Abstract
The debilitating neuromuscular disorders Duchenne muscular dystrophy (DMD) and spinal muscular atrophy (SMA), which harm 1 in 5000 newborn males and 1 in 11,000 newborns, respectively, are marked by progressive muscle wasting among other complications. While DMD causes generalized muscle weakness due to the absence of the dystrophin protein, SMA patients generally face motor neuron degeneration because of the lack of the survival motor neuron (SMN) protein. Many of the most promising therapies for both conditions restore the absent proteins dystrophin and SMN. Antisense oligonucleotide-mediated exon skipping and inclusion therapies are advancing clinically with the approved DMD therapies casimersen, eteplirsen, golodirsen, and viltolarsen, and the SMA therapy nusinersen. Existing antisense therapies focus on skeletal muscle for DMD and motor neurons for SMA, respectively. Through innovative techniques, such as peptide conjugation and multi-exon skipping, these therapies could be optimized for efficacy and applicability. By contrast, gene replacement therapy is administered only once to patients during treatment. Currently, only onasemnogene abeparvovec for SMA has been approved. Safety shortcomings remain a major challenge for gene therapy. Nevertheless, gene therapy for DMD has strong potential to restore dystrophin expression in patients. In light of promising functional improvements, antisense and gene therapies stand poised to elevate the lives of patients with DMD and SMA.
Similar content being viewed by others
References
Bizot F, Vulin A, Goyenvalle A. Current status of antisense oligonucleotide-based therapy in neuromuscular disorders. Drugs. 2020;80(14):1397–415. https://doi.org/10.1007/s40265-020-01363-3.
Li D, Mastaglia FL, Fletcher S, Wilton SD. Precision medicine through antisense oligonucleotide-mediated exon skipping. Trends Pharmacol Sci. 2018;39(11):982–94.
Duchenne DR. The Pathology of paralysis with muscular degeneration (paralysie myosclerotique), or paralysis with apparent hypertrophy. Br Med J. 1867;2:541–2.
Moat SJ, Bradley DM, Salmon R, Clarke A, Hartley L. Newborn bloodspot screening for Duchenne muscular dystrophy: 21 years experience in Wales (UK). Eur J Hum Genet. 2013;21(10):1049–53.
Worton RG. Duchenne muscular dystrophy: gene and gene product; mechanism of mutation in the gene. J Inherit Metab Dis. 1992;15(4):539–50.
Dubowitz V. The Duchenne dystrophy story: from phenotype to gene and potential treatment. J Child Neurol. 1989;4(4):240–50. https://doi.org/10.1177/088307388900400402.
Aartsma-Rus A, Van Deutekom JCT, Fokkema IF, Van Ommen GJB, Den Dunnen JT. Entries in the Leiden Duchenne muscular dystrophy mutation database: an overview of mutation types and paradoxical cases that confirm the reading-frame rule. Muscle Nerve. 2006;34(2):135–44.
Koenig M, Beggs AH, Moyer M, Scherpf S, Heindrich K, Bettecken T, et al. The molecular basis for Duchenne versus becker muscular dystrophy: correlation of severity with type of deletion. Am J Hum Genet. 1989;45(4):498–506.
Rahimov F, Kunkel LM. The cell biology of disease: cellular and molecular mechanisms underlying muscular dystrophy. J Cell Biol. 2013;201(4):499–510.
Le S, Yu M, Hovan L, Zhao Z, Ervasti J, Yan J. Dystrophin as a molecular shock absorber. ACS Nano. 2018;12(12):12140–8.
Gumerson JD, Michele DE. The dystrophin-glycoprotein complex in the prevention of muscle damage. J Biomed Biotechnol. 2011;2011:210797.
Hoffman EP, Brown RH, Kunkel LM. Dystrophin: the protein product of the Duchene muscular dystrophy locus. Biotechnology. 1987;51(6):919–28.
Klingler W, Jurkat-rott K, Lehmann-horn F, Schleip R. The role of fibrosis in Duchenne muscular dystrophy. Acta Myol. 2012;31:184–95.
D’Angelo MG, Berti M, Piccinini L, Romei M, Guglieri M, Bonato S, et al. Gait pattern in Duchenne muscular dystrophy. Gait Posture. 2009;29:36–41.
Thomas SS, Buckon CE, Nicorici A, Bagley A, Mcdonald CM, Sussman MD. Classification of the gait patterns of boys with Duchenne muscular dystrophy and their relationship to function. J Child Neurol. 2013;25(9):1103–9.
Korinthenberg R. A new era in the management of Duchenne muscular dystrophy. Dev Med Child Neurol. 2019;61(3):292–7.
Feingold B, Mahle WT, Auerbach S, Clemens P, Domenighetti AA, Jefferies JL, et al. Management of cardiac involvement associated with neuromuscular diseases: a scientific statement from the American Heart Association. Circulation. 2017;136(13):e200–31.
Buddhe S, Cripe L, Friedland-Little J, Kertesz N, Eghtesady P, Finder J, et al. Cardiac management of the patient with Duchenne muscular dystrophy. Pediatrics. 2018;2018(142):S72-81.
Werneck LC, Lorenzoni PJ, Ducci RD-P, Fustes OH, Kay CSK, Scola RH. Duchenne muscular dystrophy: an historical treatment review. Arq Neuropsiquiatr. 2019;77(8):579–89.
Asher DR, Thapa K, Dharia SD, Khan N, Potter RA, Rodino-Klapac LR, et al. Clinical development on the frontier: gene therapy for duchenne muscular dystrophy. Expert Opin Biol Ther. 2020;20(3):263–74. https://doi.org/10.1080/14712598.2020.1725469.
Hoffman EP. Pharmacotherapy of Duchenne muscular dystrophy. In: Handbook of experimental pharmacology. Binghamton: Binghamton University State University of New York; 2019.
Bladen CL, Salgado D, Monges S, Foncuberta ME, Kekou K, Kosma K, et al. The TREAT-NMD DMD global database: analysis of more than 7,000 duchenne muscular dystrophy mutations. Hum Mutat. 2015;36(4):395–402.
Kole R, Krieg AM. Exon skipping therapy for Duchenne muscular dystrophy. Adv Drug Deliv Rev. 2015;87:104–7.
Aoki Y, Nakamura A, Yokota T, Saito T, Okazawa H, Nagata T, et al. In-frame dystrophin following exon 51-skipping improves muscle pathology and function in the exon 52-deficient mdx mouse. Mol Ther. 2010;18(11):1995–2005.
Wein N, Vulin A, Findlay AR, Gumienny F, Huang N, Wilton SD, et al. Efficient skipping of single exon duplications in DMD patient-derived cell lines using an antisense oligonucleotide approach. J Neuromuscul Dis. 2017;4(3):199–207.
Yokota T, Lu QL, Partridge T, Kobayashi M, Nakamura A, Takeda S, et al. Efficacy of systemic morpholino exon-skipping in duchenne dystrophy dogs. Ann Neurol. 2009;65(6):667–76.
Qi LL, Rabinowitz A, Yun CC, Yokota T, Yin HF, Alter J, et al. Systemic delivery of antisense oligoribonucleotide restorers dystrophin expression in body-wide skeletal muscles. Proc Natl Acad Sci USA. 2005;102(1):198–203.
Dunckley MG, Manoharan M, Villiet P, Eperon IC, Dickson G. Modification of splicing in the dystrophin gene in cultured mdx muscle cells by antisense oligoribonucleotides. Hum Mol Genet. 1998;5(1):1083–90.
Aartsma-Rus A, Ferlini A, Goemans N, Pasmooij AMG, Wells DJ, Bushby K, et al. Translational and regulatory challenges for exon skipping therapies. Hum Gene Ther. 2014;25(10):885–92.
Bello L, Campadello P, Barp A, Fanin M, Semplicini C, Sorarù G, et al. Functional changes in Becker muscular dystrophy: implications for clinical trials in dystrophinopathies. Sci Rep. 2016;6:1–12.
Aartsma-Rus A, Straub V, Hemmings R, Haas M, Schlosser-Weber G, Stoyanova-Beninska V, et al. Development of exon skipping therapies for duchenne muscular dystrophy: a critical review and a perspective on the outstanding issues. Nucleic Acid Ther. 2017;27(5):251–9.
Kesselheim AS, Avorn J. Approving a problematic muscular dystrophy drug: implications for FDA policy. J Am Med Assoc. 2016;316(22):2357–8.
Aartsma-Rus A, Goemans N. A sequel to the Eteplirsen Saga: eteplirsen is approved in the united states but was not approved in Europe. Nucleic Acid Ther. 2019;29(1):13–5.
Zingariello CD, Kang PB. Dollars and antisense for Duchenne muscular dystrophy. Neurology. 2018;90(24):1091–2.
Dalakas MC. Gene therapy for Duchenne muscular dystrophy: balancing good science, marginal efficacy, high emotions and excessive cost. Ther Adv Neurol Disord. 2017;10:293–6.
Randeree L, Eslick GD. Eteplirsen for paediatric patients with Duchenne muscular dystrophy: a pooled-analysis. J Clin Neurosci. 2018;49:1–6. https://doi.org/10.1016/j.jocn.2017.10.082.
Echigoya Y, Lim KRQ, Trieu N, Bao B, Nichols BM, Vila MC, et al. Quantitative antisense screening and optimization for exon 51 skipping in duchenne muscular dystrophy. Mol Ther. 2017;25(11):2561–72. https://doi.org/10.1016/j.ymthe.2017.07.014.
Nguyen Q, Yokota T. Immortalized muscle cell model to test the exon skipping efficacy for duchenne muscular dystrophy. J Pers Med. 2017;7(4):13.
Aupy P, Echevarría L, Relizani K, Zarrouki F, Haeberli A, Komisarski M, et al. Identifying and avoiding tcDNA-ASO sequence-specific toxicity for the development of DMD Exon 51 skipping therapy. Mol Ther Nucleic Acids. 2020;19:371–83. https://doi.org/10.1016/j.omtn.2019.11.020.
Shimizu-Motohashi Y, Komaki H, Motohashi N, Takeda S, Yokota T, Aoki Y. Restoring dystrophin expression in duchenne muscular dystrophy: current status of therapeutic approaches. J Pers Med. 2019;9(1):1–14.
Heo Y-A. Golodirsen: first approval. Drugs. 2020;80(3):329–33.
Muntoni F, Frank DE, Morgan J, Domingos J, Schnell FJ, Dickson G, et al. Golodirsen induces exon skipping leading to sarcolemmal dystrophin expression in patients with genetic mutations amenable to exon 53 skipping. Neuromuscul Disord. 2018;28:S5. https://doi.org/10.1016/S0960-8966(18)30304-3.
Lundin KE, Gissberg O, Smith CIE, Zain R. Chemical development of therapeutic oligonucleotides. Methods Mol Biol. 2019;2036:3–16.
US FDA. Amondys 45 (casimersen) injection, for intravenous use: US prescribing information. 2021. https://www.accessdata.fda.gov/drugsatfda_docs/label/2021/213026lbl.pdf. Accessed 12 May 2021
Roshmi RR, Yokota T. Viltolarsen for the treatment of Duchenne muscular dystrophy. Drugs Today (Barc). 2019;55(10):627–39.
Hwang J, Yokota T. Recent advancements in exon-skipping therapies using antisense oligonucleotides and genome editing for the treatment of various muscular dystrophies. Expert Rev Mol Med. 2019;21:e5.
Watanabe N, Nagata T, Satou Y, Masuda S, Saito T, Kitagawa H, et al. NS-065/NCNP-01: an antisense oligonucleotide for potential treatment of exon 53 skipping in duchenne muscular dystrophy. Mol Ther Nucleic Acids. 2018;13:442–9. https://doi.org/10.1016/j.omtn.2018.09.017.
Komaki H, Nagata T, Saito T, Masuda S, Takeshita E, Sasaki M, et al. Systemic administration of the antisense oligonucleotide NS-065/NCNP-01 for skipping of exon 53 in patients with Duchenne muscular dystrophy. Sci Transl Med. 2018;10(437):eaan0713.
Komaki H, Takeshima Y, Matsumura T, Ozasa S, Funato M, Takeshita E, et al. Viltolarsen in Japanese Duchenne muscular dystrophy patients: a phase 1/2 study. Ann Clin Transl Neurol. 2020;7:2393–408.
Clemens PR, Rao VK, Connolly AM, Harper AD, Mah JK, Smith EC, et al. Safety, tolerability, and efficacy of viltolarsen in boys with duchenne muscular dystrophy amenable to exon 53 skipping: a phase 2 randomized clinical trial. JAMA Neurol. 2020;15261:1–10.
NS Pharma’s VILTEPSOTM (viltolarsen) injection Now FDA-Approved in the US for the treatment of Duchenne muscular dystrophy in patients amenable to exon 53 skipping therapy. https://www.prnewswire.com/news-releases/ns-pharmas-viltepso-viltolarsen-injection-now-fda-approved-in-the-us-for-the-treatment-of-duchenne-muscular-dystrophy-in-patients-amenable-to-exon-53-skipping-therapy-301111298.html. Accessed 19 Dec 2020
Jearawiriyapaisarn N, Moulton HM, Buckley B, Roberts J, Sazani P, Fucharoen S, et al. Sustained dystrophin expression induced by peptide-conjugated morpholino oligomers in the muscles of mdx mice. Mol Ther. 2008;16(9):1624–9. https://doi.org/10.1038/mt.2008.120.
Wu B, Moulton HM, Iversen PL, Jiang J, Li J, Li J, et al. Effective rescue of dystrophin improves cardiac function in dystrophin-deficient mice by a modified morpholino oligomer. Proc Natl Acad Sci USA. 2008;105(39):14814–9.
Echigoya Y, Nakamura A, Nagata T, Urasawa N, Lim KRQ, Trieu N, et al. Effects of systemic multiexon skipping with peptide-conjugated morpholinos in the heart of a dog model of Duchenne muscular dystrophy. Proc Natl Acad Sci. 2017;114(16):4213–8. https://doi.org/10.1073/pnas.1613203114.
Duan D, Systemic AAV. Micro-dystrophin gene therapy for duchenne muscular dystrophy. Mol Ther. 2018;26(10):2337–56.
Le Guiner C, Servais L, Montus M, Larcher T, Fraysse B, Moullec S, et al. Long-term microdystrophin gene therapy is effective in a canine model of Duchenne muscular dystrophy. Nat Commun. 2017;8:16105.
Mendell JR, Sahenk Z, Lehman K, Nease C, Lowes LP, Miller NF, et al. Assessment of systemic delivery of rAAVrh74.MHCK7.micro-dystrophin in children with duchenne muscular dystrophy: a nonrandomized controlled trial. JAMA Neurol. 2020;77(9):1122–31.
Solid Biosciences Provides SGT-001 Program Update. 2019. https://www.solidbio.com/about/media/press-releases/solid-biosciences-provides-sgt-001-program-update. Accessed 27 Mar 2020
Solid biosciences announces FDA lifts clinical hold on IGNITE DMD Clinical Trial. 2020. https://www.solidbio.com/about/media/press-releases/solid-biosciences-announces-fda-lifts-clinical-hold-on-ignite-dmd-clinical-trial. Accessed 18 Dec 2020
Elverman M, Goddard MA, Mack D, Snyder JM, Lawlor MW, Meng H, et al. Long-term effects of systemic gene therapy in a canine model of myotubular myopathy. Muscle Nerve. 2017;56(5):943–53.
Audentes therapeutics provides update on the ASPIRO clinical trial evaluating AT132 in patients with X-linked myotubular myopathy. 2020. https://myotubulartrust.org/a-third-patient-tragically-dies-after-dosing-in-aspiro-at132-gene-therapy-trial/. Accesed 6 Dec 2020
Shieh PB, Bönnemann CG, Müller-Felber W, Blaschek A, Dowling JJ, Kuntz NL, et al. Re: “Moving forward after two deaths in a gene therapy trial of myotubular myopathy” by Wilson and Flotte. Hum Gene Ther. 2020;31(15–16):787.
Amburgey K, Tsuchiya E, De Chastonay S, Glueck M, Alverez R, Nguyen CT, et al. A natural history study of X-linked myotubular myopathy. Neurology. 2017;89(13):1355–64.
Pfizer’s New Phase 1b results of gene therapy in ambulatory boys with duchenne muscular dystrophy (DMD) support advancement into pivotal phase 3 study. 2020. https://investors.pfizer.com/investor-news/press-release-details/2020/Pfizers-New-Phase-1b-Results-of-Gene-Therapy-in-Ambulatory-Boys-with-Duchenne-Muscular-Dystrophy-DMD-Support-Advancement-into-Pivotal-Phase-3-Study/default.aspx. Accessed 6 Dec 2020
Lefebvre S, Bürglen L, Reboullet S, Clermont O, Burlet P, Viollet L, et al. Identification and characterization of a spinal muscular atrophy-determining gene. Cell. 1995;80(1):155–65.
Lefebvre S, Burlet P, Liu Q, Bertrandy S, Clermont O, Munnich A, et al. Correlation between severity and SMN protein level in spinal muscular atrophy. Nat Genet. 1997;16(3):265–9. https://doi.org/10.1038/ng0797-265.
Sugarman EA, Nagan N, Zhu H, Akmaev VR, Zhou Z, Rohlfs EM, et al. Pan-ethnic carrier screening and prenatal diagnosis for spinal muscular atrophy: clinical laboratory analysis of > 72,400 specimens. Eur J Hum Genet. 2012;20(1):27–32.
Singh RN, Singh NN. Mechanism of splicing regulation of spinal muscular atrophy genes. Adv Neurobiol. 2018;20:31–61.
Butchbach MER. Copy number variations in the survival motor neuron genes: implications for spinal muscular atrophy and other neurodegenerative diseases. Front Mol Biosci. 2016;3:1–10.
Schrank B, Götz R, Gunnersen JM, Ure JM, Toyka KV, Smith AG, et al. Inactivation of the survival motor neuron gene, a candidate gene for human spinal muscular atrophy, leads to massive cell death in early mouse embryos. Proc Natl Acad Sci USA. 1997;94(18):9920–5.
Duque SI, Arnold WD, Odermatt P, Li X, Porensky PN, Schmelzer L, et al. A large animal model of spinal muscular atrophy and correction of phenotype. Ann Neurol. 2015;77(3):399–414.
Singh NK, Singh NN, Androphy EJ, Singh RN. Splicing of a critical exon of human survival motor neuron is regulated by a unique silencer element located in the last intron. Mol Cell Biol. 2006;26(4):1333–46.
Ratni H, Ebeling M, Baird J, Bendels S, Bylund J, Chen KS, et al. Discovery of risdiplam, a selective survival of motor neuron-2 ( SMN2) gene splicing modifier for the treatment of spinal muscular atrophy (SMA). J Med Chem. 2018;61(15):6501–17.
Poirier A, Weetall M, Heinig K, Bucheli F, Schoenlein K, Alsenz J, et al. Risdiplam distributes and increases SMN protein in both the central nervous system and peripheral organs. Pharmacol Res Perspect. 2018;6(6):1–13.
Oskoui M, Levy G, Garland CJ, Gray JM, O’Hagen J, De Vivo DC, et al. The changing natural history of spinal muscular atrophy type 1. Neurology. 2007;69(20):1931–6.
Finkel RS, McDermott MP, Kaufmann P, Darras BT, Chung WK, Sproule DM, et al. Observational study of spinal muscular atrophy type I and implications for clinical trials. Neurology. 2014;83(9):810–7.
Kaufmann P, McDermott MP, Darras BT, Finkel R, Kang P, Oskoui M, et al. Observational study of spinal muscular atrophy type 2 and 3: Functional outcomes over 1 year. Arch Neurol. 2011;68(6):779–86.
De Sanctis R, Pane M, Coratti G, Palermo C, Leone D, Pera MC, et al. Clinical phenotypes and trajectories of disease progression in type 1 spinal muscular atrophy. Neuromuscul Disord. 2018;28(1):24–8.
Yeo CJJ, Darras BT. Overturning the paradigm of spinal muscular atrophy as just a motor neuron disease. Pediatr Neurol. 2020;109:12–9.
Besse A, Astord S, Marais T, Roda M, Giroux B, Lejeune FX, et al. AAV9-mediated expression of SMN restricted to neurons does not rescue the spinal muscular atrophy phenotype in mice. Mol Ther. 2020;28(8):1887–901.
Sleutjes BTHM, Wijngaarde CA, Wadman RI, Otto LAM, Asselman FL, Cuppen I, et al. Assessment of motor unit loss in patients with spinal muscular atrophy. Clin Neurophysiol. 2020;131(6):1280–6.
Murray LM, Beauvais A, Bhanot K, Kothary R. Defects in neuromuscular junction remodelling in the Smn2B/- mouse model of spinal muscular atrophy. Neurobiol Dis. 2013;49(1):57–67. https://doi.org/10.1016/j.nbd.2012.08.019.
Boyer JG, Murray LM, Scott K, De Repentigny Y, Renaud JM, Kothary R. Early onset muscle weakness and disruption of muscle proteins in mouse models of spinal muscular atrophy. Skelet Muscle. 2013;3(1):24.
Lee Y, Mikesh M, Smith I, Rimer M, Thompson W. Muscles in a mouse model of spinal muscular atrophy show profound defects in neuromuscular development even in the absence of failure in neuromuscular transmission or loss of motor neurons. Dev Biol. 2011;356(2):432–44. https://doi.org/10.1016/j.ydbio.2011.05.667.
Martinez TL, Kong L, Wang X, Osborne MA, Crowder ME, Van Meerbeke JP, et al. Survival motor neuron protein in motor neurons determines synaptic integrity in spinal muscular atrophy. J Neurosci. 2012;32(25):8703–15.
Janssen MMHP, Peeters LHC, De Groot IJM. Quantitative description of upper extremity function and activity of people with spinal muscular atrophy. J Neuroeng Rehabil. 2020;17(1):1–14.
Wijngaarde CA, Veldhoen ES, Van Eijk RPA, Stam M, Otto LAM, Asselman FL, et al. Natural history of lung function in spinal muscular atrophy. Orphanet J Rare Dis. 2020;15(1):1–12.
Groen EJN, Talbot K, Gillingwater TH. Advances in therapy for spinal muscular atrophy: promises and challenges. Nat Rev Neurol. 2018;14(4):214–24. https://doi.org/10.1038/nrneurol.2018.4.
Sergott RC, Amorelli GM, Baranello G, Barreau E, Beres S, Kane S, et al. Risdiplam treatment has not led to retinal toxicity in patients with spinal muscular atrophy. Ann Clin Transl Neurol. 2021;8(1):54–65.
Baranello G, Darras BT, Day JW, Deconinck N, Klein A, Masson R, et al. Risdiplam in type 1 spinal muscular atrophy. N Engl J Med. 2021;384(10):915–23.
Dhillon S. Risdiplam: first approval. Drugs. 2020;80(17):1853–8.
Baranello G, Bertini E, Chiriboga C, Darras BT, Day JW, Deconinck N, et al. Pooled safety data from the risdiplam (RG7916) clinical trial development program. Neurology. 2020;94(15 Supplement):1267.
Ando S, Suzuki S, Okubo S, Ohuchi K, Takahashi K, Nakamura S, et al. Discovery of a CNS penetrant small molecule SMN2 splicing modulator with improved tolerability for spinal muscular atrophy. Sci Rep. 2020;10(1):1–17.
Hua Y, Vickers TA, Baker BF, Bennett CF, Krainer AR. Enhancement of SMN2 exon 7 inclusion by antisense oligonucleotides targeting the exon. PLoS Biol. 2007;5(4):729–44.
Berciano MT, Puente-Bedia A, Medina-Samamé A, Rodríguez-Rey JC, Calderó J, Lafarga M, et al. Nusinersen ameliorates motor function and prevents motoneuron Cajal body disassembly and abnormal poly(A) RNA distribution in a SMA mouse model. Sci Rep. 2020;10(1):1–14.
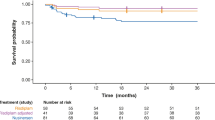
Finkel RS, Mercuri E, Darras BT, Connolly AM, Kuntz NL, Kirschner J, et al. Nusinersen versus sham control in infantile-onset spinal muscular atrophy. N Engl J Med. 2017;377(18):1723–32.
Pera MC, Coratti G, Forcina N, Mazzone ES, Scoto M, Montes J, et al. Content validity and clinical meaningfulness of the HFMSE in spinal muscular atrophy. BMC Neurol. 2017;17(1):1–11.
Mercuri E, Darras BT, Chiriboga CA, Day JW, Campbell C, Connolly AM, et al. Nusinersen versus sham control in later-onset spinal muscular atrophy. N Engl J Med. 2018;378(7):625–35.
De VDC, Bertini E, Swoboda KJ, Hwu W, Crawford TO, Finkel RS, et al. Nusinersen initiated in infants during the presymptomatic stage of SMA: Interim efficacy and safety results from the Phase 2 NURTURE study. Neuromuscular. 2019;29:842–56.
Pane M, Palermo C, Messina S, Sansone VA, Bruno C, Catteruccia M, et al. Nusinersen in type 1 SMA infants, children and young adults: preliminary results on motor function. Neuromuscul Disord. 2018;28(7):582–5.
Pane M, Coratti G, Sansone VA, Messina S, Bruno C, Catteruccia M, et al. Nusinersen in type 1 spinal muscular atrophy: twelve-month real-world data. Ann Neurol. 2019;86(3):443–51.
Darras BT, Chiriboga CA, Iannaccone ST, Swoboda KJ, Montes J, Mignon L, et al. Nusinersen in later-onset spinal muscular atrophy: long-term results from the phase 1/2 studies. Neurology. 2019;92(21):e2492–506.
Daimee M, Shakti N. Nusinersen Initiation in adults with spinal muscular atrophy. Neurology. 2020;94(15 Supplement):4906.
Day JW, Swoboda KJ, Darras BT, Chiriboga CA, Iannaccone ST, De Vivo DC, et al. Longer-term experience with nusinersen in teenagers and young adults with spinal muscular atrophy: results from the CS2/CS12 and SHINE studies. Neurology. 2020;94(15 Supplement):1132.
Montes J, Young SD, Mazzone E, Pasternak A, Glanzman A, Finkel R, et al. Ambulatory function and fatigue in nusinersen-treated children with spinal muscular atrophy. Neurology. 2018;90(15 Supplement):P2.322.
Chiriboga CA, Swoboda KJ, Darras BT, Iannaccone ST, Montes J, De Vivo DC, et al. Results from a phase 1 study of nusinersen (ISIS-SMN Rx) in children with spinal muscular atrophy. Neurology. 2016;86(10):890–7.
Darras BT, De Vivo DC, Farrar MA, Mercuri E, Finkel RS, Foster R, et al. Safety profile of nusinersen in presymptomatic and infantile-onset spinal muscular atrophy (SMA): interim results from the NURTURE and ENDEAR-SHINE studies. Neurology. 2020;94(15 Supplement):1659.
Darras BT, Farrar MA, Mercuri E, Finkel RS, Foster R, Hughes SG, et al. An integrated safety analysis of infants and children with symptomatic spinal muscular atrophy (SMA) treated with nusinersen in seven clinical trials. CNS Drugs. 2019;33(9):919–32. https://doi.org/10.1007/s40263-019-00656-w.
Wurster CD, Winter B, Wollinsky K, Ludolph AC, Uzelac Z, Witzel S, et al. Intrathecal administration of nusinersen in adolescent and adult SMA type 2 and 3 patients. J Neurol. 2019;266(1):183–94. https://doi.org/10.1007/s00415-018-9124-0.
Kizina K, Stolte B, Totzeck A, Bolz S, Schlag M, Ose C, et al. Fatigue in adults with spinal muscular atrophy under treatment with nusinersen. Sci Rep. 2020;10(1):1–12.
Osmanovic A, Ranxha G, Kumpe M, Müschen L, Binz C, Wiehler F, et al. Treatment expectations and patient-reported outcomes of nusinersen therapy in adult spinal muscular atrophy. J Neurol. 2020;267(8):2398–407. https://doi.org/10.1007/s00415-020-09847-8.
Sansone VA, Pirola A, Albamonte E, Pane M, Lizio A, D’Amico A, et al. Respiratory needs in patients with type 1 spinal muscular atrophy treated with nusinersen. J Pediatr. 2020;219:223-228.e4.
Audic F, De La Banda MGG, Bernoux D, Ramirez-Garcia P, Durigneux J, Barnerias C, et al. Effects of nusinersen after one year of treatment in 123 children with SMA type 1 or 2: A French real-life observational study. Orphanet J Rare Dis. 2020;15(1):1–11.
Hammond SM, Hazell G, Shabanpoor F, Saleh AF, Bowerman M, Sleigh JN, et al. Systemic peptide-mediated oligonucleotide therapy improves long-term survival in spinal muscular atrophy. Proc Natl Acad Sci USA. 2016;113(39):10962–7.
Passini MA, Bu J, Roskelley EM, Richards AM, Sardi SP, O’Riordan CR, et al. CNS-targeted gene therapy improves survival and motor function in a mouse model of spinal muscular atrophy. J Clin Invest. 2010;120(4):1253–64.
Foust KD, Wang X, McGovern VL, Braun L, Bevan AK, Haidet AM, et al. Rescue of the spinal muscular atrophy phenotype in a mouse model by early postnatal delivery of SMN. Nat Biotechnol. 2010;28(3):271–4.
Dominguez E, Marais T, Chatauret N, Benkhelifa-Ziyyat S, Duque S, Ravassard P, et al. Intravenous scAAV9 delivery of a codon-optimized SMN1 sequence rescues SMA mice. Hum Mol Genet. 2011;20(4):681–93.
Mendell JR, Al-Zaidy S, Shell R, Arnold WD, Rodino-Klapac LR, Prior TW, et al. Single-dose gene-replacement therapy for spinal muscular atrophy. N Engl J Med. 2017;377(18):1713–22.
Lowes LP, Alfano LN, Arnold WD, Shell R, Prior TW, McColly M, et al. Impact of age and motor function in a phase 1/2A study of infants with SMA type 1 receiving single-dose gene replacement therapy. Pediatr Neurol. 2019;98:39–45.
Dabbous O, Sproule DM, Feltner DE, Ogrinc FG, Menier M, Droege M, et al. Event-free survival and motor milestone achievement following AVXS-101 and nusinersen interventions contrasted to natural history for type I spinal muscular atrophy patients. Neurology. 2019;92(15 Supplement):S25.005.
Dabbous O, Maru B, Jansen JP, Lorenzi M, Cloutier M, Guérin A, et al. Survival, motor function, and motor milestones: comparison of AVXS-101 relative to nusinersen for the treatment of infants with spinal muscular atrophy type 1. Adv Ther. 2019;36:1164–76.
Sandrock AW, Farwell W. Comparisons between separately conducted clinical trials: letter to the editor regarding Dabbous O, Maru B, Jansen JP, Lorenzi M, Cloutier M, Guérin A, et al. Adv Ther (2019) 36(5):1164–76. doi:10.1007/s12325-019-00923-8. Adv Ther. 2019;36(11):2979–81. https://doi.org/10.1007/s12325-019-01087-1.
Malone DC, Dean R, Arjunji R, Jensen I, Cyr P, Miller B, et al. Cost-effectiveness analysis of using onasemnogene abeparvocec (AVXS-101) in spinal muscular atrophy type 1 patients. J Mark Access Health Policy. 2019;7(1):1601484.
Burgart AM, Magnus D, Tabor HK, Paquette EDT, Frader J, Glover JJ, et al. Ethical challenges confronted when providing nusinersen treatment for spinal muscular atrophy. JAMA Pediatr. 2018;172(2):188–92.
Zuluaga-Sanchez S, Teynor M, Knight C, Thompson R, Lundqvist T, Ekelund M, et al. Cost effectiveness of nusinersen in the treatment of patients with infantile-onset and later-onset spinal muscular atrophy in Sweden. Pharmacoeconomics. 2019;37(6):845–65.
Harada Y, Arya K, Napchan-Pomerantz G, Kauffmann R, Agarwal A, Stefans V, et al. Combination therapy with nusinersen and AVXS-101: a real-world clinical experience. Neurology. 2020;94(15 Supplement):4152.
Harada Y, Rao VK, Arya K, Kuntz NL, DiDonato CJ, Napchan-Pomerantz G, et al. Combination molecular therapies for type 1 spinal muscular atrophy. Muscle Nerve. 2020;62(4):550–4.
Matesanz SE, Curry C, Gross B, Rubin AI, Linn R, Yum SW, et al. Clinical course in a patient with spinal muscular atrophy type 0 treated with nusinersen and onasemnogene abeparvovec. J Child Neurol. 2020;35(11):717–23.
Lim KRQ, Echigoya Y, Nagata T, Kuraoka M, Kobayashi M, Aoki Y, et al. Efficacy of multi-exon skipping treatment in duchenne muscular dystrophy dog model neonates. Mol Ther. 2019;27(1):76–86. https://doi.org/10.1016/j.ymthe.2018.10.011.
Blain AM, Greally E, McClorey G, Manzano R, Betts CA, Godfrey C, et al. Peptide-conjugated phosphodiamidate oligomer-mediated exon skipping has benefits for cardiac function in mdx and Cmah-/-mdx mouse models of Duchenne muscular dystrophy. PLoS ONE. 2018;13(6):e0198897.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflicts of Interest
TY is a founder and shareholder of OligomicsTx, which aims to commercialize antisense oligonucleotide technology. OS has no conflicts of interest to report.
Author Contributions
Literature review draft preparation by Omar Sheikh. Supervision and funding acquisition by Toshifumi Yokota. Review and editing performed jointly. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by Muscular Dystrophy Canada, the Friends of Garrett Cumming Research Fund, the HM Toupin Neurological Science Research Fund, Fulbright Scholarship Program, and the Women and Children’s Health Research Institute (WCHRI).
Ethics approval
Not applicable.
Consent to participate
Not applicable.
Consent to publish
Not applicable.
Availability of data and material
Not applicable.
Code availability
Not applicable.
Acknowledgements
The authors wish to thank Mary Claire De Villa for writing feedback.
Rights and permissions
About this article
Cite this article
Sheikh, O., Yokota, T. Restoring Protein Expression in Neuromuscular Conditions: A Review Assessing the Current State of Exon Skipping/Inclusion and Gene Therapies for Duchenne Muscular Dystrophy and Spinal Muscular Atrophy. BioDrugs 35, 389–399 (2021). https://doi.org/10.1007/s40259-021-00486-7
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40259-021-00486-7