patient files, and adjusting for changes in treatment regimens over time. Our main endpoint, CTCAE grade 3 or higher adverse events, had a lower incidence than we had expected from the literature. The incidence of anemia grade ≥ 3, for example, was too low in variant allele carriers to test the association multivariable. In addition, ABCG2 c.421C>A carriers have potentially also increased risk on specific adverse events, but the low incidence of specific severe adverse events means that this does not emerge from our analysis. Furthermore, the different treatment regimens might have biased some of the outcomes, but we have countered this by incorporation of the regimens in our multivariable analyses. Additionally, it should be noted that we excluded carriers of UGT1A1*28 and *93, which allowed us to better study the investigated SNPs, but might have led to different results than in previous studies in an unselected population. The relation between the UGT1A1 SNPs and the ABCG2 SNP with toxicity could be investigated in future research.
Overall, pharmacogenetic testing is a low-invasive way to identify patients at high risk for treatment-related toxicity. Previous studies have already shown that patients prone to developing severe adverse events can be identified by pharmacogenetic testing, and that dose reductions in these patients reduce the incidence of treatment-related adverse events in a cost-effective manner [17, 52]. Therefore, it is important to continue searching for novel candidate polymorphisms that could serve as predictive biomarkers, which in general is done in retrospective studies. As for this study, these results need to be validated in larger and preferably prospective studies, as the retrospective and explorative character of these studies and the lack of correction for multiple testing might lead to false positive findings. In general, pharmacogenetic testing could not only improve patient safety during irinotecan treatment, but also reduce treatment-related costs.
5 Conclusion
In this study, we found that ABCG2 c.421C>A variant allele carriers are at higher risk of severe irinotecan-related overall toxicity. In addition, CES1 c.1165-41C>T and CES1 n.95346T>C variant allele carriers had a reduced risk of all-grade thrombocytopenia. Despite the contradictory results from other retrospective cohorts, our study indicates that ABCG2 and CES1 SNPs might be used as predictive markers for irinotecan-induced toxicity. Prospective studies addressing both adverse events and pharmacokinetics in patients treated with irinotecan are needed to validate the pharmacogenetic biomarkers found in our study for irinotecan-induced toxicity other than UGT1A1 *28 and *93.
References
Geneesmiddelenbank. Summary of product characteristics (SmPC) irinotecan HCL-trihydraat accord 20mg/ml 23/12/2021.
de Man FM, Goey AKL, van Schaik RHN, Mathijssen RHJ, Bins S. Individualization of irinotecan treatment: a review of pharmacokinetics, pharmacodynamics, and pharmacogenetics. Clin Pharmacokinet. 2018;57(10):1229–54.
Cunningham D, Pyrhönen S, James RD, Punt CJ, Hickish TF, Heikkila R, et al. Randomised trial of irinotecan plus supportive care versus supportive care alone after fluorouracil failure for patients with metastatic colorectal cancer. Lancet. 1998;352(9138):1413–8.
Sobrero AF, Maurel J, Fehrenbacher L, Scheithauer W, Abubakr YA, Lutz MP, et al. EPIC: phase III trial of cetuximab plus irinotecan after fluoropyrimidine and oxaliplatin failure in patients with metastatic colorectal cancer. J Clin Oncol. 2008;26(14):2311–9.
Rougier P, Van Cutsem E, Bajetta E, Niederle N, Possinger K, Labianca R, et al. Randomised trial of irinotecan versus fluorouracil by continuous infusion after fluorouracil failure in patients with metastatic colorectal cancer. Lancet. 1998;352(9138):1407–12.
Saltz LB, Cox JV, Blanke C, Rosen LS, Fehrenbacher L, Moore MJ, et al. Irinotecan plus fluorouracil and leucovorin for metastatic colorectal cancer. Irinotecan Study Group. N Engl J Med. 2000;343(13):905–14.
Slatter JG, Su P, Sams JP, Schaaf LJ, Wienkers LC. Bioactivation of the anticancer agent CPT-11 to SN-38 by human hepatic microsomal carboxylesterases and the in vitro assessment of potential drug interactions. Drug Metab Dispos. 1997;25(10):1157–64.
Chabot GG, Abigerges D, Catimel G, Culine S, de Forni M, Extra JM, et al. Population pharmacokinetics and pharmacodynamics of irinotecan (CPT-11) and active metabolite SN-38 during phase I trials. Ann Oncol. 1995;6(2):141–51.
Nozawa T, Minami H, Sugiura S, Tsuji A, Tamai I. Role of organic anion transporter OATP1B1 (OATP-C) in hepatic uptake of irinotecan and its active metabolite, 7-ethyl-10-hydroxycamptothecin: in vitro evidence and effect of single nucleotide polymorphisms. Drug Metab Dispos. 2005;33(3):434–9.
Whirl-Carrillo M, McDonagh EM, Hebert JM, Gong L, Sangkuhl K, Thorn CF, et al. Pharmacogenomics knowledge for personalized medicine. Clin Pharmacol Ther. 2012;92(4):414–7.
Riera P, Páez D. Elucidating the role of pharmacogenetics in irinotecan efficacy and adverse events in metastatic colorectal cancer patients. Expert Opin Drug Metab Toxicol. 2021;17(10):1157–63.
Rivory LP, Robert J. Identification and kinetics of a beta-glucuronide metabolite of SN-38 in human plasma after administration of the camptothecin derivative irinotecan. Cancer Chemother Pharmacol. 1995;36(2):176–9.
Li M, Seiser EL, Baldwin RM, Ramirez J, Ratain MJ, Innocenti F, et al. ABC transporter polymorphisms are associated with irinotecan pharmacokinetics and neutropenia. Pharmacogenomics J. 2018;18(1):35–42.
Mathijssen RH, Gurney H. Irinogenetics: how many stars are there in the sky? J Clin Oncol. 2009;27(16):2578–9.
Innocenti F, Schilsky RL, Ramírez J, Janisch L, Undevia S, House LK, et al. Dose-finding and pharmacokinetic study to optimize the dosing of irinotecan according to the UGT1A1 genotype of patients with cancer. J Clin Oncol. 2014;32(22):2328–34.
Toffoli G, Cecchin E, Gasparini G, D’Andrea M, Azzarello G, Basso U, et al. Genotype-driven phase I study of irinotecan administered in combination with fluorouracil/leucovorin in patients with metastatic colorectal cancer. J Clin Oncol. 2010;28(5):866–71.
Hulshof EC, de With M, de Man FM, Creemers GJ, Deiman B, Swen JJ, et al. UGT1A1 genotype-guided dosing of irinotecan: a prospective safety and cost analysis in poor metaboliser patients. Eur J Cancer. 2022;162:148–57.
Innocenti F, Kroetz DL, Schuetz E, Dolan ME, Ramírez J, Relling M, et al. Comprehensive pharmacogenetic analysis of irinotecan neutropenia and pharmacokinetics. J Clin Oncol. 2009;27(16):2604–14.
Mathijssen RH, Marsh S, Karlsson MO, Xie R, Baker SD, Verweij J, et al. Irinotecan pathway genotype analysis to predict pharmacokinetics. Clin Cancer Res. 2003;9(9):3246–53.
Hamzic S, Kummer D, Milesi S, Mueller D, Joerger M, Aebi S, et al. Novel genetic variants in carboxylesterase 1 predict severe early-onset capecitabine-related toxicity. Clin Pharmacol Ther. 2017;102(5):796–804.
Han JY, Lim HS, Yoo YK, Shin ES, Park YH, Lee SY, et al. Associations of ABCB1, ABCC2, and ABCG2 polymorphisms with irinotecan-pharmacokinetics and clinical outcome in patients with advanced non-small cell lung cancer. Cancer. 2007;110(1):138–47.
Jada SR, Lim R, Wong CI, Shu X, Lee SC, Zhou Q, et al. Role of UGT1A1*6, UGT1A1*28 and ABCG2 c.421C>A polymorphisms in irinotecan-induced neutropenia in Asian cancer patients. Cancer Sci. 2007;98(9):1461–7.
Laizure SC, Parker RB. Is genetic variability in carboxylesterase-1 and carboxylesterase-2 drug metabolism an important component of personalized medicine? Xenobiotica. 2020;50(1):92–100.
U.S. Department of Health and Human Services. Common terminology criteria for adverse events (CTCAE) Version 5.0; 2017 November 27, 2017.
Imai Y, Nakane M, Kage K, Tsukahara S, Ishikawa E, Tsuruo T, et al. C421A polymorphism in the human breast cancer resistance protein gene is associated with low expression of Q141K protein and low-level drug resistance. Mol Cancer Ther. 2002;1(8):611–6.
de Jong FA, Marsh S, Mathijssen RH, King C, Verweij J, Sparreboom A, et al. ABCG2 pharmacogenetics: ethnic differences in allele frequency and assessment of influence on irinotecan disposition. Clin Cancer Res. 2004;10(17):5889–94.
Basel MT, Balivada S, Shrestha TB, Seo GM, Pyle MM, Tamura M, et al. A cell-delivered and cell-activated SN38-dextran prodrug increases survival in a murine disseminated pancreatic cancer model. Small. 2012;8(6):913–20.
Choi SS, Yoon K, Choi SA, Yoon SB, Kim SU, Lee HJ. Tumor-specific gene therapy for pancreatic cancer using human neural stem cells encoding carboxylesterase. Oncotarget. 2016;7(46):75319–27.
Oosterhoff D, Overmeer RM, de Graaf M, van der Meulen IH, Giaccone G, van Beusechem VW, et al. Adenoviral vector-mediated expression of a gene encoding secreted, EpCAM-targeted carboxylesterase-2 sensitises colon cancer spheroids to CPT-11. Br J Cancer. 2005;92(5):882–7.
Uchino J, Takayama K, Harada A, Sone T, Harada T, Curiel DT, et al. Tumor targeting carboxylesterase fused with anti-CEA scFv improve the anticancer effect with a less toxic dose of irinotecan. Cancer Gene Ther. 2008;15(2):94–100.
Guichard S, Terret C, Hennebelle I, Lochon I, Chevreau P, Frétigny E, et al. CPT-11 converting carboxylesterase and topoisomerase activities in tumour and normal colon and liver tissues. Br J Cancer. 1999;80(3–4):364–70.
Hsieh YT, Lin HP, Chen BM, Huang PT, Roffler SR. Effect of Cellular Location of human carboxylesterase 2 on CPT-11 hydrolysis and anticancer activity. PLoS ONE. 2015;10(10): e0141088.
Kawato Y, Furuta T, Aonuma M, Yasuoka M, Yokokura T, Matsumoto K. Antitumor activity of a camptothecin derivative, CPT-11, against human tumor xenografts in nude mice. Cancer Chemother Pharmacol. 1991;28(3):192–8.
Ohtsuka K, Inoue S, Kameyama M, Kanetoshi A, Fujimoto T, Takaoka K, et al. Intracellular conversion of irinotecan to its active form, SN-38, by native carboxylesterase in human non-small cell lung cancer. Lung Cancer. 2003;41(2):187–98.
van Ark-Otte J, Kedde MA, van der Vijgh WJ, Dingemans AM, Jansen WJ, Pinedo HM, et al. Determinants of CPT-11 and SN-38 activities in human lung cancer cells. Br J Cancer. 1998;77(12):2171–6.
Xu G, Zhang W, Ma MK, McLeod HL. Human carboxylesterase 2 is commonly expressed in tumor tissue and is correlated with activation of irinotecan. Clin Cancer Res. 2002;8(8):2605–11.
de With M, van Doorn L, Maasland DC, Mulder TAM, Oomen-de Hoop E, Mostert B, et al. Capecitabine-induced hand-foot syndrome: a pharmacogenetic study beyond DPYD. Biomed Pharmacother. 2023;9(159): 114232.
Teft WA, Welch S, Lenehan J, Parfitt J, Choi YH, Winquist E, et al. OATP1B1 and tumour OATP1B3 modulate exposure, toxicity, and survival after irinotecan-based chemotherapy. Br J Cancer. 2015;112(5):857–65.
Lévi F, Karaboué A, Saffroy R, Desterke C, Boige V, Smith D, et al. Pharmacogenetic determinants of outcomes on triplet hepatic artery infusion and intravenous cetuximab for liver metastases from colorectal cancer (European trial OPTILIV, NCT00852228). Br J Cancer. 2017;117(7):965–73.
Han JY, Lim HS, Park YH, Lee SY, Lee JS. Integrated pharmacogenetic prediction of irinotecan pharmacokinetics and toxicity in patients with advanced non-small cell lung cancer. Lung Cancer. 2009;63(1):115–20.
Salvador-Martín S, García-González X, García MI, Blanco C, García-Alfonso P, Robles L, et al. Clinical utility of ABCB1 genotyping for preventing toxicity in treatment with irinotecan. Pharmacol Res. 2018;136:133–9.
Glimelius B, Garmo H, Berglund A, Fredriksson LA, Berglund M, Kohnke H, et al. Prediction of irinotecan and 5-fluorouracil toxicity and response in patients with advanced colorectal cancer. Pharmacogenomics J. 2011;11(1):61–71.
Cortejoso L, López-Fernández LA. Pharmacogenetic markers of toxicity for chemotherapy in colorectal cancer patients. Pharmacogenomics. 2012;13(10):1173–91.
Atasilp C, Chansriwong P, Sirachainan E, Reungwetwattana T, Sirilerttrakul S, Chamnanphon M, et al. Effect of drug metabolizing enzymes and transporters in Thai colorectal cancer patients treated with irinotecan-based chemotherapy. Sci Rep. 2020;10(1):13486.
Côté JF, Kirzin S, Kramar A, Mosnier JF, Diebold MD, Soubeyran I, et al. UGT1A1 polymorphism can predict hematologic toxicity in patients treated with irinotecan. Clin Cancer Res. 2007;13(11):3269–75.
Riera P, Artigas-Baleri A, Salazar J, Sebio A, Virgili AC, Arranz MJ, et al. ABCB1 Genetic variants as predictors of irinotecan-induced severe gastrointestinal toxicity in metastatic colorectal cancer patients. Front Pharmacol. 2020;11:973.
Crona DJ, Ramirez J, Qiao W, de Graan AJ, Ratain MJ, van Schaik RH, et al. Clinical validity of new genetic biomarkers of irinotecan neutropenia: an independent replication study. Pharmacogenomics J. 2016;16(1):54–9.
Zaïr ZM, Singer DR. Efflux transporter variants as predictors of drug toxicity in lung cancer patients: systematic review and meta-analysis. Pharmacogenomics. 2016;17(9):1089–112.
de Jong FA, Scott-Horton TJ, Kroetz DL, McLeod HL, Friberg LE, Mathijssen RH, et al. Irinotecan-induced diarrhea: functional significance of the polymorphic ABCC2 transporter protein. Clin Pharmacol Ther. 2007;81(1):42–9.
Versteeg KS, Konings IR, Lagaay AM, van de Loosdrecht AA, Verheul HMW. Prediction of treatment-related toxicity and outcome with geriatric assessment in elderly patients with solid malignancies treated with chemotherapy: a systematic review. Ann Oncol. 2014;25(10):1914–8.
Sastre J, Puente J, García-Saenz JA, Díaz-Rubio E. Irinotecan in the treatment of elderly patients with advanced colorectal cancer. Crit Rev Oncol Hematol. 2008;68(3):250–5.
Henricks LM, Lunenburg C, de Man FM, Meulendijks D, Frederix GWJ, Kienhuis E, et al. A cost analysis of upfront DPYD genotype-guided dose individualisation in fluoropyrimidine-based anticancer therapy. Eur J Cancer. 2019;107:60–7.
Acknowledgements
We want to thank Prof. H.M.W. Verheul from Erasmus Medical Center Cancer Institute for critically reviewing the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of interest
The authors declare no financial or non-financial conflicts of interest.
Funding
No funding was received.
Trial registration:
Part of the included patients were selected on the basis of their inclusion in the IRI-28 study; trial registration NTR-6612.
Ethics approval of the study:
The study was approved by the institutional research ethics committee of the Erasmus Medical Center (local protocol: MEC02-1002 and MEC20-007) and was conducted in accordance with good clinical practice guidelines and the current version of the Declaration of Helsinki.
Author contributions:
Conceptualization: MdW, LvD, MM, EO, RvS, RM, and SB. Formal analysis and investigation: MdW, LvD, EK, AvV, MdN, and EO. Writing – original draft preparation: MdW and SB. All authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Consent to Participate
Written informed consent was obtained from every study subject prior to inclusion into the study.
Consent for Publication
All subjects signed the informed consent.
Code availability
Not applicable.
Availability of Data and Material
The datasets generated during and/or analyzed during the current study are available from the corresponding author on reasonable request.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
de With, M., van Doorn, L., Kloet, E. et al. Irinotecan-Induced Toxicity: A Pharmacogenetic Study Beyond UGT1A1. Clin Pharmacokinet 62, 1589–1597 (2023). https://doi.org/10.1007/s40262-023-01279-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40262-023-01279-7