Abstract
Purpose
We aimed to explore the prevalence and within-host evolution of resistance in polymyxin-heteroresistant carbapenem-resistant Klebsiella pneumoniae (PHR-CRKP) in critically ill patients.
Methods
We performed an epidemiological analysis of consecutive patients with PHR-CRKP from clinical cases. Our study investigated the within-host resistance evolution and its clinical significance during polymyxin exposure. Furthermore, we explored the mechanisms underlying the dynamic evolution of polymyxin resistance at both subpopulation and genetic levels, involved population analysis profile test, time-killing assays, competition experiments, and sanger sequencing. Additionally, comparative genomic analysis was performed on 713 carbapenemase-producing K. pneumoniae strains.
Results
We enrolled 109 consecutive patients, and PHR-CRKP was found in 69.7% of patients without previous polymyxin exposure. 38.1% of PHR-CRKP isolates exhibited polymyxin resistance and led to therapeutic failure in critically ill scenarios. An increased frequency of resistant subpopulations was detected during PHR-CRKP evolution, with rapid regrowth of resistant subpopulations under high polymyxin concentrations, and a fitness cost in an antibiotic-free environment. Mechanistic analysis revealed that diverse mgrB insertions and pmrB hypermutations contributed to the dynamic changes in polymyxin susceptibility in dominant resistant subpopulations during PHR evolution, which were validated by comparative genomic analysis. Several deleterious mutations (e.g. pmrBLeu82Arg, pmrBSer85Arg) were firstly detected during PHR-CRKP evolution. Indeed, specific sequence types of K. pneumoniae demonstrated unique deletions and deleterious mutations.
Conclusions
Our study emphasizes the high prevalence of pre-existing heteroresistance in CRKP, which can lead to polymyxin resistance and fatal outcomes. Hence, it is essential to continuously monitor and observe the treatment response to polymyxins in appropriate critically ill scenarios.
Graphical Abstract

Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Carbapenem-resistant Klebsiella pneumoniae (CRKP) poses a significant global threat to clinical settings [1]. Polymyxins, such as polymyxin B (PMB) and colistin, are considered the last resort for combating CRKP infections in cases of sepsis [2, 3]. However, the clinical effectiveness of polymyxins in critically ill patients has been questioned because of the emergence of polymyxin resistance and heteroresistance [4, 5]. Heteroresistance refers to the presence of subpopulations with resistance traits within clinically identified non-resistant pathogens, and these heteroresistant isolates can rapidly replicate in the presence of antibiotics [6, 7]. Therefore, providing clinical evidence to support the prudent utilization of polymyxins is crucial.
Currently, there is a pressing need for clinical studies on the epidemiology of, risk factors for, and clinical significance of polymyxin-heteroresistant (PHR)-CRKP and on the dynamic surveillance of PHR infections during antimicrobial therapy, especially among immunosuppressed and critically ill patients [5, 7]. The prevalence of PHR-CRKP isolates varies significantly from 8.4 to 100% in different studies [5, 8,9,10,11,12]. Polymyxin heteroresistance is often underestimated because conventional minimum inhibitory concentration (MIC) testing methods are unable to detect heteroresistant (HR) and implementing the ‘gold standard’ population analysis profile (PAP) test in clinical settings can be challenging [6, 13]. Prior polymyxin exposure may induce polymyxin heteroresistance [14]. Concerningly, several PHR- and polymyxin-resistant (PR)-CRKP isolates have been identified in patients without prior antibiotic exposure [5, 15,16,17]. Furthermore, polymyxin heteroresistance in Enterobacterales has been implicated in treatment failure and affecting treatment outcomes in animal infection models [18]. However, clinical evidence concerning the contribution of polymyxin heteroresistance to polymyxin treatment failure remains limited in clinical practice [5, 7, 17].
Various chromosomal mechanisms are major contributors to polymyxin heteroresistance, including mutations in key genes, such as mgrB, pmrAB, crrAB, and phoPQ in K. pneumoniae, which affect lipopolysaccharide modifications [17, 19, 20]. Polymyxin heteroresistance can also be driven by spontaneous amplification and increased expression of resistance-related genes [21]. Interestingly, the resistant phenotype can revert to susceptible in the absence of antibiotics due to gene amplification instability or a reduction in fitness cost due to genetically stable mutations in animal infection models [18]. However, the exact mechanisms underlying this heterogeneity remain unclear and require further investigation in clinical practice. In addition, the relationship between genetic background and HR remains to be explored [8].
In this study, we investigated the prevalence of PHR-CRKP, its in vivo evolution, and its clinical importance during polymyxin exposure within critically ill scenarios. Next, we explored the mechanisms underlying the dynamic evolution of polymyxin resistance at both subpopulation and genetic levels. Additionally, we analyzed carbapenemase-producing K. pneumoniae strains from the National Center for Biotechnology Information (NCBI) database to explore the mutational diversity of canonical genes associated with polymyxin heteroresistance in different genetic backgrounds.
Materials and methods
Study design
From 1 April to 31 October 2020, we conducted a prospective and consecutive microbiological follow-up study of CRKP cases at Ruijin Hospital, Shanghai Jiao Tong University School of Medicine, Shanghai, China. Our objectives were to assess the prevalence of PHR-CRKP isolates, investigate the changes in susceptibility to polymyxin during the treatment, and understand its underlying evolutionary process in clinical practice.
First, we enrolled 109 consecutive patients with polymyxin-intermediate (PI)-CRKP. Polymyxin susceptibility testing was performed using the VITEK 2 Compact system (bioMérieux) in clinical laboratory [22].The result was further verified by colistin agar test and manual broth microdilution method, as recommended by the Clinical and Laboratory Standards Institute (CLSI) M100 Ed30 [23]. The breakpoint determination for polymyxin was interpreted according to the latest standards of CLSI M100 Ed30 [23]. The prevalence of polymyxin heteroresistance in their initial isolates was determined using a PAP test [6, 20]. Among the 21 patients receiving polymyxin treatment, we further examined eight sepsis patients (A–H) with the dynamic changes in polymyxin susceptibility in the subsequent predominant K. pneumoniae subpopulations and evaluated their clinical outcomes (Table S1).The HR phenotype was limited to PI-CRKP isolates, which are defined based on detectable resistant subpopulations that can grow in the presence of > 2 mg/L colistin on Mueller–Hinton agar plates [6, 20].
Second, we investigated the mechanism of in vivo evolution of PHR-CRKP as follows: (i) At the subpopulation level, we performed the PAP test to monitored the frequency of resistant subpopulations in HR isolates collected before the emergence of polymyxin resistance in patients A, B, and C. Additionally, we conducted time-killing studies, subculture experiments, and competition assays in these isolates in the presence and absence of polymyxin [24,25,26]. (ii) At the genetic level, we selected pairs of strains, including a subsequent PR-CRKP strain and its heteroresistant ancestor, from each patient and sequenced PR canonical genes (phoPQ, pmrAB, crrAB, and mgrB) using Sanger sequencing (Table S2). We also analyzed all continuously obtained strains from patients C and G to gain insights into the dynamics of polymyxin resistance in the predominant PHR-CRKP subpopulations during long-term polymyxin therapy. Quantitative reverse transcription polymerase chain reaction (qRT-PCR) was used to assess the contributions of coexisting mutations requiring further experimental evaluation [27].
Finally, we performed a comprehensive analysis of the publicly available complete genomes of carbapenemase-producing K. pneumoniae from the NCBI database to determine the genetic background and variability of canonical genes associated with polymyxin heteroresistance and resistance.
Please refer to the Supplementary materials for a detailed description of the methods used.
Statistical analyses
The clinical characteristics and outcome analysis were performed in SPSS version 26. Chi-squared and Fisher’s exact tests were used for categorical variables, and Mann-Whitney U-tests were used for continuous variables. The results from the time-killing study, competition assay, and qRT-PCR experiments are presented as means ± standard deviations. Charts for the PAP test, time-killing study, and competition assay were generated using the Origin version 2018 software (Origin Lab). Statistical analysis of the qRT-PCR data was performed using Student’s t-test using GraphPad Prism version 6.
Ethical approval
The Ethics Committee of Ruijin Hospital, School of Medicine, Shanghai Jiao Tong University (RJ2019NO1-3) reviewed and approved the study. Personally identifiable information was removed prior to the analysis, and the requirement for informed consent was waived.
Results
Prevalence of PHR-CRKP and dynamic changes in clinical isolates
Out of the consecutive 109 patients carried PI-CRKP isolates, 76 (69.7%) showed polymyxin heteroresistance (Fig. 1). Among these patients with PHR-CRKP, only two had previous polymyxin exposure and 21 received polymyxin treatment. Interestingly, eight (38.1%) of these patients subsequently exhibited PR-CRKP during or after the treatment. In contrast, in the non-heteroresistant group, none of the patients had a history of polymyxin exposure. In subset of non-PHR group, no PR-CRKP strains were identified, although four patients received polymyxin treatment during their hospital stay.
Clinical characteristics and dynamic evolution of polymyxin resistance in patients with clinical PHR-CRKP infection
Table S1 shows the clinical characteristics of 21 patients receiving polymyxin treatment, of there eight critically ill sepsis patients (A–H) with multiple organ dysfunction syndrome subsequently exhibited polymyxin resistance. These 8 patients received longer courses of polymyxin treatment compared to the remaining 13 patients who did not exhibit resistance (median 23 versus 13, p = 0.076). A total of 54 clinical K. pneumoniae isolates obtained from patients A-H were available for further analysis according to Pulse-field gel electrophoresis results (PFGE) results (Figure S1). Figure 2 provides a comprehensive timeline of the clinical samples, isolated strains, dynamic susceptibility of CRKP strains to polymyxins, antimicrobial treatments, and clinical outcomes.In patients A, C, D, E, and H, polymyxins were administered in combination with in vitro-active tigecycline (TGC) or ceftazidime/avibactam (CZA) for clinically diagnosed PI-CRKP infections.Patients A and C received low-dose polymyxin regimens according to the recommended treatment guidelines [28]. Prior to polymyxin treatment, patient C developed acute renal failure and received continuous renal replacement therapy (CRRT). Throughout the course of polymyxin therapy, patients A, B, D, E, G, and H experienced deteriorating renal function, and patient E required CRRT. However, after a short duration of polymyxin-based treatment (median, 11 days), all eight patients subsequently had PR-CRKP infections and treatment failure. Notably, patients A and B showed improvement in infection symptoms when switched to CZA, and the PI-CRKP strains were detected after discontinuing polymyxin B for 49 and 18 days, respectively. However, the remaining six patients continued to present persistent PR-CRKP infections and unfortunately experienced fatal outcomes despite attempts to switch to in vitro active antibiotic therapies, including CZA.
The evolving polymyxin resistance in a series of PHR-CRKP isolates collected from eight sepsis patients. The timeline of clinical samples, isolated strains, MIC, antimicrobial treatment, and clinical outcomes was described for 54 strains included in the analysis. PFGE results indicate clonal homogeneity among isolates from each patient, as shown in Figure S1. Different clinical samples are color-coded, with red highlighting antimicrobial treatments involving polymyxins. The MICs of the original heteroresistant isolates and resistant subpopulations are indicated in black and red, respectively. The clinical prognosis of death or improvement after discharge is also shown in the figure. Abbreviations: PHR-CRKP, polymyxin-heteroresistant carbapenem-resistant Klebsiella pneumoniae; MIC, minimum inhibitory concentration; PMB, polymyxin B; TGC, tigecycline; CZA, ceftazidime/avibactam; MEM, meropenem; IPM, imipenem; CMS, colistin methanesulfonate
Genetic and phenotypic characteristics of CRKP isolates among the PHR-CRKP patients
Table S3 presents the genetic and phenotypic characteristics of the paired isogenic isolates collected before and after the exhibition of polymyxin resistance in the eight patients. Most CRKP strains were of the ST11 type and carried the blaKPC−2 gene, with the exception of patient E, whose strains belonged to ST307 and carried the blaOXA−48 gene. Among the five patients with positive hypervirulent biomarkers, patient D showed the highest pathogenic potential, as indicated by the presence of virulence genes, including rmpA, rmpA2, iucA, and peg-344. Notably, none of the strains tested positive for the mcr-1 gene.
In vivo resistance evolution under polymyxin pressure at subpopulation level
The PAP test revealed an elevated frequency of resistant subpopulations in each patient during the polymyxin treatment (Fig. 3). Among all PHR-CRKP strains, the frequencies of resistance ranged from 2.02 × 10–5 to 2 × 10–7. Importantly, the frequencies significantly decreased in KPB4 and became undetectable in KPA7 after discontinuing polymyxins. To investigate the dynamic changes in subpopulations within PHR isolates, we collected three PHR isolates (KPA2, KPB1, KPC1) from patients A, B with retrieved susceptibility after discontinuing polymyxins and C with remained resistance. Notably, the time-killing studies demonstrated that the major intermediate population were initially eliminated, whereas the resistant subpopulations survived and rapidly regrew as early as 2 h, even at concentrations of 64× MIC in KPA2 and KPC1 (Fig. 4). After the 50th passage in an antibiotic-free medium, the MICs of resistant clones in KPA2 and KPC1 decreased, indicating the instability of the resistance phenotype. Additionally, competition assays were performed among strains obtained from patients A, B, and C to assess the fitness cost of the resistant subpopulations in the absence of antibiotics. The resistant subpopulations were outcompeted by the major intermediate population isolated from the original CRKP, with competition indices ranging from 0.22 to 0.43, indicating the fitness cost of resistant subpopulations in combination of culture (Figure S2).
PAP confirmation of polymyxin heteroresistance in the eight patients. As a negative control, Pseudomonas aeruginosa ATCC 27,853 was included in the study. Abbreviations: PAP, population analysis profile; PI-CRKP, polymyxin-intermediated carbapenem-resistant Klebsiella pneumoniae; CFU, colony-forming unit
The time–killing curve of PMB against PHR-CRKP from patient A, B, and C, respectively. Each sample was measured in triplicate. The three isolates used for the time-kill analysis corresponded to the strains utilized in the competition assays depicted in Figure S2. Abbreviations: MIC, minimum inhibitory concentration; CFU, colony-forming unit; PMB, polymyxin B; CRKP, carbapenem-resistant Klebsiella pneumoniae
Dynamic changes of resistance canonical gene mutations in dominant resistant subpopulations during PHR-CRKP evolution
Among the PHR-CRKP isolates, variants were detected only in pmrB (Gly256Arg, Ala246Thr) of KPB1, with no concurrent mutations found in other amplified genes. These non-synonymous mutations do not contribute to polymyxin resistance [29]. During the evolution process, diverse variations were observed in sequent predominate PR-CRKP strains. The most prevalent mutation among the seven canonical genes was an insertion in mgrB (Table 1). Thirteen PRKP strains isolated from patients B, C, G, and H exhibited three different insertion sequence (IS) elements (ISkpn26-like, IS903B-like, ISkpn14) that were identified in mgrB. Several deleterious mutations (such as pmrBLeu82Arg, pmrBSer85Arg, phoPAsp191Ala) were first detected during PHR-CRKP evolution. All strains carried the wild-type pmrA and phoQ genes, whereas crrA and crrB were lacked in ST11 stains [30]. No variations were identified in the key resistance genes of the remaining four PRKP isolates (KPA3, KPG3B, KPG4A, KPG6B). In patient C, IS903B-like elements were inserted at various locations of mgrB during polymyxin treatment. In patient G, mgrB was disrupted by IS903B-like and ISkpn14 at different positions in serial isolates, along with diverse mutations (Thr157Pro, Leu82Arg, and Ser85Arg) in pmrB, resulting in variable MICs (Table 1). In patient D, the PRKP strain KPD4 harbored two rarely described mutations, pmrBSer203Pro and phoPAsp191Ala, and qRT-PCR analysis revealed significantly increased expression of both genes (Figure S3). In patient E, both crrA and crrB were amplified in the two ST307 strains, with KPE4 carrying a Pro151Ser mutation in crrB compared with KPE1, which also contributes to polymyxin resistance [30, 31].
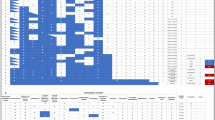
Variability of polymyxin-resistant canonical genes within different sequence types in the broader genetic context of carbapenemase-producing Klebsiella pneumoniae
A comprehensive analysis was performed on 713 genome sequences of carbapenemase-producing K. pneumoniae (CPKP) obtained from the NCBI database (Fig. 5, Table S4). The most common sequence types (STs) were ST11 (26.65%) and ST258 (19.07%). The predominant carbapenemase genes were blaKPC (61.15%) and blaOXA (23.56%). Only a small proportion (0.98%) of the isolates harbored mcr genes.
Variations within the analysed dataset included IS insertions, non-synonymous mutations, lack, and splicing mutations. Insertion sequences were primarily observed in mgrB (76.47%) (Table S5). In total, 1035 non-synonymous mutations, encompassing both deleterious and neutral mutations, were identified across seven genes (Table S6). The pmrB gene exhibited the highest number of mutations (43.96%), followed by crrB (30.34%). Gene lacking were primarily observed in crrA (49.51%) and crrB (33.66%). Detailed analysis revealed splicing mutations in crrC (nt321) and crrB (nt741) in 110 KPC-producing ST11 isolates, which led to the lack of crrA. Notably, 100 of these ST11 isolates were obtained from China. The frequency of crrAB lacking or splicing mutation was nearly 100% in specific STs, including ST231 and ST23, and was higher in ST11 (73.6%) compared with ST258 (30.15%).Within the analyzed dataset, 84 (11.78%) isolates displayed previously reported deleterious mutations associated with polymyxin heteroresistance and resistance. These mutations included IS insertions (n = 39) and lack (n = 4) in mgrB and non-synonymous mutations (n = 42) in seven genes (Table S6). Deleterious non-synonymous mutations were mainly observed in pmrB, pmrA, and mgrB.
Summary of variants in seven polymyxin-resistant canonical genes in 713 carbapenemase-producing Klebsiella pneumoniae. The reference control used was the ST258 and PI-CRKP (KPC-2 producing) ATCC BAA-1705 (GenBank accession number NZ_AOGQ00000000.1). Each branch in the figure represents a CPKP strain, with different STs labeled using different colors. Triangles are used to represent carbapenemase and mcr genes. Abbreviations: CPKP, carbapenemase-producing Klebsiella pneumoniae; NCBI, National Center for Biotechnology Information; WT, wild type; SNV, single-nucleotide variant; IS, insertion sequence; ST, sequence type
Discussion
Currently, the clinical effectiveness and potential adverse effects of polymyxins have prompted us to reevaluate their appropriate application in the treatment of carbapenem-resistant Gram-negative bacteria (CR-GNB) [28]. Concerns regarding both the resistance and heteroresistance to polymyxins merit substantial clinical attention [5, 7]. Our study emphasizes the high prevalence of undetected PHR and its potential clinical significance, particularly in the development of resistant and refractory CRKP infections. Our study revealed that 69.7% of CRKP isolates exhibited heteroresistance, a finding consistent with those of previous studies in China but significantly higher than the 8.4% reported in the United States [5, 8, 9, 11, 17]. This discrepancy suggests that the varying incidences of heteroresistance may be influenced by the genetic diversity of pathogens in different regions. Although the risk factors for heteroresistance remain unclear, it is evident from our study that a significant number of PHR cases can manifest in patients without prior polymyxin exposure [5, 17]. This may be associated with cross-resistance due to environmental factors [15]. These findings highlight the limitations of relying solely on MICs to determine susceptibility and ignoring the phenomenon of PHR [8, 13]. Developing universally applicable methods for rapid PHR detection within regions of high endemicity are imperative [7].
Despite the recognition of heteroresistance, few studies have explored the dynamic evolution of in-host resistance and its effects on treatment failure in clinical settings [5, 7]. HR can serve as a transitional stage leading to the emergence of resistance [32]. Notably, we observed the recoverment of resistance in 38.1% of patients with PHR-CRKP following polymyxin treatment, consistent with the recent study by Xiao et al. [5]. Our study is the first to report eight sepsis cases of the dynamic selection of PR strains from a PHR-CRKP isolate under polymyxin treatment. PR emerged rapidly in these patients, with a median time of 11 days. Previous studies have suggested combining colistin with tetracyclines or aminoglycosides as an effective approach to suppress the selection of resistant subpopulations and have demonstrated synergistic effects against PHR infections in vitro [9, 19]. However, although our patients received combination therapy at appropriate doses, the PHR-CRKP strains quickly progressed to PR-CRKP, resulting in the failure of polymyxin-based treatment, and the prognosis remained refractory despite remedial combination treatments [3]. Recent guidelines have replaced polymyxins with alternative formulations, such as novel enzyme inhibitor complexes, for carbapenem-resistant Enterobacteriaceae because of their improved clinical efficacy [33]. Nevertheless, polymyxin-based combination strategies continue to play a pivotal role in specific scenarios, such as managing multiple coinfections involving CR-GNB or when the choice of active agents is restricted [34]. Therefore, the challenges posed by the heterogeneity and dynamic resistance require careful clinical consideration. Whether attributable to inadequate dosing or other factors, the presence of heteroresistance should be considered when observing a poor response to polymyxin therapy, prompting a timely reassessment of therapeutic strategies. Prospective studies are required to confirm the true scale and clinical effects of bedside polymyxin heteroresistance. Further studies are warranted to determine the optimal antibiotic combination for combating PI-CRKP and mitigating the emergence of resistance in vivo [11].
We investigated the frequencies, resistance levels, and stability of resistant subpopulations during the dynamic evolution of PHR-CRKP at the subpopulation level. In the initial PHR-CRKP strains, we observed rapid regrowth of low-frequency resistant subpopulations with high MICs, indicating their potential role in resistance recoverment and treatment failure. Our PAP test on serial isogenic strains confirmed the increasing frequency of resistant subpopulations during in vivo resistance evolution under polymyxin treatment, which is consistent with the findings in animal models by Band et al. [18]. These results suggest that although adequate doses of polymyxins are recommended, this approach may inadvertently induce adaptive resistance and promote the propagation of resistant subpopulations [35]. Hence, even in combination therapies, it is crucial to remain vigilant regarding the issue of heteroresistance and continuously monitor the clinical treatment response to polymyxins. Interestingly, in vitro experiments have shown that the resistant subpopulations are consistently outcompeted by the isogenic major intermediate population in antibiotic-free media [25]. Additionally, we observed the emergence of intermediate revertants with reduced or undetectable resistant subpopulations in two patients after discontinuing polymyxins. However, further studies are required to determine the feasibility of reusing polymyxins under these conditions. Previous studies have described the mechanisms of HR instability, including high fitness costs associated with genetically stable mutations, which can lead to the generation of compensatory mutations with reduced resistance [18].
Previous studies have indicated the coexistence of different subpopulations within the same parental PHR isolate [36]. However, mechanisms governing the predominance of specific subpopulations in patients undergoing polymyxin treatment remain unclear.The adaptation of PHR-CRKP to polymyxin pressure involves multiple evolutionary pathways and the simultaneous activation of various two-component systems, leading to a dynamic process with reversible susceptibility and unstable genetic mutations in seven canonical resistance genes [19]. Our findings highlight the significant roles of mgrB insertion, pmrB hypermutation, and phoP upregulation in polymyxin heteroresistance and resistance, suggesting the possibility of predominant evolutionary phenotypes under antibiotic selection. Consistent with previous studies, polymyxin exposure can trigger the mobilization of IS1 and IS5 elements in mgrB, generating genetic diversity in K. pneumoniae and contributing to adaptive resistance evolution [12, 17, 37]. pmrB’s inherent hypermutability plays a crucial role in the evolution of polymyxin heteroresistance evolution [36]. In our study, pmrBThr157Pro is a commonly confirmed mechanism associated with polymyxin heteroresistance and resistance [5, 12, 16, 38]. pmrBLeu82Arg and pmrBSer85Arg were first identified during PHR evolution in our study and can activate the PmrAB system and modify lipopolysaccharide even in the absence of physiological signals [39]. We also discovered a rare pmrBSer203Pro mutation that was only present in a resistant subpopulation of patients without prior polymyxin exposure [15]. Additionally, the coexistence of pmrBSer203Pro and a previously described phoPAsp191Ala mutation was observed, and their contributions still need further experimental confirmation in KPD4 during PHR evolution [15, 40].
Finally, we analyzed 713 CPKP isolates from the NCBI database to explore the potential relationship between genetic background and polymyxin heteroresistance and resistance. Our results confirmed that mgrB insertion was a common mechanism of PR across various genetic backgrounds [41]. We identified specific insertion hotspots for the IS5-like family at nt 69–75 in mgrB, including ISkpn26-like and IS903B-like elements (Table S5) [5]. Additionally, IS insertions in mgrB may be transposed from plasmids into the chromosomal canonical region, increasing the threat of polymyxin heteroresistance and polymyxin resistance, and disruption of mgrB can avoid host defences and promote virulence, thereby increasing the risk of treatment failure [42, 43]. Compared with phoPQ, we observed a higher frequency of mutations in the pmrAB genes conferring resistance. Notably, the pmrBT157P mutation was frequently detected and exhibited a polyphyletic distribution, suggesting its predominant role in conferring resistance, which aligns with the evolutionary progression of PHR-CRKP observed in our patients. Previous studies have suggested that crrBAC-kexD cluster has been proposed to loss and re-acquired repeatly through homologous recombination in K. pneumoniae complex or from other bacterial species [30, 44]. We also observed the lack of the crrAB region in several STs, including a specific deletion involving crrA and a part of crrB that was commonly found in ST11 isolates, particularly those from China. Besides the contribution to mechanism of polymyxin heteroresistance and resistance, the role of these genes in bacterial physiology required further studies [30]. Overall, our findings highlight the diverse mutational landscape of genes associated with polymyxin heteroresistance or resistance in CRKP across different STs and genetic backgrounds.
Our study has some limitations. Firstly, it was conducted at a single center, resulting in a small sample size. Secondly, we only studied the canonical colistin resistance genes and not the complete genomes of the isolates recovered from the patient. Further studies of representative resistant subpopulations in intermediate phenotypic isolates are needed, such as whole-genome sequencing [45].Finally, we were unable to assess the relationship between the genetic background and polymyxin susceptibility in our analysis of the genetic database because of the absence of susceptibility data.
Conclusions
Our study revealed the substantial prevalence of PHR in CRKP, even among patients without prior polymyxin exposure. We present a high likelihood of within-host transition from PHR to PR during polymyxin treatment in critically ill patients. Polymyxin heteroresistance significantly increases the risk of resistance exhibition and treatment failure even in the presence of appropriate polymyxin application. Therefore, it is crucial to consistently monitor and closely evaluate the treatment outcomes of polymyxins in the appropriate clinical context for CR-GNB infections.
Data availability
No datasets were generated or analysed during the current study.
References
Tacconelli E, Carrara E, Savoldi A, et al. Discovery, research, and development of new antibiotics: the WHO priority list of antibiotic-resistant bacteria and tuberculosis. Lancet Infect Dis. 2018;18(3):318–27.
Li J, Nation RL, Turnidge JD, et al. Colistin: the re-emerging antibiotic for multidrug-resistant Gram-negative bacterial infections. Lancet Infect Dis. 2006;6(9):589–601.
Liu S, Wu Y, Qi S, et al. Polymyxin B therapy based on therapeutic drug monitoring in carbapenem-resistant organisms sepsis: the PMB-CROS randomized clinical trial. Crit Care. 2023;27(1):232.
Tamma PD, Aitken SL, Bonomo RA, Mathers AJ, van Duin D, Clancy CJ. Infectious Diseases Society of America 2022 Guidance on the treatment of extended-spectrum β-lactamase Producing enterobacterales (ESBL-E), Carbapenem-Resistant Enterobacterales (CRE), and Pseudomonas aeruginosa with difficult-to-treat Resistance (DTR-P. aeruginosa). Clin Infect Dis 2022: 187–212.
Luo Q, Xu L, Wang Y, et al. Clinical relevance, mechanisms, and evolution of polymyxin B heteroresistance carbapenem-resistant Klebsiella pneumoniae: a genomic, retrospective cohort study. Clin Microbiol Infect. 2024;30(4):507–14.
Andersson DI, Nicoloff H, Hjort K. Mechanisms and clinical relevance of bacterial heteroresistance. Nat Rev Microbiol. 2019;17(8):479–96.
Roch M, Sierra R, Andrey DO. Antibiotic heteroresistance in ESKAPE pathogens, from bench to bedside. Clin Microbiol Infect. 2023;29(3):320–5.
Band VI, Satola SW, Smith RD, et al. Colistin Heteroresistance is largely undetected among Carbapenem-Resistant in the United States. mBio. 2021;12(1):e02881.
Tian Y, Zhang Q, Wen L, Chen J. Combined effect of Polymyxin B and Tigecycline to overcome Heteroresistance in Carbapenem-resistant Klebsiella pneumoniae. Microbiol Spectr. 2021;9(2):e0015221.
Weng Y, Wang T, Huang B et al. Multicenter Study of Colistin Heteroresistance in Carbapenem-resistant Klebsiella pneumoniae strains in China. Microbiol Spectr 2023: e0221822.
Wang Y, Ma X, Zhao L, et al. Heteroresistance is Associated with in vitro Regrowth during Colistin Treatment in Carbapenem-resistant Klebsiella pneumoniae. Front Microbiol. 2022;13:868991.
Braspenning A, Rajakani SG, Sey A et al. Assessment of Colistin Heteroresistance among Multidrug-resistant Klebsiella pneumoniae isolated from Intensive Care patients in Europe. Antibiot (Basel) 2024; 13(3).
Ozturk T, Weiss DS. Heteroresistance is a cause of discrepant antibiotic susceptibility testing results. The Lancet Microbe; 2024.
Hawley JS, Murray CK, Jorgensen JH. Colistin heteroresistance in acinetobacter and its association with previous colistin therapy. Antimicrob Agents Chemother. 2008;52(1):351–2.
Sato T, Wada T, Nishijima S, et al. Emergence of the Novel Aminoglycoside acetyltransferase variant aac(6’)-Ib-D179Y and Acquisition of Colistin Heteroresistance in Carbapenem-resistant Klebsiella pneumoniae due to a disrupting mutation in the DNA repair enzyme MutS. mBio. 2020;11(6):e01954.
Seo J, Wi YM, Kim JM, Kim YJ, Ko KS. Detection of colistin-resistant populations prior to antibiotic exposure in KPC-2-producing Klebsiella pneumoniae clinical isolates. J Microbiol. 2021;59(6):590–7.
Lin JY, Zhu ZC, Zhu J, Chen L, Du H. Antibiotic heteroresistance in Klebsiella pneumoniae: definition, detection methods, mechanisms, and combination therapy. Microbiol Res. 2024;283:127701.
Band VI, Crispell EK, Napier BA, et al. Antibiotic failure mediated by a resistant subpopulation in Enterobacter cloacae. Nat Microbiol. 2016;1(6):16053.
Cheong HS, Kim SY, Wi YM, Peck KR, Ko KS. Colistin Heteroresistance in Klebsiella Pneumoniae isolates and diverse mutations of PmrAB and PhoPQ in resistant subpopulations. J Clin Med. 2019;8(9):1444.
Halaby T, Kucukkose E, Janssen AB, et al. Genomic characterization of Colistin Heteroresistance in Klebsiella pneumoniae during a nosocomial outbreak. Antimicrob Agents Chemother. 2016;60(11):6837–43.
Sánchez MB, Sánchez-Gorostiaga A, Cuesta T, Martínez JL. The Acquisition of Colistin Resistance is Associated to the amplification of a large chromosomal region in Klebsiella pneumoniae kp52145. Int J Mol Sci. 2021;22(2):649.
Nakasone I, Kinjo T, Yamane N, Kisanuki K, Shiohira CM. Laboratory-based evaluation of the colorimetric VITEK-2 Compact system for species identification and of the Advanced Expert System for detection of antimicrobial resistances: VITEK-2 Compact system identification and antimicrobial susceptibility testing. Diagn Microbiol Infect Dis. 2007;58(2):191–8.
CLSI. Performance Standards for Antimicrobial Susceptibility Testing. 30th ed. CLSI supplement M100. Clinical and Laboratory Standards Institute 2020; Wanyne, PA.
Li J, Rayner CR, Nation RL, et al. Heteroresistance to colistin in multidrug-resistant Acinetobacter baumannii. Antimicrob Agents Chemother. 2006;50(9):2946–50.
Wang Y, Chen T, Chi X et al. Clinical, biological, and genome-wide comparison of carbapenem-resistant Klebsiella pneumoniae with susceptibility transformation to polymyxin B during therapy. Clin Microbiol Infect 2023.
Hafza N, Challita C, Dandachi I, Bousaab M, Dahdouh E, Daoud Z. Competition assays between ESBL-producing E. Coli and K. pneumoniae isolates collected from Lebanese elderly: an additional cost on fitness. J Infect Public Health. 2018;11(3):393–7.
Schmittgen TD, Livak KJ. Analyzing real-time PCR data by the comparative C(T) method. Nat Protoc. 2008;3(6):1101–8.
Tsuji BT, Pogue JM, Zavascki AP, et al. International Consensus guidelines for the optimal use of the polymyxins: endorsed by the American College of Clinical Pharmacy (ACCP), European Society of Clinical Microbiology and Infectious diseases (ESCMID), Infectious Diseases Society of America (IDSA), International Society for anti-infective pharmacology (ISAP), society of critical Care Medicine (SCCM), and Society of Infectious diseases pharmacists (SIDP). Pharmacotherapy. 2019;39(1):10–39.
Cheng Y-H, Lin T-L, Pan Y-J, Wang Y-P, Lin Y-T, Wang J-T. Colistin resistance mechanisms in Klebsiella pneumoniae strains from Taiwan. Antimicrob Agents Chemother. 2015;59(5):2909–13.
Kim SJ, Cho H, Ko KS. Comparative analysis of the colistin resistance-regulating gene cluster in Klebsiella species. J Microbiol. 2022;60(5):461–8.
Cheng Y-H, Lin T-L, Lin Y-T, Wang J-T. Amino acid substitutions of CrrB responsible for resistance to Colistin through CrrC in Klebsiella pneumoniae. Antimicrob Agents Chemother. 2016;60(6):3709–16.
Band VI, Weiss DS. Heteroresistance to beta-lactam antibiotics may often be a stage in the progression to antibiotic resistance. PLoS Biol. 2021;19(7):e3001346.
Tamma PD, Aitken SL, Bonomo RA, Mathers AJ, van Duin D, Clancy CJ. Infectious Diseases Society of America 2023 Guidance on the treatment of Antimicrobial resistant gram-negative infections. Clin Infect Dis; 2023.
Tiseo G, Brigante G, Giacobbe DR et al. Diagnosis and management of infections caused by multidrug-resistant bacteria: guideline endorsed by the Italian Society of Infection and Tropical Diseases (SIMIT), the Italian society of anti-infective therapy (SITA), the Italian Group for Antimicrobial Stewardship (GISA), the Italian Association of Clinical microbiologists (AMCLI) and the Italian Society of Microbiology (SIM). Int J Antimicrob Agents 2022: 106611.
Meletiadis J, Paranos P, Tsala M, Pournaras S, Vourli S. Pharmacodynamics of colistin resistance in carbapenemase-producing Klebsiella pneumoniae: the double-edged sword of heteroresistance and adaptive resistance. J Med Microbiol 2022; 71(10).
Kapel N, Caballero JD, MacLean RC. Localized pmrB hypermutation drives the evolution of colistin heteroresistance. Cell Rep. 2022;39(10):110929.
Yang TY, Wang SF, Lin JE, et al. Contributions of insertion sequences conferring colistin resistance in Klebsiella pneumoniae. Int J Antimicrob Agents. 2020;55(3):105894.
Olaitan AO, Diene SM, Kempf M, et al. Worldwide emergence of colistin resistance in Klebsiella pneumoniae from healthy humans and patients in Lao PDR, Thailand, Israel, Nigeria and France owing to inactivation of the PhoP/PhoQ regulator mgrB: an epidemiological and molecular study. Int J Antimicrob Agents. 2014;44(6):500–7.
Cannatelli A, Di Pilato V, Giani T, et al. In vivo evolution to colistin resistance by PmrB sensor kinase mutation in KPC-producing Klebsiella pneumoniae is associated with low-dosage colistin treatment. Antimicrob Agents Chemother. 2014;58(8):4399–403.
Li Z, Liu X, Lei Z et al. Genetic diversity of polymyxin-resistance mechanisms in clinical isolates of Carbapenem-resistant Klebsiella pneumoniae: a Multicenter Study in China. Microbiol Spectr 2023: e0523122.
Hu H, Shi Q, Zhang P, et al. Prevalence and molecular characteristics of colistin-resistant isolates among clinically isolated carbapenem-resistant Klebsiella pneumoniae in China. Int J Antimicrob Agents. 2023;62(2):106873.
Kidd TJ, Mills G, Sá-Pessoa J, et al. A Klebsiella pneumoniae antibiotic resistance mechanism that subdues host defences and promotes virulence. EMBO Mol Med. 2017;9(4):430–47.
Antonelli A, D’Andrea MM, Giani T, Rossolini GM. Plasmid-mediated or chromosomally mediated colistin resistance in Klebsiella pneumoniae? Lancet Infect Dis. 2017;17(1):26–7.
Cain AK, Boinett CJ, Barquist L, et al. Morphological, genomic and transcriptomic responses of Klebsiella pneumoniae to the last-line antibiotic colistin. Sci Rep. 2018;8(1):9868.
Janssen AB, Doorduijn DJ, Mills G et al. Evolution of Colistin Resistance in the Klebsiella pneumoniae Complex follows multiple evolutionary trajectories with Variable effects on Fitness and virulence characteristics. Antimicrob Agents Chemother 2020; 65(1).
Acknowledgements
The graphical abstract was generated with the support of Biorender (www.biorender.com).
Funding
This study was supported by National Natural Science Foundation of China (grant 82272372 to Jingyong Sun), Science and Technology Commission of Shanghai Municipality (grant 20Y11901100 to Hongping Qu), Clinical science and technology innovation project of SHCD (grant SHDC22021212 to Hongping Qu) and Guangci discipline group construction of public health and disaster emergency center (grant XKQ-09 to Hongping Qu).
Author information
Authors and Affiliations
Contributions
HPQ, RMT, and TTP conceived and supervised the study. XLW, TJM, and YQD collected the clinical isolates and data, analyzed, and wrote the manuscript. HYO and JYS provided technical support and experimental instruments. MW and BT contributed to the data analysis and figure preparation. DCC conducted the experiments and revised the manuscript. All authors reviewed and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Wang, X., Meng, T., Dai, Y. et al. High prevalence of polymyxin-heteroresistant carbapenem-resistant Klebsiella pneumoniae and its within-host evolution to resistance among critically ill scenarios. Infection (2024). https://doi.org/10.1007/s15010-024-02365-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s15010-024-02365-z