Abstract
Background
Atopic dermatitis is a chronic inflammatory skin disease that can negatively impact work productivity and daily activities. Ruxolitinib cream, a Janus kinase inhibitor, demonstrated efficacy and safety in patients with atopic dermatitis in two phase III studies (TRuE-AD1 and TRuE-AD2).
Objective
This post hoc analysis sought to describe the effects of ruxolitinib cream on work productivity and activity impairment from pooled data from the phase III studies, to estimate indirect costs due to atopic dermatitis, and to estimate the incremental cost savings with ruxolitinib cream versus vehicle cream.
Methods
Patients in both studies were ≥ 12 years old with atopic dermatitis for ≥ 2 years, an Investigator’s Global Assessment score of 2 or 3, and a 3–20% affected body surface area at baseline. Patients were randomized 2:2:1 to receive ruxolitinib cream (0.75% or 1.5%) or vehicle cream for 8 weeks. Patient self-reported productivity in the efficacy-evaluable population was assessed at weeks 2, 4, and 8 using the Work Productivity and Activity Impairment Questionnaire-Specific Health Problem version 2.0. Statistical significance for the two doses versus vehicle was calculated using an analysis of covariance. Work Productivity and Activity Impairment overall work impairment scores were converted to a model of costs per employed patient due to lost productivity and incremental cost savings from ruxolitinib cream treatment using a human capital approach.
Results
Of 1249 patients enrolled (median age, 32 years; female sex, 61.7%), 1208 were included in the efficacy-evaluable population. Patients applying 0.75% or 1.5% ruxolitinib cream had significant changes in overall work impairment (− 17.9% [0.75% strength] and − 15.0% [1.5% strength] vs − 5.7% for vehicle; p < 0.0001 for both) and daily activity impairment (− 20.6% [0.75% strength] and − 21.5% [1.5% strength] vs − 10.6% for vehicle; p < 0.0001 for both). These corresponded to estimated lost productivity costs in 2021 US dollars of $1313 (0.75% strength) and $1242 (1.5% strength) versus $2008 (vehicle) over the 8-week trial period. Compared with a patient receiving vehicle, incremental annual indirect cost savings were estimated to be $5302 with 0.75% ruxolitinib cream and $4228 with 1.5% ruxolitinib cream.
Conclusions
Ruxolitinib cream therapy is associated with improved work productivity and daily activity compared with vehicle and is estimated to reduce the indirect cost burden on the patient.
Clinical trial registration
ClinicalTrials.gov identifiers: NCT03745638 (registered 19 November, 2018) and NCT03745651 (registered 19 November, 2018)
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Treatment of atopic dermatitis with ruxolitinib cream significantly improved patient-reported measures of work productivity and daily activity impairment. |
Using a human capital approach, incremental annual indirect cost savings for patients applying 0.75% or 1.5% ruxolitinib cream were estimated to be $5302 and $4228, respectively. |
1 Background
Atopic dermatitis (AD) is a chronic inflammatory skin disease characterized by itching, dryness, and redness that occurs in approximately 10–15% of children and 5–10% of adults in the USA [1,2,3,4]. Atopic dermatitis is associated with pruritus, skin pain, frequent flares, depression, anxiety, and sleep deprivation that can negatively impact work productivity and daily activities [2, 5, 6]. Even patients with mild AD and their caregivers may incur substantial indirect costs based on missed days or lost productivity at work and career modification and have reduced quality of life [7].
Janus kinases (JAKs) play important roles in the pathogenesis of AD and itch by mediating proinflammatory cytokines in skin and sensory neurons [8, 9]. A topical cream formulation of ruxolitinib, a selective inhibitor of JAK1 and JAK2 [10], is approved by the US Food and Drug Administration for the treatment of patients with mild to moderate AD aged at least 12 years who are not immunocompromised and whose disease is not adequately controlled with topical prescription therapies, or when those therapies are not advisable [11]. Regulatory approval was based on two phase III AD studies of identical design (Topical Ruxolitinib Evaluation in Atopic Dermatitis [TRuE-AD] 1 [NCT03745638] and TRuE-AD2 [NCT03745651]), in which ruxolitinib cream demonstrated anti-inflammatory activity with antipruritic action versus vehicle and was well tolerated [12]. The objective of this post hoc analysis was to describe the effects of ruxolitinib cream on work productivity and activity impairment based on pooled data from these two phase III trials in adolescent and adult patients with AD. From these data, the overall associated indirect costs from lost productivity to the individual patient were estimated.
2 Methods
2.1 Patients and Study Design
The two phase III studies of identical design, TRuE-AD1 (NCT03745638) and TRuE-AD2 (NCT03745651), were randomized, double-blind, and vehicle controlled, and the results were previously reported [12]. Eligible patients were aged at least 12 years with AD for at least 2 years and had an Investigator’s Global Assessment (IGA) score of 2 or 3 and an affected body surface area of 3–20% (excluding scalp). Patients were randomized 2:2:1 to one of two ruxolitinib cream strength regimens (0.75% or 1.5%) or vehicle cream, applied twice daily as continuous treatment of initially affected areas over an 8-week double-blind trial period. Additional details regarding patients and study design were previously reported [12].
2.2 Assessments
In both studies, patient self-reported productivity was assessed using the Work Productivity and Activity Impairment Questionnaire-Specific Health Problem version 2.0 (WPAI:SHP v2.0) at weeks 2, 4, and 8. The WPAI:SHP v2.0 is a six-item questionnaire that measures the effect of overall health and specific symptoms on productivity at work and regular activity outside of work during the previous 7 days, including work time missed due to AD (absenteeism), impairment while working with AD (presenteeism), overall AD-related work impairment (absenteeism and presenteeism), and AD-related activity impairment. Scores are expressed as a percentage of impairment, with higher scores indicating greater impairment [13]. Only patients who self-identified as having paid employment were asked questions regarding absenteeism, presenteeism, and overall work impairment.
2.3 Statistical Analysis
All analyses were conducted in the efficacy-evaluable population using the pooled data from both studies. The statistical significance of changes from baseline in WPAI:SHP scores at weeks 2, 4, and 8 was assessed using an analysis of covariance.
2.4 Indirect Cost Model
The WPAI overall work impairment scores were used to assess the cost of lost productivity and potential cost savings per employed patient resulting from the use of ruxolitinib cream using a human capital approach. Scores at week 6 were imputed as the means of weeks 4 and 8. The proportion of time with impairment was combined with epidemiologic data on employment status among patients with AD (full time, 79%; part time, 21%) [5] and the median weekly wage from the 2021 US Bureau of Labor Statistics (Table 1) [14]. Employees were stratified by full-time versus part-time employment based on a published study of employment status in patients with AD [5]. Age-specific and sex-specific median weekly wages for full-time and part-time workers were extracted from Bureau of Labor Statistics data and used to create a weighted average weekly wage in 2021 US dollars for patients with AD, considering baseline age and sex. This weighted average cost per week was multiplied by the proportion of overall work impairment, overall and by treatment arm. Indirect costs were calculated based on the baseline WPAI:SHP v2.0 scores (untreated) and those from the vehicle-controlled period (treated). Variance in incremental indirect cost savings was calculated from the upper and lower bounds of the 95% confidence interval for the mean difference in overall work impairment at each timepoint.
3 Results
3.1 Patients
Overall, 1249 patients (median age, 32 years; female sex, 61.7%) were randomized in the two trials (vehicle, n = 250; 0.75% ruxolitinib cream, n = 500; 1.5% ruxolitinib cream, n = 449), and 1208 patients were included in the efficacy analysis [12]. Of these, 678 (56.1%) completed at least one of the work-related questions, and 1205 (99.8%) completed the daily activity impairment question of the WPAI:SHP. Distribution of baseline demographics and clinical characteristics was similar across treatment groups. Across cohorts in the efficacy-evaluable population, 68.6% were White, 24.2% were Black, 3.8% were Asian, and 3.4% were other races (Table 2). Most patients (74.2%) had a baseline IGA score of 3. Mean (standard deviation [SD]) itch numeric rating scale score was 5.1 (2.4) at baseline; 64.4% of patients had a score of at least 4.
3.2 WPAI Scores
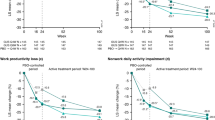
Improvements in WPAI:SHP scores among patients randomized to ruxolitinib cream (0.75% or 1.5%) versus vehicle were observed at weeks 2, 4, and 8 for domains of presenteeism, overall work impairment, and daily activity impairment (Fig. 1 and Table 3). Statistically significant differences in percentage change from baseline versus vehicle at week 8 were observed for presenteeism (− 19.2%/− 19.8% for 0.75%/1.5% strength vs − 12.3% for vehicle; p < 0.0001 for both), overall work impairment (− 17.9%/− 15.0% vs − 5.7%; p < 0.0001 for both), and daily activity impairment (− 20.6%/− 21.5% vs − 10.6%; p < 0.0001 for both). Significant differences at week 8 were noted for absenteeism with 0.75% ruxolitinib cream versus vehicle (1.3% vs 7.4%; p < 0.05), and 1.5% ruxolitinib cream (4.8%) showed a trend toward difference versus vehicle.
Change from baseline in Work Productivity and Activity Impairment Questionnaire-Specific Health Problem version 2.0 (WPAI:SHP v2.0) scores for domains of (A) absenteeism, (B) presenteeism, (C) overall work impairment, and (D) daily activity impairment. CI confidence interval, *p < 0.05 versus vehicle; ****p < 0.0001 versus vehicle
3.3 Indirect Costs
Estimated indirect costs per employed patient were lower for patients using either strength of ruxolitinib cream versus patients using vehicle (Table 4). These costs were lower for each 2-week period of the 8-week vehicle-controlled period. Total estimated indirect cost savings per patient over the 8-week trial period for 0.75% and 1.5% ruxolitinib cream versus vehicle were $695 and $766, respectively (Fig. 2A). Over a 1-year horizon, reductions in indirect costs owing to treatment were estimated to be $2127 for vehicle cream, $7428 for 0.75% ruxolitinib cream, and $6355 for 1.5% ruxolitinib cream (Fig. 2B). Incremental indirect cost savings compared with patients randomized to vehicle cream were estimated to be $5302 ($5126–$5477) and $4228 ($3987–$4469) for patients randomized to 0.75% and 1.5% ruxolitinib cream, respectively.
4 Discussion
In pooled results from two phase III trials, patients with AD who had an IGA score of 2 or 3, an affected body surface area of 3−20%, and applied either 0.75% or 1.5% ruxolitinib cream reported improvement in work productivity versus vehicle, with significant improvements in presenteeism (19.2%/19.8% vs 12.3%), overall work impairment scores (17.9%/15.0% vs 5.7%), and activity impairment (20.6%/21.5% vs 10.6%) scores at week 8. Previous studies in patients with psoriasis [15] and psoriatic arthritis [16] suggest that a 15–20% improvement in each WPAI:SHP domain is clinically meaningful, defined as the minimal improvement in an outcome that is perceived by patients as being beneficial. Improvements in work productivity with ruxolitinib cream are generally comparable to results obtained in other studies with oral JAK inhibitors in patients with moderate to severe AD. Patients who were treated with abrocitinib, an oral JAK1 inhibitor, reported a 22.9% reduction in overall work impairment after 12 weeks of therapy compared with 5.0% for treatment with placebo [17]. The combination of topical corticosteroid cream with baricitinib, an oral JAK1/JAK2 inhibitor, in adult patients with AD eligible for systemic treatment reduced the overall work impairment by 26.3%, compared with 12.2% for topical corticosteroids and placebo, after 2 weeks of therapy [18]. Although no real-world observational data are available for other JAK inhibitors in AD, improvements in work productivity with the application of ruxolitinib cream also compared favorably with improvements with dupilumab observed in Dutch patients with moderate to severe AD (mean [SD] baseline impairment, 35.5% [28.5%]; mean [SD] impairment at 52 weeks, 11.5% [18.4%]) [19]. Of note, underlying comorbidities may have an impact on work productivity. For example, in the Dutch patients, the mean (SD) improvement from baseline in overall work impairment significantly differed between patients who did not have self-reported asthma (− 30.6% [29.4%]) and those who had self-reported asthma (− 19.9% [26.3%]) [19]. Furthermore, claims database analyses of patients in the USA found that nonresponse with systemic agents, such as conventional immunosuppressive agents or dupilumab, was significantly associated with having comorbid respiratory conditions [20] and that 59% of non-responders to dupilumab had Quan-Charlson Comorbidity Index values of 3 or 4 [21]. Such observations will need to be considered in real-world studies of ruxolitinib cream in patients with AD.
Ruxolitinib cream improves several signs and symptoms of AD that may contribute to the observed improvements in work productivity. As demonstrated in the TRuE-AD clinical trials, application of ruxolitinib cream alleviates pruritus [12]. In addition, preliminary data from the TRuE-AD trials showed that ruxolitinib cream improved skin pain [22] and provided a clinical benefit regardless of the anatomic region (including head and neck, trunk, upper limbs, and lower limbs) [23]. Ruxolitinib cream may also improve sleep, as measured by a ≥ 6-point improvement from baseline in the Patient-Reported Outcomes Measurement Information System (PROMIS) sleep disturbance questionnaire in the TRuE-AD1 study, although improvements in the PROMIS questionnaire were not statistically significant in the identically designed TRuE-AD2 study [12]. Itch and skin pain in patients with moderate or severe AD correlate with severity of sleep disturbance, which contributes to impairments in work productivity [24, 25]. Pruritus has also been directly correlated with impaired concentration, resulting in increased presenteeism in patients with AD, which may be a greater problem than absenteeism [26, 27]. Patients with AD experiencing fatigue, daytime sleepiness, and/or insomnia reported greater absenteeism than those with either AD or fatigue alone [4]. Finally, involvement in readily visible areas of the body, such as the face, is associated with impaired quality of life, which is in turn associated with indirect costs [28]. Additionally, patients with chronic hand eczema, another inflammatory skin condition, incur a substantial impairment in work productivity [29]. Managing physicians may promote the maintenance of or improvements in their patients’ work productivity by screening for these signs and symptoms and tailoring their treatment strategy accordingly.
Previous studies reported an increased work impairment and indirect costs among patients with AD. In a recent survey of patients receiving topical therapy for moderate to severe AD, those with uncontrolled disease had a greater overall work impairment than those who had controlled disease [30]. Notably, patients from this survey and responders with mild to moderate AD in another survey reported a less severe overall work impairment compared with patients at baseline in the current study [5, 30]. A recent claims analysis of commercial-insured and Medicare-insured adults in the USA found that work absences and short-term disability claims were more common among patients with AD compared with matched controls without AD, contributing to higher indirect costs [31]. These real-world data support previous estimates, which were also calculated using the human capital approach of estimating future loss of income, of increased indirect costs due to absenteeism and presenteeism in adults with uncontrolled AD compared with controlled AD [32] and in patients with AD compared with matched non-AD control patients [26]. In the current analysis, which included a population of patients of whom approximately 90% had been receiving active treatment and not achieved control prior to the study, estimated indirect costs were substantially reduced in patients with AD who applied ruxolitinib cream. These estimates were lower than estimated reductions in indirect costs in patients with moderate to severe AD treated with abrocitinib, even though an improvement in the overall work impairment was similar, indicating that the increased severity of the population in that analysis may have influenced the baseline indirect costs and that use of the overall annual median wage from the first quarter of 2020 and the lack of interim timepoints may have overestimated indirect costs [17].
This analysis had several limitations to consider. The data were from randomized controlled trials with a specified population and may not be reflective of real-world experiences. In particular, the trial design excluded patients with severe AD as indicated by a greater IGA score (> 3) or affected body surface area (> 20%), a population that tends to be more resistant to therapy [33]. Extrapolation from the short-term vehicle-controlled period to annual costs may not account for potential AD disease progression in which ruxolitinib cream may no longer be effective. Furthermore, because of the limited data on the use of topical agents in AD treatment, indirect cost comparisons were made versus vehicle rather than an active topical agent. This potentially overestimates the cost savings with ruxolitinib cream compared with other topical therapies. Additionally, only 56.1% of patients in our study completed the work-related questions, likely reflecting the proportion of the study population in employment and potentially providing an underestimation of the work-related impairment when considering AD may prevent some people from working. Additionally, there was a drop-off in WPAI:SHP completion over the 8-week study period, with approximately 80% of patients applying ruxolitinib cream completing the baseline questionnaire at week 8. This drop-off may have led to an underestimation of productivity loss as the worst affected patients may not have completed the questionnaire in later weeks. Furthermore, the model used does not account for all indirect costs, such as impaired quality of life. Finally, this analysis focuses only on indirect costs, without consideration of direct medical and pharmacy costs, including the cost of ruxolitinib cream.
5 Conclusions
In summary, ruxolitinib cream is associated with significantly improved work productivity and daily activity compared with vehicle for patients with AD. Patients randomized to ruxolitinib cream reported reduced work time missed, work impairment, and daily activity impairment compared with vehicle. Results of the indirect cost analysis showed that ruxolitinib cream may also significantly reduce the annual indirect cost burden on patients with AD.
References
Chiesa Fuxench ZC, Block JK, Boguniewicz M, Boyle J, Fonacier L, Gelfand JM, et al. Atopic Dermatitis in America Study: a cross-sectional study examining the prevalence and disease burden of atopic dermatitis in the US adult population. J Invest Dermatol. 2019;139(3):583–90.
Langan SM, Irvine AD, Weidinger S. Atopic dermatitis. Lancet. 2020;396(10247):345–60.
Silverberg JI, Simpson EL. Associations of childhood eczema severity: a US population-based study. Dermatitis. 2014;25(3):107–14.
Silverberg JI, Garg NK, Paller AS, Fishbein AB, Zee PC. Sleep disturbances in adults with eczema are associated with impaired overall health: a US population-based study. J Invest Dermatol. 2015;135(1):56–66.
Andersen L, Nyeland ME, Nyberg F. Increasing severity of atopic dermatitis is associated with a negative impact on work productivity among adults with atopic dermatitis in France, Germany, the UK and the USA. Br J Dermatol. 2020;182(4):1007–16.
Whiteley J, Emir B, Seitzman R, Makinson G. The burden of atopic dermatitis in US adults: results from the 2013 National Health and Wellness Survey. Curr Med Res Opin. 2016;32(10):1645–51.
Hebert AA, Stingl G, Ho LK, Lynde C, Cappelleri JC, Tallman AM, et al. Patient impact and economic burden of mild-to-moderate atopic dermatitis. Curr Med Res Opin. 2018;34(12):2177–85.
Bao L, Zhang H, Chan LS. The involvement of the JAK-STAT signaling pathway in chronic inflammatory skin disease atopic dermatitis. JAKSTAT. 2013;2(3): e24137.
Oetjen LK, Mack MR, Feng J, Whelan TM, Niu H, Guo CJ, et al. Sensory neurons co-opt classical immune signaling pathways to mediate chronic itch. Cell. 2017;171(1):217–28.
Quintás-Cardama A, Vaddi K, Liu P, Manshouri T, Li J, Scherle PA, et al. Preclinical characterization of the selective JAK1/2 inhibitor INCB018424: therapeutic implications for the treatment of myeloproliferative neoplasms. Blood. 2010;115(15):3109–17.
Opzelura™ (ruxolitinib cream). Full prescribing information. Wilmington, DE: Incyte Corporation; 2022.
Papp K, Szepietowski JC, Kircik L, Toth D, Eichenfield L, Leung DY, et al. Efficacy and safety of ruxolitinib cream for the treatment of atopic dermatitis: results from two phase 3, randomized, double-blind studies. J Am Acad Dermatol. 2021;85(4):863–72.
Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. Pharmacoeconomics. 1993;4(5):353–65.
US Bureau of Labor Statistics. Usual weekly earnings of wage and salary workers. 2021. https://www.bls.gov/. Accessed 22 Feb 2021.
Wu JJ, Lin C, Sun L, Goldblum O, Zbrozek A, Burge R, et al. Minimal clinically important difference (MCID) for Work Productivity and Activity Impairment (WPAI) questionnaire in psoriasis patients. J Eur Acad Dermatol Venereol. 2019;33(2):318–24.
Tillett W, Lin CY, Zbrozek A, Sprabery AT, Birt J. A threshold of meaning for work disability improvement in psoriatic arthritis measured by the Work Productivity and Activity Impairment Questionnaire. Rheumatol Ther. 2019;6(3):379–91.
Gooderham MJ, Chu CY, Rojo R, Valdez H, Biswas P, Cameron MC, et al. Economic impact of abrocitinib monotherapy and combination therapy in patients with moderate-to-severe atopic dermatitis: results from JADE MONO-2 and JADE COMPARE. JAAD Int. 2021;4:46–8.
Wollenberg A, Nakahara T, Maari C, Peris K, Lio P, Augustin M, et al. Impact of baricitinib in combination with topical steroids on atopic dermatitis symptoms, quality of life and functioning in adult patients with moderate-to-severe atopic dermatitis from the BREEZE-AD7 phase 3 randomized trial. J Eur Acad Dermatol Venereol. 2021;35(7):1543–52.
Ariens LFM, Bakker DS, Spekhorst LS, Van der Schaft J, Thijs JL, Haeck I, et al. Rapid and sustained effect of dupilumab on work productivity in patients with difficult-to-treat atopic dermatitis: results from the Dutch BioDay registry. Acta Derm Venereol. 2021;101(10):adv00573.
Wu JJ, Lafeuille MH, Emond B, Fakih I, Duh MS, Cappelleri JC, et al. Real-world effectiveness of newly initiated systemic therapy for atopic dermatitis in the United States: a claims database analysis. Adv Ther. 2022. https://doi.org/10.1007/s12325-022-02197-z.
Wu JJ, Hong CH, Merola JF, Gruben D, Guler E, Feeney C, et al. Predictors of nonresponse to dupilumab in patients with atopic dermatitis: a machine learning analysis. Ann Allergy Asthma Immunol. 2022;129(3):354-9.e5.
Blauvelt A, Szepietowski JC, Papp K, Simpson E, Silverberg JI, Kim BS, et al. Ruxolitinib cream rapidly decreases skin pain in atopic dermatitis [abstract 325]. J Invest Dermatol. 2021;141(5 Suppl.):S57.
Simpson EL, Bissonnette R, Stein Gold LF, Chiesa Fuxench ZC, Venturanza ME, Ren H, et al., editors. Efficacy of ruxolitinib cream for the treatment of atopic dermatitis by anatomic region: pooled analysis from two randomized phase 3 studies. American Academy of Dermatology (AAD) Annual Meeting; 25-29 Mar 2022; Boston, MA. 2022.
Silverberg JI, Chiesa-Fuxench Z, Margolis D, Boguniewicz M, Fonacier L, Grayson M, et al. Sleep disturbances in atopic dermatitis in US adults. Dermatitis. 2021. https://doi.org/10.1097/DER.0000000000000731 (Epub ahead of print).
Kwatra SG, Gruben D, Fung S, DiBonaventura M. Psychosocial comorbidities and health status among adults with moderate-to-severe atopic dermatitis: a 2017 US National Health and Wellness Survey analysis. Adv Ther. 2021;38(3):1627–37.
Eckert L, Gupta S, Amand C, Gadkari A, Mahajan P, Gelfand JM. Impact of atopic dermatitis on health-related quality of life and productivity in adults in the United States: an analysis using the National Health and Wellness Survey. J Am Acad Dermatol. 2017;77(2):274–9.
Chung J, Simpson EL. The socioeconomics of atopic dermatitis. Ann Allergy Asthma Immunol. 2019;122(4):360–6.
Drucker AM, Wang AR, Li WQ, Sevetson E, Block JK, Qureshi AA. The burden of atopic dermatitis: summary of a report for the National Eczema Association. J Invest Dermatol. 2017;137(1):26–30.
Armstrong A, Hahn-Pedersen J, Bartlett C, Glanville J, Thyssen JP. Economic burden of chronic hand eczema: a review. Am J Clin Dermatol. 2022;23(3):287–300.
Anderson P, Austin J, Lofland JH, Piercy J, Joish VN. Inadequate disease control, treatment dissatisfaction, and quality-of-life impairments among US patients receiving topical therapy for atopic dermatitis. Dermatol Ther (Heidelb). 2021;11(5):1571–85.
Manjelievskaia J, Boytsov N, Brouillette MA, Onyekwere U, Pierce E, Goldblum O, et al. The direct and indirect costs of adult atopic dermatitis. J Manag Care Spec Pharm. 2021;27(10):1416–25.
Ariens LFM, van Nimwegen KJM, Shams M, de Bruin DT, van der Schaft J, van Os-Medendorp H, et al. Economic burden of adult patients with moderate to severe atopic dermatitis indicated for systemic treatment. Acta Derm Venereol. 2019;99(9):762–8.
Johnson BB, Franco AI, Beck LA, Prezzano JC. Treatment-resistant atopic dermatitis: challenges and solutions. Clin Cosmet Investig Dermatol. 2019;12:181–92.
Acknowledgments
The authors thank the patients, investigators, and investigational sites whose participation made the study possible. This study was funded by Incyte Corporation (Wilmington, DE, USA). Writing assistance was provided by Joshua Solomon, PhD, an employee of ICON (Blue Bell, PA, USA), and was funded by Incyte Corporation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
The study was funded by Incyte Corporation (Wilmington, DE, USA).
Conflicts of Interest/Competing Interests
Lisa Bloudek, Kristen Migliaccio-Walle, and Sean D. Sullivan are employees of Curta Inc. and served as paid consultants to Incyte Corporation in connection with this study. Lawrence F. Eichenfield has served as an investigator, consultant, speaker, or data safety monitoring board member for AbbVie, Almirall, Arcutis, Asana BioSciences, Dermavant, Eli Lilly, Forte Biosciences, Galderma, Ichnos/Glenmark, Incyte Corporation, Janssen, LEO Pharma, Novartis, Ortho Dermatologics, Otsuka, Pfizer, Regeneron, and Sanofi Genzyme. Jonathan I. Silverberg has received honoraria for advisory board, speaker, and consultant services from AbbVie, Asana, Bluefin, Boehringer Ingelheim, Celgene, Dermavant, Dermira, Eli Lilly, Galderma, GlaxoSmithKline, Glenmark, Incyte Corporation, Kiniksa, LEO Pharma, Menlo, Novartis, Pfizer, Realm, Regeneron, and Sanofi; and research grants for investigator services from GlaxoSmithKline and Galderma. Vijay N. Joish, Jennifer H. Lofland, and Kang Sun are employees and shareholders of Incyte Corporation. Matthias Augustin has served as a consultant, researcher, and/or has received research grants from AbbVie, ALK-Abelló, Almirall, Amgen, Bayer, Beiersdorf, Biogen, Boehringer Ingelheim, Bristol Myers Squibb, Celgene, Centocor, Dermira, Eli Lilly, Galderma, Genzyme, GlaxoSmithKline, Hexal, Janssen, LEO Pharma, Medac, Menlo Therapeutics, MSD, Mylan B.V., Novartis, Pfizer, Regeneron, Sandoz, Sanofi, Stallergenes, Trevi, and XenoPort. Sean D. Sullivan is an owner of VeriTech Corporation and served as a consultant to Incyte Corporation in connection with this study.
Ethics Approval
The study was conducted in accordance with the International Council on Harmonisation Guideline for Good Clinical Practice, the Declaration of Helsinki, and all other applicable local ethical and legal requirements.
Consent to Participate
Written informed consent or assent was provided by all patients before enrollment.
Consent to publish
Not applicable.
Availability of Data and Material
Incyte Corporation (Wilmington, DE, USA) is committed to data sharing that advances science and medicine while protecting patient privacy. Qualified external scientific researchers may request anonymized datasets owned by Incyte Corporation for the purpose of conducting legitimate scientific research. Researchers may request anonymized datasets from any interventional study (except phase I studies) for which the product and indication were approved on or after 1 January, 2020 in at least one major market (e.g., USA, European Union, Japan). Data will be available for request after the primary publication or 2 years after the study has ended. Information on Incyte Corporation’s clinical trial data sharing policy and instructions for submitting clinical trial data requests are available at: https://www.incyte.com/Portals/0/Assets/Compliance%20and%20Transparency/clinical-trial-data-sharing.pdf?ver=2020-05-21-132838-960.
Code Availability
Not applicable.
Authors’ Contributions
All authors contributed to the study conception and design and development of the manuscript. All authors read and approved the final manuscript.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Bloudek, L., Eichenfield, L.F., Silverberg, J.I. et al. Impact of Ruxolitinib Cream on Work Productivity and Activity Impairment and Associated Indirect Costs in Patients with Atopic Dermatitis: Pooled Results From Two Phase III Studies. Am J Clin Dermatol 24, 109–117 (2023). https://doi.org/10.1007/s40257-022-00734-8
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40257-022-00734-8