Abstract
Introduction
ReCOV is a recombinant protein vaccine that aims to induce cross-neutralization against SARS-CoV-2 variants. The phase I and phase II studies were conducted in New Zealand and the Philippines, respectively, for ReCOV primary series.
Methods
Both studies were randomized, double-blind, placebo-controlled designed among COVID-19 vaccine-naïve healthy adults who received two doses of study vaccination with a 21-day interval. In phase I, 100 younger (15–55 years) and older (56–80 years) subjects were 4:1 randomized to receive ReCOV (20 µg or 40 µg) or placebo. In the phase II study, 347 subjects (≥ 18 years) were 2:1 randomized to receive 40 µg ReCOV or placebo. Subjects that received ReCOV were followed up for 6 months after the second dosing. The safety outcomes included solicited and unsolicited AEs, SAEs, and AESIs. The immunogenicity outcomes were live-virus neutralizing antibody (NAb) against prototype, while pseudovirus NAbs against several SARS-CoV-2 variants were included in phase II as well.
Results
No related SAE, AESI, or AE leading to early discontinuation were reported. The AE incidences were higher in ReCOV groups than placebo group in phase I while they were similar between study groups in phase II. The majority of solicited AEs were mild or moderate with median duration of 1.0–4.0 days. The common (≥ 10%) solicited AEs in phase I were injection site reactions, headache, pyrexia, fatigue, and myalgia, and common reported (≥ 5%) ones in phase II included injection site pain, headache, and pyrexia. Robust neutralizing activities against the prototype were observed in ReCOV groups, peaking at 14 days post the second dosing: in phase I, the GMTs for 20 μg and 40 μg ReCOV groups were 1643.2 IU/mL (95% CI 1188.5, 2271.9) and 1289.2 IU/mL (95% CI 868.3, 1914.1) in younger adults, and 1122.3 IU/mL (95% CI 722.6, 1743.1) and 680.3 IU/mL (95% CI 440.2, 1051.4) in older adults, respectively, while in the ReCOV group of phase II, the GMTs for subjects with seronegative and seropositive status at baseline were 3741.0 IU/mL (95% CI 3113.4, 4495.0) and 6138.3 IU/mL (95% CI 5255.1, 7169.9), respectively. In phase II, substantial levels of pseudovirus NAbs against SARS-CoV-2 variants were demonstrated; the peak GMTs for prototype, Omicron BA.2, and BA.4/5 were 8857, 4441, and 2644, and 15,667.3, 7334.3, and 4478.8 among seronegative and seropositive subjects, respectively. The neutralization persisted till 6 months post the second dosing, with only 2.5- to 5.2-fold declines for Omicron variants.
Conclusions
Two doses of 20 µg and 40 µg ReCOV are safe and immunogenic against SARS-CoV-2 prototype. The cross-neutralizing activities against Omicron variants support ReCOV advance to late-stage clinical trials.
Trial Registration
Phase I study, clinicaltrials.gov NCT04818801; phase II study, clinicaltrials.gov NCT05084989.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Why carry out this study? |
Cumulative data suggested that the current COVID-19 vaccines were unlikely to cope with SARS-CoV-2 infection and related diseases efficiently, due to the waning of vaccine-induced immunity and constant emergence of SARS-CoV-2 variants. |
ReCOV contains the amino acid sequence of the N-terminal domain and receptor binding domain domains of Spike protein, which harbors more neutralization epitopes. Adjuvantisation of this antigen with BFA03, an AS03-like oil-in-water emulsion squalene novel adjuvant, contributed to the robust immunogenic and protective effects of ReCOV against SARS-CoV-2 in animal models. |
These studies were designed to evaluate the safety and immunogenicity elicited by two doses of 20 µg or 40 µg ReCOV. |
What was learned from the study? |
Both 20 µg and 40 µg ReCOV were well tolerated with good safety profiles. No related serious adverse events, adverse events of special interest, or adverse events leading to early discontinuation were reported. The majority of solicited adverse events were mild or moderate, and were transient. |
Two doses of 20 µg and 40 µg ReCOV are immunogenic against the SARS-CoV-2 prototype. Notably, cross-neutralization against Omicron variants was observed, strongly supporting this live-virus-based COVID-19 vaccine moving forward to late-stage clinical trials. |
Introduction
During the global pandemic, coronavirus disease 2019 (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) has resulted in considerable illness and death. By the end of May 2023, more than 760 million confirmed cases of COVID-19 and more than 6.9 million deaths had been reported by World Health Organization (WHO) [1]. The outbreak and extensive spread of COVID-19 have brought heavy economic and medical burden globally, seriously threatening human survival and health. Prophylactic vaccines have become the most effective means to prevent SARS-CoV-2-induced diseases.
Although more than a dozen vaccines have been authorized for emergency use by WHO or national governments, breakthrough infections continuously develop and are challenging the vaccine effectiveness, due to the waning of vaccine-induced immunity and constant emergence of SARS-CoV-2 variants especially Omicron and its sublineages [2,3,4]. WHO warned that Omicron variants can be markedly resistant to neutralization by serum from individuals that were fully vaccinated with one of the four widely used prototype-based COVID-19 vaccines, raising the urgent need for new-generation vaccines, to cope with diseases induced by emerging variants with unforeseen immune escape risks.
ReCOV is expressed in CHO cells, containing the 14–541 amino acid sequence (NTD and RBD domains) of Spike protein for SARS-CoV-2 Wuhan-Hu-1, and is fused with the foldon of T4 bacteriophage at the C-terminus to form a trimerized protein containing NTD-RBD foldon. A preclinical proof-of-concept study showed that the combination of NTD and RBD was superior to either RBD or NTD alone in eliciting neutralizing activity [5]. ReCOV is adjuvanted with BFA03, an AS03-like squalene adjuvant, which is an oil-in-water emulsion containing two immunostimulants (squalene, α-tocopherol). Two-dose immunizations of ReCOV, with an interval of 21 days, elicited potent high titers of virus-specific binding and NAb responses to SARS-CoV-2, and provided complete protection against challenge with SARS-CoV-2 in hACE2 transgenic mice and rhesus macaques [6]. As an antigen-based NAb-guided COVID-19 vaccine, we have observed cross-neutralization activity by primary immunization against Brazilian variant P.1 (Gamma), UK variant B.1.1.7 (Alpha), South African variant B.1.351 (Beta), Indian variants B.1.617.2 (Delta), and Peruvian variant C.37 (Lambda) in animal models. ReCOV is therefore expected to have good broad-spectrum immunogenicity against SARS-CoV-2 prototype and derived variants in humans.
Here we report the safety and immunogenicity results of ReCOV as two-dose primary vaccination series from the phase I (NCT04818801) and the phase II (NCT05084989) studies.
Methods
Trial Design and Oversight
The phase I trial was the first in human study conducted at New Zealand Clinical Research (Christchurch and Auckland, June 2021–May 2022). The phase II study for the primary vaccination series was conducted at St. Paul’s Hospital, Medical City Iloilo, and Health Centrum in the Philippines (January–September 2022). Both studies were based on the randomized, double-blind, placebo-controlled design among healthy adults aged 18 years and older. The placebo in the phase I study was normal saline, while in the phase II it was all compositions of ReCOV vaccine except for the antigen.
In both studies, subjects were excluded if they had a history of COVID-19 or confirmed SARS-CoV-2 infection, positive results by SARS-CoV-2 reverse transcriptase polymerase chain reaction at screening, received any prior vaccine against a coronavirus, were immunized with inactivated vaccines within 14 days or live or attenuated vaccines within 30 days prior to enrollment, with acute or severe or uncontrolled medical conditions, and pregnant women. In the phase I study, subjects with SARS-CoV-2 IgM and/or IgG positive status during screening were also excluded. However, IgM or IgG antibody status was not used as an exclusion criterion in the phase II study.
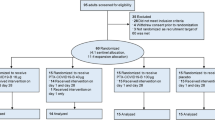
In the phase I study (Fig. 1A), low dose (20 μg) or high dose (40 μg) of ReCOV was administered in dose escalation manner, and progressed sequentially from younger (18–55 years) to older (56–80 years) adults. Subjects in each cohort were randomized to receive ReCOV or placebo at a 4:1 ratio. In each cohort, two sentinel subjects were vaccinated first and followed for safety assessment at least 48 h after the first dosing, before the enrollment of the rest of the subjects. A safety monitoring committee (SMC), composed of investigators and representatives of the sponsor, reviewed all safety data to day 7, and cumulative safety data from previous cohorts prior to approval for escalation from cohort 1 (younger adults, 20 μg ReCOV) to cohort 2 (younger adults, 40 μg ReCOV) and cohort 3 (older adults, 20 μg ReCOV), and from cohort 3 to cohort 4 (older adults, 40 μg ReCOV). In the phase II study (Fig. 1B), 40 μg ReCOV was selected on the basis of its good safety and immunogenicity as shown in the phase I study, and eligible subjects were randomized to receive 40 μg ReCOV or placebo at a 2:1 ratio, stratified by age (18–59 years versus ≥ 60 years) and serostatus of SARS-CoV-2 IgG/IgM at baseline (negative versus positive).
Flow diagram of phase I and phase II studies. SMC safety monitoring committee, EOS end of study. Phase I study (A): cohort 1 will be enrolled and dosed first. Cohorts 2 and 3 will be enrolled and dosed in parallel, after a review of safety data through to 7 days following the first dose from cohort 1 by the SMC. Cohort 4 will be dosed after a review of safety data through to 7 days following the first dose from cohort 3, as well as cumulative data from all previously completed cohorts, if available. Phase II study (B): as a result of the COVID-19 surge from late December 2021 to March 2022 in the Philippines, 51.4% (178) of enrolled subjects were SARS-CoV-2 IgM or IgG positive at baseline, with 118 in ReCOV group and 60 in placebo control group, respectively
In both studies, eligible subjects received two intramuscular doses of ReCOV or placebo, 21 days apart, and were assessed for safety and immunogenicity as scheduled in the protocols. In the phase I study, all subjects were followed up until 30 days post the second dosing, then were individually unblinded to vaccination allocation to allow the placebo recipients to withdraw. ReCOV vaccinated subjects continued follow-up till 6 months after the last dosing. In the phase II study, after all subjects completed the visit 28 days post last dosing, the unblinded subjects in the ReCOV group continued follow-up visit until 6 months after the last dosing.
The sponsor participated in the study design but had no role in data collection and analysis. All authors had full access to all the study data and had final responsibility for the decision to submit for publication. Both studies received funding from Jiangsu Recbio Technology Co., Ltd. The studies were performed in compliance with International Council for Harmonization Good Clinical Practice, and the ethical principles of the Declaration of Helsinki. Prior to initiation of the study, the study protocol and informed consent form were approved by local ethics committees. Informed consent was obtained from each subject before any study procedures were performed.
In the phase I study, the randomization was performed via the electronic data capture system (Viedoc™). To maintain the data integrity, rolling database lock and unblinding was performed based on the dosage cohorts. In the phase II study, randomization was performed via the electronic data capture system (Clinflash EDC), and the double-blinded period was maintained until all subjects completed the visit at 28 days post the second dosing.
Trial Procedures
Safety Assessments
After each dosing, subjects were observed for 30 min (6 h for sentinels in the phase I study) at a site for assessment of immediate AEs. Solicited local and systemic AEs were recorded up to 7 days after each dosing. Unsolicited AEs were recorded from the first vaccination to 30 days (phase I) or 28 days (phase II) after the second dosing. SAEs and AESIs were monitored during the entire study period. AESI was defined as potential immune-mediated diseases and COVID-19-specific AEs based on the Coalition for Epidemic Preparedness Innovations Safety Platform for Emergency vaccines Project guidelines [7].
In the phase I study, AEs were graded for severity according to US Food and Drug Administration Toxicity Grading Scale for Healthy Adult and Adolescent Volunteers Enrolled in Preventive Vaccine Clinical Trials [8]. In the phase II study, China National Medical Product Administration Guidelines for Adverse Event Classification Standards for Clinical Trials of Preventive Vaccines were adopted for AE severity evaluation. Investigators judged the severity gradings and assessed causality.
Immunological Assessments
In the phase I study, immunogenicity tests were performed at the central laboratory 360Biolabs (Melbourne VIC, Australia) with validated assays and following laboratory standard operating procedures. Microneutralization assay was applied for NAb testing, with a prototype SARS-CoV-2 hCoV-19/Australia/VIC01/2020 (GenBank MT007544.1) passaged in Vero E6 cells. Sequence analysis of the spike protein showed high sequence homology between SARS-CoV-2 hCoV-19/Australia/VIC01/2020 and Wuhan-Hu-1 strain with only one nucleotide difference (S247R). The first WHO International Standard (Catalog #20/136) was adopted to calibrate its in-house standards and subsequently converted its assay results to international units (IU/mL). RBD- and NTD-specific IgGs were measured with V-Plex SARS-CoV-2 Panel 1 (IgG) Multiplex ELISA (MSD Cat # MESOK15359U-4). Peripheral blood mononuclear cells (PBMCs) were stimulated with PepMix SARS-CoV-2 Spike glycoprotein peptide pool, and CD4+ and CD8+ T cells secreting interleukin (IL)-2, interferon-γ (IFNγ), IL-4, or IL-5 were detected by flow cytometry to assess the T cell immune responses.
In the phase II study, a validated microneutralization assay was implemented for live-virus neutralization at the central laboratory Viroclinics Biosciences, with a SARS-CoV-2 strain which harbors highly homologic sequence to Wuhan-Hu-1 strain. The WHO international standard (Catalog #20/136) was also used to calibrate the NAb titers. To assess the cross-neutralizing activities, NAbs against the prototype, Omicron BA.2 and BA.4/5 were tested via a validated VSV-based pseudovirus neutralization assay, at the central laboratory Gobond Testing Technology (Beijing) Co., Ltd and following laboratory standard operating procedures.
Statistical Analysis
For the phase I study, a sample size of 100 with 25 subjects in each cohort was considered sufficient to provide a descriptive summary of safety and immunogenicity of two dose levels of ReCOV in two age groups. For the phase II study, a sample size of 340, anticipating around 50% of the subjects being seronegative at baseline, was determined to provide more than 99% power to detect a difference in seroconversion rates (SCRs) between 95% and 5% in investigational vaccine and placebo, respectively, when one-side type I error is 0.025.
Continuous variables were summarized using mean or geometric mean with standard deviation, median, minimum, maximum, interquartile range, and coefficient of variance. For categorical variables, frequency and percentage (%) of subjects were presented. The default significance level was 5%, and all confidence intervals (CIs) reported were two-sided 95% CIs, unless otherwise specified in the description of the analyses. Safety analyses were performed in all randomized subjects who received at least one vaccination for the phase I study (safety analysis set), among all randomized subjects who have received at least one vaccination (SS1), and who have received two doses vaccination (SS2) for the phase II study. Immunogenicity analyses were performed in all randomized subjects who have received at least one vaccination and had at least one quantifiable immunogenicity sample collected after vaccination (immunogenicity analysis set, IMM). Chi-square test/Fisher’s exact test was used for statistical test of the differences between groups. Antibody titers were log-transformed before using for calculation of geometric mean titers (GMTs) or geometric mean increase (GMI), and analysis of variance (ANOVA) was performed for statistical test of intergroup differences. The antibody titers reported as below the lower limit of quantification were analyzed using half of the limit value. Titers that were greater than the upper limit of quantification were converted to the upper limit. The SCR was defined as the proportion of subjects with at least fourfold increase in postvaccination antibody titers over baseline. All analyses were conducted using SAS Version 9.4 or higher (SAS Institute).
Results
Trial Population
In both studies, the demographic and baseline clinical characteristics of the subjects were comparable across vaccination groups (Table 1). In the phase I study, the mean age was 31.4 years and 61.3 years among younger and older adults, with a comparable gender distribution in both age groups. Most subjects were White (55.0%) and Asian (35.0%). All 100 subjects except for one in the older group received at least one study vaccination and 98 subjects completed the full vaccination. In the phase II study, 347 subjects were randomized: 66.5% were male, all were Asians of Philippine descent, and the mean age was 31.8 years. About half (51.4%) of the enrolled subjects were SARS-CoV-2 IgM or IgG positive at baseline due to the COVID-19 surge during the enrollment period. All subjects except one received at least one study vaccination and 338 subjects completed the full vaccination. Subjects were followed up regularly throughout the study period, and any individual feeling unwell and/or suspected of being infected with the SARS-CoV-2 virus (presenting with fever, cough, and other respiratory symptoms) was tested for SARS-CoV-2 nucleic acid to confirm infection. No COVID-19-positive individuals were identified. Figure 1 presents flow diagrams for phase I and phase II studies.
Safety Outcomes
In both studies, no vaccination-related SAE, AESI, AE leading to early discontinuation, or clinically significant abnormalities in vital signs or laboratory results related to study vaccination were reported.
In the phase I study, the incidences of AEs were generally higher in ReCOV groups than those in the placebo group (normal saline). In the pooled ReCOV group and placebo group, the incidences of solicited local AEs were 65.0% and 10.0% among younger adults and 69.2% and 10.0% among older adults, respectively; the incidences of solicited systemic AEs were 60.0% and 30.0% among younger adults and 51.3% and 50.0% among older adults, respectively (Fig. 2A, B); the incidences of unsolicited AEs were 65.0% and 20.0% among younger adults and 59.0% and 70.0% in older adults (Table S1 in the supplementary material). Unexpectedly, the incidences of AEs in the 40 μg ReCOV group were remarkably lower in the phase II study than in the phase I study, and appeared to be similar to placebo group (all compositions in ReCOV vaccine except for the antigen): the incidences of solicited local AEs, solicited systemic AEs, and unsolicited AEs were 13.4%, 19.0%, and 7.8% in the ReCOV group and 16.5%, 13.9%, and 8.6% in the placebo group, respectively (Fig. 2C, Table S1).
In the phase I study, although the incidences of solicited local AEs tended to be higher in the 40 μg ReCOV group (younger adults 70.0%, older adults 84.2%) than those in the 20 μg ReCOV group (younger adults 60.0%, older adults 55.0%), the incidences of solicited systemic AEs appeared unrelated to the dose level (Fig. 2), and unsolicited AEs were similar between the two dose level groups (Table S1).
The incidences of solicited AEs after the first and second dosing were compared. In the phase I study, the incidences of solicited AEs after the second dosing tended to be higher than those post the first dosing. In the pooled ReCOV group, the incidences of solicited local and systemic AEs were respectively 48.1% and 21.5% after the first dosing and 58.2% and 49.4% after the second dosing (Fig. 2A, B). However, different data trends in the ReCOV group were observed in the phase II study: the incidences of solicited local and systemic AEs were respectively 10.7% and 13.8% after the first dosing and 5.4% and 8.6% after the second dosing (Fig. 2C).
Consistent common AEs in ReCOV groups were observed in the phase I and phase II studies. In the phase I study, the common (≥ 10%) solicited local AEs were injection site reactions (first dose 48.1%, second dose 58.2%); the common (≥ 10%) solicited systemic AEs were fatigue (first dose 13.9%, second dose 34.2%), myalgia (first dose 6.3%, second dose 30.4%), headache (first dose 8.9%, second dose 27.8%), and pyrexia (first dose 0, second dose 12.7%) (Fig. 2A, B); all solicited AEs in ReCOV groups were transient (median duration 4 days, pooled ReCOV group) and mild in severity, except for one young adult in the 20 µg ReCOV group who developed moderate pyrexia (Tables S2 and S3 in the supplementary material). In the phase II study, the common (≥ 5%) solicited AEs in the ReCOV group were injection site pain (11.6%), headache (8.9%), and pyrexia (8.0%), as shown in Fig. 2C; all solicited AEs were transient (median duration 1.0–4.0 days) and mild or moderate in severity, except for one subject in the ReCOV group who experienced one grade 3 injection site rash and three subjects in the ReCOV group who experienced three grade 3 events of pyrexia (Table S4 in the supplementary material). Similarly, almost all unsolicited AEs were mild to moderate in severity in both studies (Table S1). In the phase I study, the common (≥ 10%) unsolicited AEs in ReCOV groups were upper respiratory tract infection. In the phase II study, no common unsolicited AE was detected in the ReCOV group.
Immunogenicity Outcomes
Robust neutralization against SARS-CoV-2 prototype was consistently shown in ReCOV groups for both phase I and phase II, starting from 21 days post the first dosing, peaked at 14 days post the second dosing, and persisted till the end of the studies, i.e., 6 months post the second dosing. In addition, strong cross-neutralization against the prototype, Omicron BA.2, and BA.4/5 were observed in the phase II study. The phase I study also proved that ReCOV elicited persistent Th1 biased cellular response.
Neutralizing Antibody Response Against SARS-CoV-2 Prototype
In the phase I study, live-virus NAb against the prototype was elicited in most subjects at 21 days after the first dosing of both 20 μg and 40 μg ReCOV, with an SCR of 95.0% and 100% in younger adults and 70.0% and 94.4% in older adults, respectively. After the second ReCOV dosing, the SCR reached 100% at 14 days and remained at this level till the end of the study, i.e., at least 6 months after the dosing, irrespective of dose level and age group. No subject in pooled placebo groups was seropositive at all timepoints tested (Table S5 in the supplementary material). The high seroconversion elicited by 40 μg ReCOV was confirmed in the phase II study. Among subjects seronegative for SARS-CoV-2 IgG/IgM at baseline, a similar population to that in the phase I study, the SCR was significantly higher in the ReCOV group (99.1%) than that in the placebo group (5.8%) at 14 days post the second dosing, and remained at 88.8% in the ReCOV group at the end of the study (Table S6 in the supplementary material).
Both phase I and phase II studies showed that the GMT of live-virus NAb against the prototype reached peak level at 14 days post the second dosing, then decreased over time while remaining at a high level till the end of the studies (Figs. 3 and 4). In the phase I study, high levels of GMTs were demonstrated in both younger and older adults, although the GMTs tended to be lower in older groups as expected. Both 20 μg and 40 μg ReCOV induced high levels of NAb throughout the study period, 40 μg ReCOV tended to elicit higher levels post the first dosing, while 20 μg ReCOV led a stronger response post the second dosing. At 21 days post the first dosing, the GMTs in 20 μg and 40 μg ReCOV groups were 118.0 IU/mL (95% CI 70.5, 197.3) and 135.5 IU/mL (95% CI 88.4, 207.7) among younger adults and 59.0 IU/mL (95% CI 28.5, 122.2) and 78.7 IU/mL (95% CI 47.0, 131.8) among older adults, respectively. The peak GMTs, at 14 days post the second dosing in 20 μg and 40 μg ReCOV groups, were 1643.2 IU/mL (95% CI 1188.5, 2271.9) and 1289.2 IU/mL (95% CI 868.3, 1914.1) among younger adults, with corresponding GMIs of 265.0 and 208.0, while among older adults, the peak GMTs were 1122.3 IU/mL (95% CI 722.6, 1743.1) and 680.3 IU/mL (95% CI 440.2, 1051.4), with corresponding GMIs of 174.9 and 109.7, respectively. At end of the study, 6 months post the second dosing, the GMTs in the two ReCOV groups were still above the level post the first dosing, i.e., 357.6 IU/mL (95% CI 251.1, 509.2) and 293.0 IU/mL (95% CI 168.1, 510.7) among younger adults and 178.8 IU/mL (95% CI 125.6, 254.6) and 268.7 IU/mL (95% CI 131.7, 548.3) among older adults, respectively (Fig. 3).
GMTs of neutralizing antibody against SARS-CoV-2 prototype in the phase I study. The GMTs of neutralizing antibody at baseline, before the second vaccination (21p1), 14 days (14p2), 30 days (30p2), 3 months (3mp2), and 6 months (6mp2) post the second vaccination, respectively, are illustrated for younger adults (A) and older adults (B)
GMTs of neutralizing antibody against SARS-CoV-2 prototype in the phase II study. The GMTs of neutralizing antibody at baseline, 14 days (14p2) and 6 months (6mp2) post the second vaccination are illustrated for the overall study population (Overall), subjects with SARS-CoV-2 seronegative status at baseline (Seronegative), and subjects with SARS-CoV-2 seropositive status at baseline (Seropositive)
The strong and persistent live-virus NAb elicited by ReCOV was further demonstrated in the phase II study (Fig. 4). At baseline, the GMTs were comparable between vaccination groups; however, they were at least 20 times higher in subjects with SARS-CoV-2 seropositive status at baseline (936.0 IU/mL, 95% CI 704.8, 1242.9) than those in subjects with seronegative status at baseline (44.4 IU/mL, 95% CI 34.7, 56.8). At 14 days post the second dosing, the GMTs in ReCOV groups were significantly higher than those in placebo groups, irrespective of serostatus at baseline: in seronegative subjects, the GMTs were 3741.0 IU/mL (95% CI 3113.4, 4495.0) and 41.7 IU/mL (95% CI 30.4, 57.1), with GMIs of 84.3 and 1.1, respectively, while in seropositive subjects, the GMTs were 6138.3 IU/mL (95% CI 5255.1, 7169.9) and 540.3 IU/mL (95% CI 391.0, 746.8), with GMIs of 6.6 and 0.8, respectively (all p values < 0.0001). In the ReCOV group, the NAbs remained at high level at the end of the study, with GMTs of 1094.9 IU/mL (95% CI 894.6, 1340.2) and 1569.8 IU/mL (95% CI 1315.4, 1873.5) in seronegative and seropositive subjects, respectively.
In addition, pseudovirus NAbs against SARS-CoV-2 prototype was also evaluated in the phase II study (Fig. 5), with results consistent with those of the live-virus neutralization. A significant correlation in titers of NAbs measured by live-virus and pseudovirus-based tests was established (Fig. 6), with an overall Pearson’s correlation coefficient of 0.95 (p < 0.0001).
GMTs of pseudovirus neutralizing antibody against SARS-CoV-2 prototype and Omicron variants in the phase II study. The GMTs of pseudovirus NAb against SARS-CoV-2 prototype, Omicron BA.2, and BA.4/5 at baseline, 14 days (14p2) and 6 months (6mp2) post the second vaccination respectively are illustrated for the overall study population (Overall), subjects with SARS-CoV-2 seronegative status at baseline (Seronegative), and subjects with SARS-CoV-2 seropositive status at baseline (Seropositive)
Correlation in titers of neutralizing antibody measured by live-virus and pseudovirus neutralizing antibody tests in the phase II study. The overall Pearson’s correlation coefficient was 0.95 (p < 0.0001), indicating a significant correlation in titers of NAb measured by live-virus and pseudovirus-based methodologies among all tested timepoints, i.e., at baseline, 14 days and 6 months post the second vaccination
Neutralizing Antibody Response Against Omicron Variants
Pseudovirus NAbs against the prototype, Omicron BA.2, and BA.4/5 were evaluated in the phase II study. Among seronegative subjects at baseline, the SCRs for Omicron BA.2 and BA.4/5 were 91.7% and 91.7% with GMIs of 56.3 and 59.9, respectively, in the ReCOV group, while in the placebo group, the SCRs were 11.5% and 11.5% with GMIs of 1.3 and 1.3, respectively. Among seropositive subjects at baseline, the SCRs for Omicron BA.2 and BA.4/5 were 50.5% and 58.6% with GMIs of 6.3 and 6.1 in the ReCOV group and 11.7% and 10.0% with GMIs of 1.0 and 0.8 in the placebo group, respectively (Table S6).
At baseline, the GMTs for both Omicron strains were similar between vaccination groups, but were around 15–20 times higher in seropositive subjects than those in seronegative subjects, as shown in Fig. 5. At 14 days post the second dosing, the levels of NAb against both Omicron strains in ReCOV groups were significantly higher than those in placebo groups, irrespective of serostatus at baseline. Among seronegative subjects, the GMTs against the prototype, BA.2, and BA.4/5 were 8856.6 (95% CI 7136.7, 10,991.1), 4441.0 (95% CI 3348.8, 5889.4), and 2644.3 (95% CI 1990.4, 3513.0) in the ReCOV group and 88.6 (95% CI 57.1, 137.2), 76.8 (95% CI 43.7, 134.8), and 43.0 (95% CI 25.6, 72.2) in the placebo group, respectively; among seropositive subjects, the GMTs were 15,667.3 (95% CI 13,511.5, 18,167.0), 7334.3 (95% CI 6160.1, 8732.4), and 4478.8 (95% CI 3829.8, 5237.9) in the ReCOV group and 1548.0 (95% CI 1067.0, 2245.9), 968.4 (95% CI 653.2, 1435.7), and 526.0 (95% CI 357.7, 773.5) in the placebo group, respectively (all p values < 0.0001) (Table S6). Among subjects receiving ReCOV, the GMTs were only around 2.1-fold lower for BA.2 and around 3.5-fold lower for BA.4/5, comparing to the levels for the prototype, irrespective of serostatus at baseline (Fig. 5). Consistent with the results of the prototype, at 6 months post the second dosing, the GMTs against Omicron BA.2 and BA.4/5 remained at high levels in the ReCOV group, i.e., 1447.2 (95% CI 1120.98, 1868.39) and 1052.6 (95% CI 828.6, 1337.3), respectively, among seronegative subjects and 1474.9 (95% CI 1227.1, 1772.7) and 985.9 (95% CI 829.2, 1172.3), respectively, among seropositive subjects, only 2.5-fold to 5.2-fold lower compared to the corresponding peak levels at 14 days post the second dosing (Fig. 5, Table S6).
Spike RBD- and NTD-Specific IgGs
In the phase I study, consistently low levels of RBD- and NTD-specific IgGs were observed in all study groups at baseline. Comparable peak GMTs of RBD- and NTD-specific IgGs were shown in 20 μg and 40 μg ReCOV groups, irrespective of age groups. Among older adults, the peak GMTs tended to be 1.3–1.7 times lower compared to that among younger adults; however, the antibody levels were still high and persisted throughout all testing timepoints tested. In 20 μg and 40 μg ReCOV groups, the peak GMTs of RBD- and NTD-specific IgGs were 278,596.1 AU/mL (95% CI 206,532.0, 375,805.1) and 11,232.4 AU/mL (95% CI 8273.6, 15,249.4) in the 20 μg ReCOV group and 271,838.2 AU/mL (95% CI 216471.5, 341,366.0) and 11,266.5 AU/mL (95% CI 8420.5, 15,074.4) in the 40 μg ReCOV group among younger adults, while they were 185,337.6 AU/mL (95% CI 136,635.2, 251,399.5) and 9422.8 AU/mL (95% CI 6846.1, 12,969.3) in the 20 μg ReCOV group and 203,829.7 AU/mL (95% CI 145,482.5, 285,577.6) and 6705.9 AU/mL (95% CI 4657.3, 9655.6) in the 40 μg ReCOV group among older groups, respectively. At 6 months post the second dosing, the GMTs of RBD- and NTD-specific IgGs were still above the level of post the first dosing, irrespective of dose levels and age groups (Fig. 7).
GMTs of SARS-CoV-2 Spike RBD- and NTD-specific IgG in the phase I study. The GMTs of SARS-CoV-2 Spike RBD- and NTD-specific IgG at baseline, before the second vaccination (21p1), 14 days (14p2), 30 days (30p2), 3 months (3mp2), and 6 months (6mp2) post the second vaccination are illustrated for the pooled placebo group, 20 µg ReCOV group, and 40 µg ReCOV group
Cellular Immune Responses
The cellular immune response was evaluated in the phase I study. At baseline, very low levels (≤ 0.06%) in average percentage of CD4+ T cells secreting antigen-specific IL-2 or IFNγ were observed at baseline among all study groups. In younger subjects, the average percentage of CD4+ T cells with IL-2 or IFNγ secretion increased to 0.3% (20 μg ReCOV) and 0.2% (40 μg ReCOV) at 14 days post second dosing and remained at 0.2% (20 μg ReCOV) and 0.1% (40 μg ReCOV) at 6 months post the second dosing, while in older subjects, the level increased to 0.2% (20 μg ReCOV) and 0.2% (40 μg ReCOV) at 14 days post second dosing and remained at 0.2% (20 μg ReCOV) and 0.16% (40 μg ReCOV) at 3 months post the second dosing. In placebo groups, the average percentage of CD4+ T cells secreting antigen-specific IL-2 or IFNγ remained at low levels at all timepoints tested. The peak cellular responses among older adults tended to be lower than that among younger adults.
In contrast to the Th1 biased cellular immune responses, no obvious increase in Th2 cytokine (IL-4 or IL-5) secretions was observed in both age groups receiving 20 μg and 40 μg ReCOV (Fig. 8). In addition, no obvious CD8+ T cell responses were observed across age groups and dose levels (data not shown).
Th1 and Th2 cytokine responses in the phase I study. The observation was considered as an outlier if the value was less than 1.5 × interquartile range (IQR) below Q1 or greater than 1.5 × IQR above Q3. Data show the percentage of CD4+ T cells for Th1 (IL-2 or IFNγ) and Th2 (IL-4 or IL-5) cell responses at baseline, 14 days (14p2), 30 days (30p2), 3 months (3mp2), and 6 months (6mp2) post the second vaccination of pooled placebo group, 20 µg ReCOV group, and 40 µg ReCOV group
Discussion
Both 20 μg (for phase I only) and 40 μg ReCOV were proven to be well tolerated with a good safety profile in Caucasian and Asian adults, when used as a primary vaccination series of two intramuscular injections with a 21-day interval. No vaccination-related SAE, AESI, or AE leading to early discontinuation were reported. The incidences of solicited local and systemic AEs and unsolicited AEs in the pooled ReCOV group were 65.0%, 60.0%, and 65.0% among younger adults and were 69.2%, 51.3%, and 59.0% among older adults, respectively, which were higher than those in the pooled placebo group. In the phase II study, the incidences of solicited local and systemic AEs and unsolicited AEs were 13.4%, 19.0%, and 7.8% in the ReCOV group, respectively. All solicited AEs were mild except for one moderate pyrexia in the phase I study, and the majority of solicited AEs were mild or moderate in the phase II study. In the phase I study, the NAb against prototype was elicited by any dose level of ReCOV at 21 days post the first dosing and peaked at 14 days post dosing. In the phase II study, a strong neutralization against the prototype was also elicited by 40 μg ReCOV among subjects with SARS-CoV-2 seronegative and seropositive status at baseline. High levels of NAb against the prototype remained till the end of the studies. In addition, obvious responses in NAbs against the prototype, Omicron BA.2, and BA.4/5 were shown in the 40 μg ReCOV group at 14 days post the second dosing. The NAbs against BA.2 and BA.4/5 only showed around 2.5- to 5.2-fold decreases compared to the peak levels till the end of the study. Besides, Th1 biased cytokine secretion was detected in ReCOV groups in the phase I study, with increased CD4+ T cells with IFNγ or IL-2 secretions observed.
In the phase I study, consistent safety characteristics were reported between two dose levels of ReCOV and between younger and older adults. The incidences of solicited AEs after the second dosing tended to be higher than those post the first dosing. Less frequent AEs were reported in the phase II study compared with the phase I study, likely due to different tolerance between study populations, as the same safety data collection rules and quality controls were implemented in both studies. Nevertheless, most of the solicited and vaccination-related unsolicited AEs were transient and mild or moderate in severity in both studies (only one moderate pyrexia developed in phase I, one injection site rash and three pyrexia reported as grade 3 in phase II), and all solicited AEs were transient and recovered within a few days in both studies. No vaccination-related SAE, AESI, AE leading to early discontinuation or clinically significant abnormalities in vital signs and laboratory results related to study vaccination were reported.
ReCOV is adjuvanted with BFA03, which has the same formulation as AS03 adjuvant. AS03 has been widely used globally with a good safety profile in approved and investigated vaccines against H1N1 and H5N1 pandemics. By 2019, 90 million people had been vaccinated with influenza vaccines containing AS03 adjuvant, including 9 million infants and 300,000 pregnant women [9]. AS03 has also been used in the development of COVID-19 vaccines, i.e., CoV2 preS dTM, which is a recombinant protein vaccine co-developed by Sanofi and GlaxoSmithKline, and CoVLP, which is a virus-like particle vaccine produced from a plant co-developed by Medicago and GlaxoSmithKline. Both CoV2 preS dTM and CoVLP showed acceptable safety and reactogenicity in clinical trials, with similar characteristics in adverse events as current ReCOV studies. In the phase II study of CoV2 preS dTM with three study dose levels [10], the adverse reactions were transient, were mostly mild to moderate in severity, and developed at a higher frequency and intensity after the second vaccination as observed with ReCOV in the current phase I study. In the phase II study of CoVLP [11], only 1.5% and 6.3% participants reported grade 3 solicited AEs after the first and second dosing, respectively, and in its phase III study, both local and systemic solicited AEs were also predominantly mild-to-moderate and transient. The results from current phase I and phase II studies, in alignment with AS03-adjuvated influenza and COVID-19 vaccines, supported the notion that BFA03-adjuvated ReCOV has a good safety profile and can be extended to larger-scale populations.
The robust and persistent neutralization elicited by ReCOV was demonstrated in the current two studies. The NAb against SARS-CoV-2 prototype was elicited in most subjects at 21 days after the first vaccination, reached the peak level at 14 days post the second vaccination, then decreased overtime but remained at high level at 6 months post the second vaccination. In the phase I study, high levels of GMTs were demonstrated in both younger and older adults, although the GMTs tended to be lower in older groups as expected. The higher dose (40 μg) ReCOV tended to elicit an earlier response while the lower dose (20 μg) ReCOV led to a higher level of response through the end of the study, suggesting the dose level in clinical use requires further confirmation. The quick, strong, and persistent humoral responses induced by ReCOV were supported by the consistent results for both RBD- and NTD-specific IgGs in the phase I study.
Humoral responses, especially NAbs, have been considered as immune correlates of protection against SARS-CoV-2 [12]. Considering the diversity in laboratory testing methodologies and lack of head-to-head clinical trials, the NAbs measured in the current phase I and phase II studies were calibrated by WHO international standard which allowed the conversion of the assay results to international units (IU/mL). This enabled comparison of the results in current studies with the data from other vaccines at a certain level. ReCOV elicited strong neutralization against the prototype with at least a similar or even higher level than several COVID-19 vaccines with proven promising efficacies. The peak GMTs for the prototype were 1122.3–1643.2 IU/mL in the phase I study and 3741.0 IU/mL and 6138.3 IU/mL among subjects with SARS-CoV-2 seronegative and seropositive status at baseline in the phase II study, respectively. In reported clinical studies, the peak GMTs for the two recombinant protein vaccines were reported as 224 IU/mL (SCB-2019 [13], a protein subunit vaccine candidate containing a stabilized trimeric form of S-protein Trimer combined with CpG 1018 and aluminum hydroxide) and 408 IU/mL (MVC-COV1901 [14], a recombinant protein vaccine containing pre-fusion-stabilized Spike protein S-2P adjuvanted with CpG 1018 and aluminum hydroxide), respectively, while for the mRNA vaccines they were 1404.16 IU/mL (mRNA-1273) and 928.75 IU/mL (BNT162b2), respectively [15]. In addition to the aforementioned comparison based on published data, the robust immunogenicity of ReCOV was confirmed in the head-to-head phase II study for booster vaccination, where ReCOV demonstrated comparable or stronger neutralizing activities than BNT162b2, against the prototype and multiple Omicron variants (manuscript in preparation).
With the emergence of mutated strains, especially the Omicron variants, the prototype-based vaccines were challenged in terms of their cross-strain immunogenicity and effectiveness. Unlike vaccines containing only RBD or the full length of Spike sequences, ReCOV contains NTD and RBD but without S2 of Spike. NTD and RBD have been confirmed as containing more neutralizing epitopes, while S2 contains few neutralizing antibody epitopes. ReCOV also combines the NTD-RBD sequence with the foldon sequence of phage T4 to form a trimer structure, ensuring the antigen structure is more like the natural trimer of SARS-CoV-2. The immunogenicity of ReCOV can be further enhanced and persisted by adjuvating with BFA03, which was also mentioned in the publication for AS03 adjuvant of H5N1 influenza vaccine [16]. Therefore, although the sequence is from Wuhan-Hu-1 strain, ReCOV is expected to elicit cross-neutralization against SARS-CoV-2 variants. In the phase II study, ReCOV demonstrated strong cross-neutralizing activities for the prototype and Omicron variants including BA.2 and BA.4/5. At 14 days post ReCOV vaccinations, only 2.0-fold and 3.5-fold reductions in the GMTs of NAbs against Omicron BA.2 and BA.4/5, respectively, were observed compared to the that against the prototype. These reductions were much less significant than those reported from primary vaccination studies with other COVID-19 vaccines, i.e., around 20–40-fold reductions in NAbs against Omicron variants versus the prototype for NVX-CoV2373 (41-fold and 30-fold reduction for Omicron BA.1 and BA.4/5, respectively) [17], ZF2001 (13.2-fold and 31.6-fold reduction for Omicron BA.2 and BA.4/5, respectively) [18], and BNT162b2 (31-fold reduction for Omicron variant) [19]. The data from current phase II study, together with phase II studies for ReCOV booster vaccination (manuscript in preparation), proved the concept that with the trimeric RBD-NTD-foldon structure and in combination with a potent adjuvant, ReCOV can elicit a strong and broad spectrum of neutralizing activities and has high potential to combat emergent SARS-CoV-2 strains including Omicron variants.
In addition to constant emergence of SARS-CoV-2 variants, breakthrough infections could be affected by the waning of vaccine-induced immunity. The current studies consistently showed that ReCOV-induced NAbs could persist till at least 6 months post the second vaccination. In the phase I study, the SCRs of neutralizing antibodies remained at 100% at study end, irrespective of dose levels and age groups. In the phase II study, the NAbs against the prototype, Omicron BA.2, and BA.4/5 reduced only around threefold to sixfold at the end of the study, compared to the peak values. The data in current studies indicated a longer immune persistence of ReCOV than other protein vaccines, e.g., the GMTs declined about 24.3-fold and 7.7-fold for a SARS-CoV-2 recombinant Spike protein nanoparticle vaccine (NVX-CoV2373) and a recombinant SARS-CoV-2 fusion protein Vaccine (V-01), respectively, at 6 to 8 months post the second dosing compared to the peak levels [20]. The good immune persistence, together with the high level of NAbs, further supports the continuous development of ReCOV especially in this Omicron era.
In the phase I study, Th1 biased cellular immune responses were observed for both 20 μg and 40 μg ReCOV, indicated by increased frequencies of CD4+ T cells with INFγ and/or IL-2 secretion at 14 days post the second dosing, and remained at almost the same level up to 6 months in younger subjects and 3 months in older subjects, while no obvious secretion of Th2 cytokines (IL-4 and IL-5) was detected. Th1 cytokines are important for development of T cell responses, and CD4+ T cell is required for good induction of memory B cells. A similar trend of Th1 biased cellular immune responses has also been reported in studies on mRNA-1273 [21] and BNT162b2 [22]. Notably, such a Th1 biased immune response is desirable for the development of a SARS-CoV-2 vaccine because of the hypothetical concern for immune-mediated disease enhancement observed in preclinical studies for other coronaviruses.
There were a few limitations in the current paper: first, both phase I and phase II studies adopted ReCOV with primary vaccination series, which may only be applicable in populations with limited vaccine accessibility. Second, the comparisons of immunogenicity with other COVID-19 vaccines were mainly based on literature review and no results with head-to-head comparison studies were included. Third, only NAbs against Omicron BA.2 and BA.4/5 were assessed for cross-neutralization. Fourth, no efficacy results could be reflected in both studies. Currently, two phase II studies (NCT05323435, NCT05084989) of the adopted booster vaccination series, to directly compare ReCOV with inactivated and mRNA vaccines, respectively, have demonstrated robust and persistent immunogenicity against the prototype and Omicron epidemic strains; the manuscript to report the results is under preparation. In addition, the efficacy results of ReCOV phase III study (NCT05398848) will be presented soon.
Conclusion
Both 20 µg and 40 µg ReCOV demonstrated good safety and robust and persistent immunogenicity in the phase I and phase II studies for the primary vaccination series. ReCOV could elicit strong cross-neutralization against Omicron variants tested as well. The data strongly support the further development of ReCOV in large-scale efficacy trials.
Data Availability
All data generated or analyzed during this study are included in this published article/as supplementary information files.
References
World Health Organization. WHO Coronavirus Disease (COVID-19) Dashboard. https://covid19.who.int/. Accessed 30 May 2023.
Zhang Y, Zhang W. 2019 novel coronavirus variants: current status, trends and countermeasures. Chin J Infect Dis. 2021;39(6):321–4.
Goldberg Y, Mandel M, Bar-On YM, et al. Waning immunity after the BNT162b2 vaccine in Israel. N Engl J Med. 2021;385(24):e85. https://doi.org/10.1056/NEJMoa2114228.
Keehner J, Horton LE, Binkin NJ, et al. Resurgence of SARS-CoV-2 infection in a highly vaccinated health system workforce. N Engl J Med. 2021;385(14):1330–2. https://doi.org/10.1056/NEJMc2112981.
Zhang L, Cao L, Gao XS, et al. A proof of concept for neutralizing antibody-guided vaccine design against SARS-CoV-2. Natl Sci Rev. 2021;8(8):nwab053. https://doi.org/10.1093/nsr/nwab053.
Yu J, Yao W, Hu Y, et al. A trimeric NTD and RBD SARS-CoV-2 subunit vaccine induced protective immunity in CAG-hACE2 transgenic mice and rhesus macaques. bioRxiv. 2021:2021.11.03.467182. https://doi.org/10.1101/2021.11.03.467182.
Law B, Sturkenboom M. Safety platform for emergency vaccines-d2.3 priority list of adverse events of special interest: COVID-19. https://www.regione.marche.it/portals/3/farmaceutica/SPEAC_D2.3_V2.0_COVID-19_20200525_public.pdf. Accessed 20 June 2023
FDA. Food and drug administration guidance document: toxicity grading scale for healthy adult and adolescent volunteers enrolled in preventive vaccine clinical trials. https://www.fda.gov/regulatory-information/search-fda-guidance-documents/toxicitygrading-scale-healthy-adult-and-adolescent-volunteers-enrolled-preventive-vaccine-clinical. Accessed 25 June 2023.
Cohet C, van der Most R, Bauchau V, et al. Safety of AS03-adjuvanted influenza vaccines: a review of the evidence. Vaccine. 2019;37(23):3006–21. https://doi.org/10.1016/j.vaccine.2019.04.048.
Sridhar S, Joaquin A, Bonaparte MI, et al. Safety and immunogenicity of an AS03-adjuvanted SARS-CoV-2 recombinant protein vaccine (CoV2 preS dTM) in healthy adults: interim findings from a phase 2, randomised, dose-finding, multicentre study. Lancet Infect Dis. 2022;22(5):636–48. https://doi.org/10.1016/s1473-3099(21)00764-7.
Charland N, Gobeil P, Pillet S, et al. Safety and immunogenicity of an AS03-adjuvanted plant-based SARS-CoV-2 vaccine in adults with and without comorbidities. NPJ Vaccines. 2022;7(1):142. https://doi.org/10.1038/s41541-022-00561-2.
Dai L, Gao GF. Viral targets for vaccines against COVID-19. Nat Rev Immunol. 2021;21(2):73–82. https://doi.org/10.1038/s41577-020-00480-0.
Richmond P, Hatchuel L, Dong M, et al. Safety and immunogenicity of S-Trimer (SCB-2019), a protein subunit vaccine candidate for COVID-19 in healthy adults: a phase 1, randomised, double-blind, placebo-controlled trial. Lancet. 2021;397(10275):682–94. https://doi.org/10.1016/s0140-6736(21)00241-5.
Hsieh SM, Liu MC, Chen YH, et al. Safety and immunogenicity of CpG 1018 and aluminium hydroxide-adjuvanted SARS-CoV-2 S-2P protein vaccine MVC-COV1901: interim results of a large-scale, double-blind, randomised, placebo-controlled phase 2 trial in Taiwan. Lancet Respir Med. 2021;9(12):1396–406. https://doi.org/10.1016/s2213-2600(21)00402-1.
Kung Y-A, Huang C-G, Huang S-Y, et al. Antibody titers measured by commercial assays are correlated with neutralizing antibody titers calibrated by international standards. medRxiv. 2021:2021.07.16.21260618. https://doi.org/10.1101/2021.07.16.21260618.
Shi S, Zhu H, Xia X, Liang Z, Ma X, Sun B. Vaccine adjuvants: understanding the structure and mechanism of adjuvanticity. Vaccine. 2019;37(24):3167–78. https://doi.org/10.1016/j.vaccine.2019.04.055.
Bhiman JN, Richardson SI, Lambson BE, et al. Novavax NVX-COV2373 triggers neutralization of Omicron sub-lineages. Sci Rep. 2023;13(1):1222. https://doi.org/10.1038/s41598-023-27698-x.
Zhao X, Zhang R, Qiao S, et al. Omicron SARS-CoV-2 neutralization from inactivated and ZF2001 vaccines. N Engl J Med. 2022;387(3):277–80. https://doi.org/10.1056/NEJMc2206900.
Cheng SMS, Mok CKP, Leung YWY, et al. Neutralizing antibodies against the SARS-CoV-2 Omicron variant BA.1 following homologous and heterologous CoronaVac or BNT162b2 vaccination. Nat Med. 2022;28(3):486–9. https://doi.org/10.1038/s41591-022-01704-7.
Chen X, Wang W, Chen X, et al. Prediction of long-term kinetics of vaccine-elicited neutralizing antibody and time-varying vaccine-specific efficacy against the SARS-CoV-2 Delta variant by clinical endpoint. BMC Med. 2022;20(1):36. https://doi.org/10.1186/s12916-022-02249-9.
Jacqueline M. Miller MD FAAP. mRNA-1273 clinical development program. https://www.cdc.gov/vaccines/acip/meetings/downloads/slides-2020-08/COVID-02-Miller-508.pdf. Accessed Aug 26, 2020.
Sahin U, Muik A, Vogler I, et al. BNT162b2 vaccine induces neutralizing antibodies and poly-specific T cells in humans. Nature. 2021;595(7868):572–7. https://doi.org/10.1038/s41586-021-03653-6.
Acknowledgements
This work was supported by the National Natural Science Foundation of China (number 82173584 and 82222062), Jiangsu Provincial Science Fund for Distinguished Young Scholars (number BK20220064), and Jiangsu Provincial Key Project of Science and Technology Plan (number BE2021738).
Funding
Jiangsu Recbio Technology Co., Ltd funded this study.The journal’s Rapid Service fee was funded by the study sponsor.
Author information
Authors and Affiliations
Contributions
Chris Wynne and Paul Hamilton are the principal investigators of ReCOV phase I study. Abundio Balgos is the principal investigator of the phase II study. Jing-Xin Li, Jian-Hui Zhang, and Chen Mo contributed to clinical development plan and key design of study protocols for ReCOV. Zijing Yue and Ying Ma are medical leads for both studies. Chen Mo and Jian-Hui Zhang drafted of the manuscript. Qing-Shuang Wang and Ren-Du Wen are project leads for both studies. Zheng Yao is the statistician taking charge of data statistical analysis for both studies. Jian-Hui Zhang, Hui Zheng, Jing-Xin Li, and Kun-Xue Hong contributed to critical review and revising of the manuscript. Jian-Hui Zhang, Yong Liu, Jing-Xin Li and Feng-Cai Zhu contributed to study supervision. Jia-Ping Yu and Wen-Rong Yao contributed to the design of the investigational vaccine. All authors reviewed and approved the final manuscript.
Corresponding authors
Ethics declarations
Conflict of Interest
Chen Mo, Zijing Yue, Ying Ma, Qing-Shuang Wang, Ren-Du Wen, Zheng Yao, Jia-Ping Yu, Wen-Rong Yao, Jian-Hui Zhang, Kun-Xue Hong, Yong Liu are employees of Jiangsu Recbio Technology Co., Ltd. All the other authors declare no competing interests.
Ethical Approval
For the phase 1 study, the study protocol and informed consent were approved by the Ethics Committee of the New Zealand Clinical Research. For the phase 2 study, the study protocol and informed consent were approved by the Ethics Committee of St. Paul’s Hospital, the Medical City Iloilo and the Health Centrum in Philippines. Informed consent was obtained from each subject before any study procedures were performed.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License, which permits any non-commercial use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc/4.0/.
About this article
Cite this article
Wynne, C., Balgos, A., Li, J. et al. Safety and Immunogenicity of a Recombinant Two-Component SARS-CoV-2 Protein Vaccine: Randomized, Double-Blind, Placebo-Controlled Phase I and Phase II Studies. Infect Dis Ther 13, 57–78 (2024). https://doi.org/10.1007/s40121-023-00896-w
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s40121-023-00896-w